Brugada Syndrome criteria
Brugada Syndrome is an autosomal dominant transmitted condition with male predominance (8:1) that results in high risk of sudden cardiac death due to ventricular tachyarrhythmia.
- Sudden death can occur anytime from infancy to old age
- Mean age 41 years (SD 15 years)
- Most common in southeast Asia
- Most common cause of non-trauma related death in men 40 years old in countries where it is endemic
- Causes at least 4% of all sudden deaths
- Causes >20% of sudden death in patients with structurally normal hearts
Electrocardiographic findings: 
- Types 1, 2, and 3 all require that more than 1 of the right precordial leads (V1-V3) have the abnormality described for each type
- May be associated with complete or incomplete right bundle branch block
- 1st degree AV block common (PR=200 ms)
- Type 1 (Diagnostic of Brugada Syndrome)
- ST segment: Coved shape, elevation =2 mm
- Terminal aspect of ST segment: Gradually descending
- T wave: Negative
- Meets criteria of Type 1 in the presence or absence of a sodium channel-blocking drug
- Type 2 (Suggestive of Brugada Syndrome)
- ST segment: Saddleback shape, elevation =2 mm with a high takeoff ST-segment, with the trough displaying =1 mm ST segment elevation
- T wave: Positive or biphasic
- Type 3 (Suggestive of Brugada Syndrome)
- Has either a coved or saddleback appearance (like Type I or Type II) but the ST segment elevation is 1 mm
- If Type 1 EKG, only needs the addition of 1 or more of the “Clinical Criteria” to make diagnosis of Brugada Syndrome
- If Type 2 or 3 EKG, if this converts to a Type 1 EKG with sodium channel blocker administration and 1 or more of the “Clinical Criteria” is present, diagnosis of Brugada Syndrome is made
- If Type 3 EKG converts to Type 2 EKG; this is inconclusive for the diagnosis of Brugada Syndrome
- “Clinical Criteria”
- Documented ventricular fibrillation or polymorphic ventricular tachycardia
- Family history of sudden cardiac death in someone 45 years old
- Coved-type EKGs in family members
- Inducible VT with programmed electrical stimulation
- Syncope
- Nocturnal agonal respiration
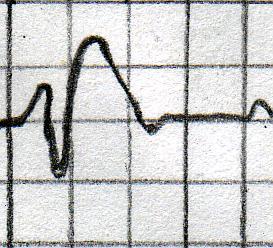
Type 1 EKG morphology example: 
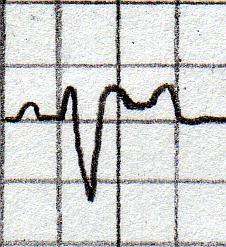
Type 2 EKG morphology example: 
The EKG findings of Brugada syndrome are often dynamic and may be concealed until unmasked by either a drug or other medical condition such as: 
- Alcohol toxicity
- Alpha adrenergic agonists
- Beta adrenergic blockers
- Cocaine toxicity
- Fever
- Hyperkalemia
- Hypercalcemia
- Hypokalemia
- Insulin and Glucose administration
- Sodium channel blockers (ajmaline, flecainide, pilsicainide, procainamide)
- Tricyclic or Tetracyclic antidepressants
- Vagotonic drugs
The only proven effective therapy for Brugada syndrome is placement of an Implanted Cardiac Defibrillator (ICD). Patients with Type 1, 2, or 3 findings on EKG without any of the additional “Clinical Criteria” require further evaluation to determine whether or not they have Brugada Syndrome and require ICD placement.
Alings M, Wilde A. “Brugada” syndrome: clinical data and suggested pathophysiological mechanism. Circulation. 1999 Feb 9;99(5):666-73.
Antzelevitch C, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005 Feb 8;111(5):659-70.
Brugada J, et al. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003 Dec 23;108(25):3092-6.
Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992 Nov 15;20(6):1391-6.
Wilde AA, et al. Proposed Diagnostic Criteria for the Brugada syndrome. Circulation. 2002 Nov 5;106(19)2514-9.
- Information
- Facts about Brugada Syndrome
- Electrocardiographic findings
- Additional Criteria
- Type 1 EKG morphology example
- Type 2 EKG morphology example
- The EKG findings of Brugada syndrome are often dynamic and may be concealed until unmasked by either a drug or other medical condition such as
- Treatment
- References