COMMUNICATION AND PATIENT SAFETY
Successful encounters with patients begin with a professional, respectful, and compassionate approach.
- Positive communications should begin by addressing the patient using proper titles such as Ms., Mrs., or Mr.; the inappropriate use of terms of endearment is a common patient complaint.
- Health-care providers (HCPs) should always introduce and identify themselves to the patient before explaining the upcoming laboratory or diagnostic study. An example is to say, “Good morning. My name is Lilli and I will be your nurse today.”
- Always conclude the conversation by asking if there are any questions before leaving the room.
- If you have a concern about a patient’s level of understanding with the conversation, ask the individual to repeat what you have just explained so you can confirm that there are no issues.
Teach the patient what to expect.
Statement of the purpose of the study.
- The level of detail provided to patients about the test purpose depends on numerous factors and should be individualized appropriately in each setting. After the introduction, explain in easily understandable age-, culture-, and gender-appropriate terms about the study that is to be performed. Ask the patient to discuss their health concerns to give you a sense of how to begin the discussion. General information to communicate should include study type (e.g., blood, x-ray, magnetic resonance imaging [MRI], urine, etc.) and the purpose or common use of the test (e.g., to assist in the diagnosis of diabetes, to assess the function of the kidneys, to identify the presence of findings that would either confirm a condition or confirm the absence of a health problem).
Description of the procedure and associated safety practices.
- Describe the procedure, what part of the body will be evaluated, whether or not the procedure is invasive, where the procedure will take place, and who will participate in performing the study.
- It is a good idea to explain to the patient that gloves will be worn by the health-care providers (HCPs) throughout the procedure. Many institutions require hand washing at the beginning and end of each specimen collection encounter and between each patient. This explanation should help the patient understand that the use of gloves is standard practice established for everyone’s safety and protection.
- Inquire about and document the patient’s known allergies.
- Explain that it is essential the patient be positively and properly identified at every encounter before care, treatment, or services are provided. Patients may become concerned that they are asked to repeat their personal identification information. They may misinterpret this safety practice as incompetence, lack of communication, or lack of interest.
- Typically, two patient-specific identifiers are used and may vary between inpatient and outpatient areas. Chosen identifiers may include full name, medical record number, or date of birth.
Addressing the need for informed consent.
- Some procedures may require informed, written consent as described in the facility’s policy and procedure manual. What does informed (written) consent mean? Who is responsible for obtaining a consent?
- The exact definition and implementation of informed consent vary among states and individual health-care facilities in the United States. Best practices suggest a team approach. However, the concept of informed consent is generally based on the underlying moral and legal premises of patient autonomy found in a health-care facility’s Bill of Patient’s Rights and specific clinical policies. The U.S. Department of Health and Human Services describes informed consent to mean that if treatment is needed, the requesting HCP must provide that individual with the information needed to make the decision to agree with or decline the specified treatment plan. While many common patient-HCP interactions involve an implied voluntary consent, some specific procedures require informed, written consent. The list of tests and treatments requiring consent varies among facilities and may change with advances in clinical practice and technology. Generally, informed written consent is required for invasive procedures, tests, or treatments with significant risks, benefits, and alternatives. Once the requesting HCP has provided information to the patient, the informed patient’s written consent must then be obtained and documented by the person designated in the facility’s policy. The consent must be signed after the patient has been informed and before the procedure or administration of any medications that would affect the patient's ability to make an important decision. There are a few legal exceptions to obtaining an informed (written) consent. Most commonly, they occur when there is a medical emergency that would result in death if not addressed immediately or in the case of mental incompetence in which an individual is unable to give or refuse consent and there is no surrogate (legal guardian or health-care proxy). Patient assault and patient battery are the legal terms put forth regarding the failure to obtain consent (as required by a facility’s policies) before performing a test or procedure or allowing a deviation from the consented test or procedure to occur (unless an additional consent is appropriately obtained).
- Make sure a written and informed consent has been signed for the requested study and properly documented prior to the procedure and prior to administering any medications and according to your facility’s requirements (Figure A–1).
Description of the sensations, including discomfort and pain, that may be experienced during specimen collection or a diagnostic procedure.
- Address concerns about pain related to the procedure, and suggest breathing or visualization techniques to promote relaxation.
- For pediatric patients, a doll may be used to “show” the procedure.
- Explain that where appropriate, sedative or anesthetizing agents may be used to assist in allaying anxiety the patient may experience related to anticipation of pain associated with the procedure.
- Sedation and anesthesia are used to facilitate the completion of selected studies. Conscious or monitored sedation uses medication to promote relaxation and minimize pain while at the same time allowing the patient to remain conscious enough to communicate with the HCP. This approach is used to prevent pain and injury during a procedure.
- General anesthesia is medication given to cause a type of coma in which the patient is without consciousness or awareness and is protected from experiencing any pain associated with the procedure. However, with this type of sedation, the patient is also left without any protective reflexes.
General instruction regarding pretesting preparations.
- Explain pretesting diet, fluid, medication, or activity instructions and why strict adherence to the instructions is required to obtain accurate results.
- Fasting means no caloric intake for 8 or more hours.
- Failure to follow dietary, fluid, medication, activity, or other restrictions before the blood test or diagnostic procedure may cause the procedure to be canceled or repeated.
The practice of an overnight fast before a laboratory test is a general recommendation.
- Reference ranges are often based on fasting populations to provide some level of standardization for comparison.
- Some test results are dramatically affected by foods, and fasting is a pretest requirement.
- The presence of lipids in the blood also may interfere with the test method; fasting eliminates this potential source of error, especially if the patient already has elevated lipid levels.
- The laboratory should always be consulted if there is a question whether fasting is a requirement or a recommendation.
The practice of an overnight fast before a diagnostic test is a general recommendation.
- Dietary restrictions are usually related either to avoiding complications (e.g., aspiration), as with the use of anesthesia or other medications known to cause nausea and vomiting, or to avoiding factors that may alter the results of the study (e.g., undigested food that obscures visualization of the area of interest).
Specific patient preparation instructions and specimen collection techniques vary by site, study required, and level of invasiveness. The following guidelines should be implemented for all studies.
- Orders should be completed accurately and submitted per laboratory or diagnostic procedural policy.
- Positive patient identification extends to all specimens collected from the patient. Specimens should always be labeled, after collection per CLSI standards, with two patient-specific identifiers (e.g., the patient’s name, date of birth, medical record number, or some other unique identifier), date collected, time collected, initials of the person collecting the sample, and laterality, if applicable (e.g., biopsies).
Recognition of anxiety related to test results.
- Provide a compassionate, reassuring environment.
- Encourage the patient to ask questions and verbalize concerns.
- Offer contact information for nationally recognized Web sites.
Results notification.
- Timely notification of a critical finding for laboratory or diagnostic studies is a role expectation of the professional nurse.
- Follow the facility’s procedure for reporting and documenting critical findings.
Pediatric considerations for a laboratory or diagnostic study.
- Preparing children depends on the age of the child. Encourage parents to be truthful about unpleasant sensations (cramping, pressure, pinching, etc.) the child may experience during the procedure and to use words that they know their child will understand. Toddlers and preschool-age children have a very short attention span, so the best time to talk about the test is right before the procedure. The child should be assured that they will be allowed to bring a favorite comfort item into the examination room, and if appropriate, that a parent will be with the child during the procedure.
- Explain to parents and caregivers that special equipment (balloon-tip catheters to assist with retention of barium during a barium enema, foam wedges used to hold a limb in place during a nuclear scan, etc.) may be needed to assist with a successful study.
- Postprocedural recovery interventions, such as achieving adequate hydration, require close attention. The parents or caregivers must receive education to help them address specific needs and to be watchful for indications of a developing problem because pediatric patients cannot do so for themselves.
Older adult considerations for a laboratory or diagnostic study.
- Older adult patients present with a variety of concerns when undergoing diagnostic procedures. Level of cooperation and fall risk may be complicated by underlying problems such as visual and hearing impairment, joint and muscle stiffness, physical weakness, mental confusion, and the effects of medications.
- A fall injury can be avoided by providing assistance getting on and off the examination table and getting on and off the toilet before and at the end of the examination.
- Older adult patients are often chronically dehydrated; anticipating the effects of hypovolemia and orthostasis can also help prevent falls.
- Older patients who are small in size compared to other adults also may receive a higher radiation dose than necessary if settings are not adjusted for their size.
- Special equipment (balloon-tip catheters to assist with retention of barium during a barium enema, foam wedges used to hold a limb in place during a nuclear scan, etc.) may be needed to assist with a successful study.
- Postprocedural recovery interventions, such as achieving adequate hydration, require close attention.
- Many older patients wish to maintain their independence. Their caregivers must receive education to help them address specific needs and to be watchful for indications of a developing problem; the limits of an older adult patient’s physical and intellectual abilities may be an obstacle to independently carrying out the proper postprocedural care.
BLOOD SPECIMENS
Most laboratory tests that require a blood specimen use venous blood. Arterial blood specimens are usually collected for specific tests such as blood gas analysis.
- Venous blood can be collected directly from the vein or by way of capillary puncture.
Venous blood also can be obtained from vascular access devices, such as:- Saline locks
- Central venous (triple-lumen subclavian, implanted venous access port, Groshong) catheters.
- Capillary blood can be obtained from the fingertips or earlobes of adults and small children and from the heels of infants.
The circumstances in which the capillary method is selected over direct venipuncture include cases in which
- The patient has poor veins.
- The patient has small veins.
- The patient has a limited number of available veins.
- The patient has significant anxiety about the venipuncture procedure.
- Fetal blood samples can be obtained, when warranted, by a qualified HCP from the scalp or from the umbilical cord.
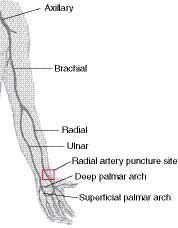
- Arterial blood can be collected from the radial, brachial, or femoral artery if blood gas analysis is requested.
In addition to guidelines presented in previous section, when collecting and handling blood specimens:
- Stress can cause variations in some test results. A sleeping patient should be gently awakened and allowed the opportunity to become oriented before collection site selection.
- Comatose or unconscious patients should be greeted in the same gentle manner because, although they are unable to respond, they may be capable of hearing and understanding.
- Anticipate instances in which patient cooperation may be an issue. Enlist a second person to assist with specimen collection to ensure a safe, quality collection experience for all involved.
- Gloves and any other additional personal protective equipment indicated by the patient’s condition should always be worn during the specimen collection process.
- The facility’s specific standard precautions policy should be consulted for further details.
- Often, several blood specimens are collected together. Ensure the blood specimens are collected in the correct order to protect the integrity of the studies. Always follow your facility’s protocol for order of draw. Generally,
- Blood culture tube (yellow) or bottle.
- Sodium citrate (blue); coagulation studies. Note:
- When using a butterfly and the blue-top tube is the first tube drawn, a nonadditive red-top or coagulation discard tube should be collected first and discarded.
- The amount of blood in the discard tube needs to be sufficient to fill the winged collection set tubing’s “dead space” or fill one-quarter of the discard tube.
- The blue-top tube to be used for testing must be completely filled to ensure the proper ratio of blood to additive in the test specimen blue-top tube.
- Serum—plain, additive, gel (red, SST); most chemistries, drug levels, and serologies.
- Heparin—additive or gel (light or dark green); most chemistries.
- EDTA—additive or gel (lavender, pink, pearl white); hematology blood counts, blood bank, molecular studies.
- Sodium fluoride/potassium oxalate—antiglycolytic inhibitor (gray); glucose studies, tolerance tests.
- Localized activity such as the application of a tourniquet or clenching the hand to assist in visualizing the vein can cause variations in some test results. It is important to be aware of affected studies before specimen collection.
- Hemoconcentration may cause variations in some test results. The tourniquet should never be left in place for longer than 1 min.
- Previous puncture sites should be avoided when accessing a blood vessel by any means to reduce the potential for infection.
- Blood specimens should never be collected above an IV line because of the potential for dilution when the specimen and the IV solution combine in the collection container, falsely decreasing the result. It is also possible that substances in the IV solution could contaminate the specimen and result in falsely elevated test results.
- Changes in posture from supine to erect or long-term maintenance of a supine posture cause variations in some test results. It is important to be aware of this effect when results are interpreted and compared with previous values.
- Collection times for therapeutic drug (peak and trough) or other specific monitoring (e.g., chemotherapy, glucose, insulin, or potassium) should be documented carefully in relation to the time of medication administration. It is essential that this information be communicated clearly and accurately to avoid misunderstanding of the dose time in relation to the collection time. Miscommunication between the individual administering the medication and the individual collecting the specimen is the most frequent cause of subtherapeutic levels, toxic levels, and misleading information used in the calculation of future therapies.
- The laboratory should be consulted regarding minimum specimen collection requirements when multiple tube types or samples are required. Factors that invalidate estimation of blood volume include conditions such as anemia, polycythemia, dehydration, and overhydration.
- The laboratory should be consulted regarding the preferred container/specimen type before sample collection.
- In many cases when a blood sample is required, serum is the specimen type of choice.
- Plasma may be frequently substituted, however. Specimen processing is more rapid for plasma samples than for serum samples because the anticoagulated sample does not need to clot before centrifugation. Plasma samples also require less centrifugation time to achieve adequate separation.
- Consultation regarding collection containers is also important because some laboratory methods are optimized for a specific specimen type (serum versus plasma).
- Preservatives present in collection containers, such as sodium fluoride, may exhibit a chemical interference with test reagents that can cause underestimation or overestimation of measured values.
- Other preservatives, such as EDTA, can block the analyte of interest in the sample (e.g., calcium) from participating in the test reaction, invalidating test results.
- It is possible that some high-throughput, robotic equipment systems require specific and standardized collection containers.
- Prompt and proper specimen processing, storage, and analysis are essential to achieve accurate results. Results that are evaluated outside the entire context of the preparatory, collection, and handling process may be interpreted erroneously if consideration is not given to these general guidelines in addition to the collection guidelines.
- Specimens collected in containers with solid or liquid preservatives or with gel separators should be mixed by inverting the tube 8 to 10 times immediately after the tube has been filled.
- Specimens should be mixed and handled gently to avoid hemolysis.
- Specimens should always be transported to the laboratory as quickly as possible after collection.
- Once the draws are completed, tell the patient that a report of the results will be made available to the requesting HCP, who will discuss the results with the patient.
- Two venipuncture-related concerns that are especially important pertain to the selection of specimen collection materials and the volume of specimen required.
- Iatrogenic anemia is a significant concern for hospitalized infants.
- Anemia from chronic blood sampling can be an issue for older adults who may also suffer malnutrition, dehydration, and diminished hematopoietic system response.
- The use of microtainers allows for specimen collection from capillary sites.
- Many vacuum tubes, including blood culture tubes, are available in pediatric sizes to reduce collection volume.
- Advances in the technology of laboratory equipment have dramatically reduced, to microsamples, the amount of specimen required for testing.
There have been other changes in equipment used specifically to address specimen collection issues in the pediatric and older adult populations.
- The use of butterfly needles or winged infusion sets has become very popular with older adults who believe “they hurt less and are smaller than” conventional needles. This is a patient perception; butterfly and Vacutainer holder needles are available in the same sizes.
- The skin of pediatric and older adult patients is very delicate, and depending on the patient’s preference, there are several methods used to hold the gauze bandage in place after the venipuncture. Many patients cannot even tolerate paper tape that is made with less adhesive.
- Bandage loosely over-wrapped with gauze and held in place by tape, without touching the skin. This approach is safer for pediatric and older adult patients who may forget to remove the self-adhesive wrap in a timely fashion. Excessive tension and compression to the skin can result in unintended injury.
- Self-adhesive wrap that sticks to itself instead of to the skin.
- Bandage or paper tape applied over the gauze and skin.
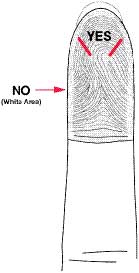
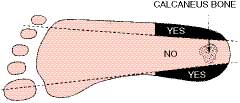
Capillary Puncture: Assess the selected area. It should be free of lesions and calluses, there should be no edema, and the site should feel warm. If the site feels cool or appears pale or cyanotic, warm compresses can be applied over 3 to 5 min to dilate the capillaries. For fingersticks, the central, fleshy, distal portions of the third or fourth fingers are the preferred collection sites (Figure A–2, Capillary puncture of the finger). For neonatal heel sticks, the medial and lateral surfaces of the plantar area are preferred to avoid direct puncture of the heel bone, which could result in osteomyelitis (Figure A–3, Capillary puncture of the heel).
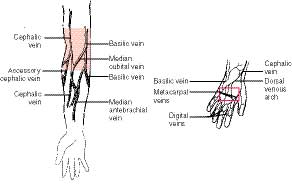
Venipuncture of Arm: Assess the arm for visibly accessible veins. The selected area should not be burned or scarred, have a tattoo, or have hematoma present. Even after the tourniquet is applied, not all patients have a prominent median cubital, cephalic, or basilic vein. Both arms should be observed because some patients have accessible veins in one arm and not the other. The median cubital vein in the antecubital fossa is the preferred venipuncture site. The patient may be able to provide the best information regarding venous access if the patient has had previous venipuncture experience. Alternative techniques to increase visibility of veins may include warming the arm, allowing the arm to dangle downward for a minute or two, tapping the antecubital area with the index finger, or massaging the arm upward from wrist to elbow. The condition of the vein also should be assessed before venipuncture. Sclerotic (hard, scarred) veins or veins in which phlebitis previously occurred should be avoided. Arms with a functioning hemodialysis access site should not be used. The arm on the affected side of a mastectomy should be avoided. In the case of a double mastectomy, the requesting HCP should be consulted before specimen collection.
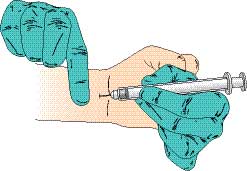
Venipuncture of Hand and Wrist: If no veins in the arms are available, hands and wrists should be examined as described for the arm (Figure A–4, Venipuncture arm/hand). Consideration should be given to the venipuncture equipment selected because the veins in these areas are much smaller. Pediatric-sized collection containers and needles with a larger gauge may be more appropriate.
Venipuncture of Legs and Feet: The veins in the legs and feet can be accessed as with sites located on the arm, hand, or wrist. These extremities should be used only on the approval of the requesting HCP because veins in these locations are more prone to infection and formation of blood clots, especially in patients with diabetes, cardiac disease, and bleeding disorders.
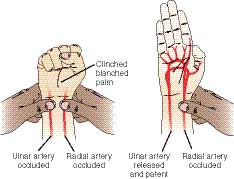
Radial Arterial Puncture: The radial artery is the artery of choice for obtaining arterial blood gas specimens because it is close to the surface of the wrist and does not require a deep puncture (Figure A–5, Arterial arm/hand). Its easy access also allows for more effective compression after the needle has been removed. The nearby ulnar artery can provide sufficient collateral circulation to the hand during specimen collection and postcollection compression. See also Figure A–6, Allen test and Figure A–7, Arterial puncture.
Percutaneous Umbilical Cord Sampling: The blood is aspirated from the umbilical cord under the guidance of ultrasonography and using a 20- or 22-gauge spinal needle inserted through the mother’s abdomen.
Postnatal Umbilical Cord Sampling: The blood is aspirated from the umbilical cord using a 20- or 22-gauge needle and transferred to the appropriate collection container.
Fetal Scalp Sampling: The requesting HCP makes a puncture in the fetal scalp using a microblade, and the specimen is collected in a long capillary tube. The tube is usually capped on both ends immediately after specimen collection.
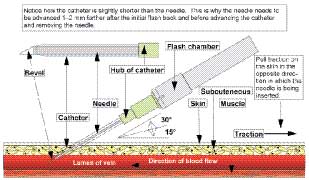
Locks and Catheters: These devices are sometimes inserted to provide a means for the administration of fluids or medications. They are also used to obtain blood specimens without the need for frequent venipuncture (Figure A–8, Starting an IV). The device first should be assessed for patency. The need for saline irrigation or clot removal depends on the type of device in use and the institution-specific or HCP-specific protocols in effect. Use sterile technique because these devices provide direct access to the patient’s bloodstream. When IV fluids are being administered via a device at the time of specimen collection, blood should be obtained from the opposite side of the body. If this is not possible, the flow should be stopped for 5 min before specimen collection. The first 5 mL of blood collected should be discarded.
Complications Associated With Invasive Punctures of the Skin:
- Pain is commonly associated with needles, and although pain experienced during a needle puncture is usually mild, on a rare occasion the needle may strike a nerve, causing severe and lasting pain.
- Hematoma results when blood leaks into the tissue during or after a needle puncture, as evidenced by pain, bruising, and/or swelling at the puncture site. The swelling can cause temporary or permanent injury by compressing the surrounding nerves. Hematomas occur more often in older adults or frail patients or in those with vessels that are difficult to access.
- Prolonged bleeding is a complication that occurs with patients who are taking blood thinners, such as aspirin or warfarin, or who have coagulopathies, such as hemophilia.
- Once the needle has been removed, bleeding or bruising can be prevented by applying direct pressure to the puncture site with gauze for a minute or two. The site should then be observed/assessed for bleeding or bruising. If no further action is required, the site can be covered by the gauze and an adhesive bandage or paper tape.
- Some patients experience a vasovagal reaction during the needle puncture procedure, evidenced by sweating (diaphoresis), low blood pressure (hypotension), fainting (syncope), or near fainting (near syncope). The potential for a fall injury is a significant concern related to vasovagal reactions.
- Other, more unusual complications of needle puncture include cellulitis, phlebitis, seizures, inadvertent arterial puncture during a venipuncture, and sepsis.
- Sepsis can be caused by introduction of bacteria from the surface of the skin into the blood as the result of improper cleansing of the puncture site.
- Immunocompromised patients are at higher risk for developing sepsis as a complication of venipuncture.
- The patient should be informed that improper collection, storage, and transport are the primary reasons for specimen rejection and subsequent requests for recollection. If the specimen is to be collected at home, it should be collected in a clean plastic container (preferably a container from the testing laboratory).
- Many studies require refrigeration after collection.
- If the collection container includes a preservative, the patient should be made aware of the contents and advised as to what the precaution labels mean (caution labels such as “caustic,” “corrosive,” “acid,” and “base” should be affixed to the container as appropriate). When a preservative or fixative is included in the container, the patient should be advised not to remove it.
- The patient also should be told not to void directly into the container. The patient should be given a collection device, if indicated, and instructed to void into the collection device.
- The specimen should be carefully transferred into the collection container. Urinary output should be recorded throughout the collection time if the specimen is being collected over a specified time interval. Some laboratories provide preprinted collection instructions tailored to their methods. The specimen should be transported promptly to the laboratory after collection.
Random: These samples are used mainly for routine screening and can be collected at any time of the day. The patient should be instructed to void either directly into the collection container (if there is no preservative) or into a collection device for transfer into the specimen container.
First Morning: Urine on rising in the morning is very concentrated. These specimens are indicated when screening for substances that may not be detectable in a more dilute random sample. These specimens are also necessary for testing conditions such as orthostatic proteinuria, in which levels vary with changes in posture.
Second Void: In some cases, it is desirable to test freshly produced urine to evaluate the patient’s current status, as with glucose and ketones. Explain to the patient that they should first void and then drink a glass of water. The patient should be instructed to wait 30 min and then void either directly into the collection container or into a collection device for transfer into the collection container.
Clean Catch: These midstream specimens are generally used for microbiological or cytological studies. They also may be requested for routine urinalysis to provide a specimen that is least contaminated with urethral cells, microorganisms, mucus, or other substances that may affect the interpretation of results. Instruct the male patient first to wash hands thoroughly, then cleanse the meatus, void a small amount into the toilet, and void either directly into the specimen container or into a collection device for transfer into the specimen container. Instruct the female patient first to wash hands thoroughly, and then to cleanse the labia from front to back. While keeping the labia separated, the patient should void a small amount into the toilet, and then, without interrupting the urine stream, void either directly into the specimen container or into a collection device for transfer into the specimen container.
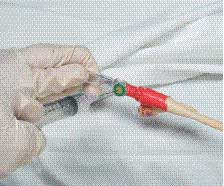
Catheterized Random or Clean Catch: “Straight catheterization” is indicated when the patient is unable to void, when the patient is unable to prepare properly for clean-catch specimen collection, or when the patient has an indwelling catheter in place from which a urine sample may be obtained. Before collecting a specimen from the catheter, observe the drainage tube to ensure that it is empty, and then clamp the tube distal to the collection port 15 min before specimen collection. Cleanse the port with an antiseptic swab such as 70% alcohol and allow the port to dry. Use a needle and syringe (sterile if indicated) to withdraw the required amount of specimen (Figure A–9, Urine collection from an indwelling catheter). Unclamp the tube.
Timed: To quantify substances in urine, 24-hr urine collections are used. They are also used to measure substances whose level of excretion varies over time. The use of preservatives and the handling of specimens during the timed collection may be subject to variability among laboratories. The testing laboratory should be consulted regarding specific instructions before starting the test. Many times, the specimen must be refrigerated or kept on ice throughout the entire collection period. Explain to the patient that it is crucial for all urine to be included in the collection. Urinary output should be recorded throughout the collection time if the specimen is being collected over a specified time interval. The test should begin between 0600 and 0800 if possible. Instruct the patient to collect the first void of the day and discard it. The start time of the collection period begins at the time the first voided specimen was discarded and should be recorded along with the date on the collection container. Urine from all subsequent voidings should be collected and transferred into the collection container. The patient should be instructed to void at the same time the following morning and to add this last voiding to the container. This is the end time of the collection and should be recorded along with the date on the container. For patients who are in the hospital, the urinary output should be compared with the volume measured in the completed collection container. Discrepancies between the two volumes indicate that a collection might have been discarded. A creatinine level often is requested along with the study of interest to evaluate the completeness of the collection.
Catheterized Timed: Instructions for this type of collection are basically the same as those for timed specimen collection. The test should begin by changing the tubing and drainage bag. If a preservative is required, it can be placed directly in the drainage bag, or the specimen can be removed at frequent intervals (every 2 hr) and transferred to the collection container to which the preservative has been added. The drainage bag must be kept on ice or emptied periodically into the collection container during the entire collection period if indicated by the testing laboratory. The tubing should be monitored throughout the collection period to ensure continued drainage.
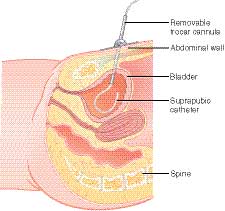
Suprapubic Aspiration: This procedure is performed by inserting a needle directly into the bladder (Figure A–10, Suprapubic aspiration of a urine specimen). Because the bladder is normally sterile, the urine collected should also be free from any contamination caused by the presence of microorganisms. Place the patient in a supine position. Cleanse the area with antiseptic and drape with sterile drapes. A local anesthetic may be administered before insertion of the needle. A needle is inserted through the skin into the bladder. A syringe attached to the needle is used to aspirate the urine sample. The needle is then removed, and a sterile dressing is applied to the site. Place the sterile sample in a sterile specimen container. The site must be observed for signs of inflammation or infection.
Pediatric: Specimen collection can be achieved by any of the previously described methods using collection devices specifically designed for pediatric patients. Appropriately cleanse the genital area and allow the area to dry. For a random collection, remove the covering of the adhesive strips on the collector bag and apply over the genital area (Figure A–11, Pediatric urine collection). Diaper the child. When the specimen is obtained, place the entire collection bag in the specimen container (use a sterile container as appropriate for the requested study). Some laboratories may have specific preferences for the submission of urine specimens for culture. Consult the laboratory before collection to avoid specimen rejection.
DIAGNOSTIC IMAGING TESTS
Imaging technology has exploded since its introduction in the early 1900s. The four most commonly used imaging modalities include radiography, nuclear medicine, magnetic resonance imaging (MRI), and ultrasound (US). The current menu of diagnostic studies can quickly become confusing, especially since some involve radiation and some do not, imaging using combined modalities is becoming more common, and most modalities can be ordered either with or without contrast.
- Radiography—detection of x-ray emissions generated by external exposure to radiation-emitting equipment
- Nuclear medicine—detection of gamma ray emissions generated from radioisotopes administered internally to the patient
- MRI—detection of radio waves generated by external exposure to a magnetic field
- US—detection of sound waves generated by a transducer, applied externally to the skin
| ||||||||||||||||||||||||||||||||||||||||||
Contrast medium is used to enhance the radio-density or radio-opaqueness of the target site. It does this by blocking the x-ray or radio wave emissions from passing through anatomical areas of various densities. Radiolucency refers to greater passage of x-ray or radio wave emissions through various densities. The opacity of an area being visualized is determined both by its density and also by the chemical properties of the elements of which it is made. Bone is the densest tissue in the body and contains a lot of calcium. Calcium has a relatively high atomic number (protons). As an example, of the common elements that make up the solids and liquids in our body, the atomic number of calcium is 20, oxygen is 8, carbon is 6, and hydrogen is 1. It is not a coincidence that materials used as contrast agents in diagnostic imaging have relatively high atomic numbers compared to the elements that comprise our body fluids and tissues; for example, iodine is 53, barium is 56, gallium is 31.
| ||||||||||||||||||||
Radiography
Radiography is a general term to describe types of studies that use x-ray emissions to look inside the body. This technology is the cornerstone of diagnostic imaging. Radiography is based on the absorption of x-rays as they pass through areas of the body composed of material having different densities. X-rays readily pass through air, water, body fluids, fat, and soft tissue and are termed radiolucent; they pass through the exposed area to the film. The images are developed respectively in shades from black to gray. Bone tissue is relatively dense and absorbs x-rays. The effect is termed radiopaque; the bones block radiation from reacting with the x-ray detectors so their images are white; the image created by the bones is essentially the shadow cast from the areas of undeveloped x-ray media.
Uses of radiography include obtaining static internal structural images to diagnose disease, structural damage, or abnormalities; identifying foreign objects; verifying surgical marker placement; planning of radiation therapy regimens. The chest x-ray is the most common radiograph.
Fluoroscopy
Images produced by this technique are generated in similar fashion to the plain x-ray, but the technology uses a continuous stream of x-rays, at a lower dose, to create a “moving picture.”
Uses of fluoroscopy include evaluation of specific areas of the body; evaluation of functional organs during a procedure (e.g., barium enema); guidance during insertion and manipulation of catheters, placement of devices (e.g., stents) or implants, and injections into joints or the spine; angiography; identification and location of foreign bodies; and numerous other applications.
Angiography
Angiography involves injection of contrast into the area of interest allowing for x-ray visualization of organ or vessel structure and function. Angiography should be performed after other studies using contrast to avoid the additive effect of visualizing residual contrast medium; consult the appropriate imaging department.
Uses of angiography include diagnostic and therapeutic applications related to blood vessels and the major associated organ systems (e.g., circulatory, brain). Examples are narrowing or blockage of blood vessels; identification of areas of inflammation or bleeding; and insertion of devices like stents or guidewires for catheterization.
Computed Tomography
CT without contrast is a relatively painless, fast, and accurate noninvasive diagnostic tool. CT uses a motorized x-ray source as opposed to a static source, as with the plain x-ray. The rotation of the x-ray tube around the patient creates detailed cross-sectional images of internal organs, bones, soft tissue, and blood vessels, including the identification of internal bleeding. CT becomes invasive when contrast is introduced via a catheter.
Images can be immediately reviewed on multiple planes and in a three-dimensional format in the imaging department, stored in the facility’s PACS (picture archiving communication system), or copied to an electronic storage device and given to the patient. CT should be performed after other studies using contrast to avoid the additive effect of visualizing residual contrast medium; consult the appropriate imaging department.
Uses of CT are extensive and are not limited to but include rapid assessment or internal injuries due to trauma; diagnosis of bone and soft tissue diseases; identification and location of tumors, thrombosis, or infection; guide surgical procedures, collection of biopsy samples; and monitor response to therapeutic regimens.
Nuclear Medicine
| ||||||||||||||||
Nuclear medicine studies use radioactive tracers that can be injected into a blood vessel (e.g., hepatobiliary scan), inhaled (e.g., lung scan), or swallowed (e.g., C-14 urea breath test) to obtain information on disease processes. Radioactive tracers emit gamma ray energy that can be detected by a conventional gamma camera or single photon emission computed tomography (SPECT)/CT camera, and then used to create computerized images.
Nuclear medicine studies can involve multiple images taken over a specified period of time, after a radionuclide is administered. Imaging intervals vary by study. Each image takes about 20 minutes; serial images may be taken in a single day or over a period of 2 to 3 days. Previous nuclear medicine scans completed within 24 to 48 hr may interfere with the current study due to the measurement of residual tracer in addition to tracer from the current study. The plasma half-life of medical radionuclides is usually short with complete clearance from the blood within 24 to 48 hr. Exceptions include Gallium-67 (78 hr), Indium-111 (2.8 days), Iodine-124 (4.2 days), Iodine-131 (8 days), and Thallium-201 (73 hr).
Pretest dietary considerations vary by procedure. Some procedures have no dietary considerations (e.g., lung scan). Patients may need to be NPO for 8 hr before the procedure (e.g., Meckel’s diverticulum scan), NPO for 8 hr before the procedure but given a special meal in the nuclear medicine department on the day of the scan (e.g., a gastric emptying study), or in other cases patients may be instructed to follow a low carbohydrate diet in the 24 hr prior to the study and be NPO for 8 hr before the study (e.g., PET scan). Individual studies should be reviewed for specific information.
Uses of nuclear medicine applications are extensive and apply to diagnostic imaging as well as planning and implementing therapeutic regimens.
- Treatments using internal exposure to radiation include brachytherapy (irradiation of areas inside a patient, such as implanted radioactive seeds) or teletherapy treatments (noninvasive, serial radiation treatments).
- Alpha radioimmunotherapy or targeted alpha therapy (TAT) is a developing area of study in which a monoclonal antibody is labeled with an alpha-emitting radioisotope. The radioisotope targets cancer at the cellular level for destruction.
PET scans are a specialized group of nuclear medicine studies that can evaluate organ and tissue function in addition to location and structure.
- PET uses radiotracers to map organ and tissue function (blood flow, glucose metabolism, oxygen use) and documents findings with the use of imaging equipment that detects the presence of the radioactive emissions. Technology is now available to simultaneously combine or superimpose the information collected in the PET scan with a CT or MRI study. Evaluation of cellular body changes allows for early recognition of disease onset even before it is noted through other forms of examination.
- PET scans can be used to identify cancer, discern whether the cancer has spread or returned, and evaluate the effectiveness of cancer treatment; it can also be used to evaluate cardiac health, cardiac muscle blood flow, damage caused by heart attack, and the potential benefit of invasive procedures such as angioplasty or surgery such as coronary artery bypass graft.
- PET scans can map heart and brain function and identify tumors and causes of memory disorders, seizures, or central nervous disorders.
- PET radiopharmaceuticals approved by the U.S. Food and Drug Administration (FDA) include F-18 sodium fluoride (bone imaging), Rb-82 rubidium chloride (cardiovascular assessment for MI), F-18 fluorodeoxyglucose (cardiovascular, neurological, oncology applications), and N-13 ammonia (cardiovascular assessment of blood flow).
Magnetic Resonance Imaging
MRI uses magnetic and radio waves to evaluate soft tissue areas of interest for diagnosis of disease and evaluation of the effectiveness of therapeutic interventions. MRI is considered to be a safer alternative than studies involving radiation, such as radiography and CT; the number of MRI studies performed is not limited as with x-ray or CT. However, with MRI, the extremely powerful magnet can inactivate, move, or shift metallic objects inside a patient. Use of an MRI screening tool is recommended to obtain accurate information and foster patient safety. Any questions related to MRI compatibility with the materials used in a patient device should be verified with the manufacturer.
Patients with extreme cases of claustrophobia may require sedation before completing the study. Patients on mechanical ventilators may need to be bagged during MRI. Ear plugs may need to be provided to dampen the loud noises made by the MRI equipment.
In specific situations where gadolinium-based contrast agent (GBCA) will be administered, the risk versus benefit must be evaluated. GBCAs cross the placental barrier, enter the fetal circulation, and pass via the fetal urinary system into the amniotic fluid. Although no definite adverse effects of GBCA administration on the human fetus have been documented, the potential bioeffects of fetal GBCA exposure are not well understood. GBCA administration should therefore be avoided during pregnancy unless no suitable alternative imaging is possible and the benefits of contrast administration outweigh the potential risk to the fetus. The use of GBCAs should also be avoided in patients with kidney dysfunction unless the benefits of the studies outweigh the risks and if essential diagnostic information is not available using non-contrast-enhanced diagnostic studies.
Uses of MRI are extensive and provide especially excellent soft-tissue imaging.
Ultrasound
Ultrasound is a fast, inexpensive, noninvasive way to visualize images with the use of high-frequency sound waves instigated by a transducer. The sound waves bounce off anatomical structures and fluids to provide diagnostic information without the use of radiation.
- Procedures such as endoscopy, surgery, biopsy, barium studies, colonoscopy, and endoscopic retrograde cholangiopancreatography can interfere with US results. US should be performed after other studies using contrast to avoid the additive effect of visualizing residual contrast medium; consult the appropriate imaging department.
Uses for US include assessment of organ perfusion; identification of thrombosis, structural abnormalities of an organ, and tumor; indication of inflammation; response to therapeutic regimens.
Potential Contraindications and Complications Associated With Diagnostic Procedures
Contraindications:
- Pregnancy: with regard to radiation or MRI in imaging, iodinated contrast, radionuclides, and anesthesia
- Pregnancy is a general contraindication to procedures involving radiation, especially when the examination site involves the abdomen, pelvis, or area where the fetus would be in the field of view, unless the potential benefits of a procedure using radiation far outweigh the risk of radiation exposure to the fetus. Explain to the patient that they may be asked the date of their last menstrual period. In all cases, the benefits and risks should be discussed with the HCP before proceeding with the study. Pregnancy testing may be performed in accordance with the facility’s imaging and contrast administration policies. Lower radiation emission technology allows for safe performance of many imaging procedures during pregnancy. The facility’s imaging polices should always be followed.
- Generally, MRI is not contraindicated during pregnancy; however, MRI with contrast (e.g., gadolinium) should be avoided during pregnancy unless no suitable alternative imaging is possible and the benefit far outweighs the potential risk to the fetus and birth parent. GBCA crosses the placental barrier, enters the fetal circulation, and passes via the kidneys into the amniotic fluid. The absence of adverse effects on the human fetus has not been definitively documented either at clinically acceptable or higher medically indicated dosages; the potential adverse effects of fetal exposure are not well understood or well studied.
- Regarding the use of iodinated contrast medium during pregnancy: iodinated contrast medium crosses the placental barrier, enters the fetal circulation, and passes via the kidneys into the amniotic fluid. The absence of adverse effects on the human fetus has not been definitively documented either at clinically acceptable or higher medically indicated dosages; the potential bioeffects of fetal exposure are not well understood or well studied. The facility’s imaging polices should always be followed.
- Generally, pregnancy screening is not indicated for Tc-99m or Ga-67m scans; however, testing may be performed in accordance with the facility’s imaging and radionuclide administration policies. In all cases, the benefits and risks should be discussed with the HCP before proceeding with the study.
- Pregnancy is a general contraindication to procedures involving anesthesia and other medications. Explain to the patient that they will be asked the date of their last menstrual period, and pregnancy testing may be performed to determine the possibility of pregnancy before the patient receives anesthetics. Breastfeeding: with regard to iodinated contrast and radionuclides
- Regarding the use of iodinated contrast medium while breastfeeding: even though a small amount of contrast medium passes into the breast milk, it is considered safe to continue breastfeeding. Benefits and risks should be discussed with the HCP before the patient makes an informed decision to continue or temporarily suspend breastfeeding. Policies may vary among facilities. For those who remain concerned about potential fetal harm, guidelines may recommend suspending breastfeeding from the time of contrast administration through a period of 12 to 24 hr during which the infant may be bottle fed with milk expressed prior to the procedure.
- Regarding the use of gallium-67 while breastfeeding: the patient should be advised prior to scheduling the procedure that complete cessation of breastfeeding is recommended after administration of Ga-67. Explain to the patient who is breastfeeding that due to the large amount of radionuclide that passes into breast milk, complete cessation of breastfeeding is recommended after administration of Ga-67. Discuss alternative strategies for feeding the infant.
- Explain to the patient who is breastfeeding that even though a small amount of the Tc-99m radionuclide passes into the breast milk, it is considered safe to continue breastfeeding. Policies may vary among facilities. Benefits and risks should be discussed with the HCP before the patient makes an informed decision to continue or temporarily suspend breastfeeding. If the patient remains concerned about potential fetal harm, facility guidelines may recommend suspending breastfeeding for a dose/tracer dependent period of time (e.g., 1 to 4 hr) during which the infant may be bottle fed with milk expressed prior to the procedure. General Use of Contrast Medium
- Patients with conditions associated with adverse reactions to contrast medium (e.g., asthma, food allergies, or allergy to contrast medium). Although patients are asked specifically if they have a known allergy to iodine or shellfish (shellfish contain high levels of iodine), it has been well established that the reaction is not to iodine; an actual iodine allergy would be problematic because iodine is required for the production of thyroid hormones. In the case of shellfish, the reaction is to a muscle protein called tropomyosin; in the case of iodinated contrast medium, the reaction is to the noniodinated part of the contrast molecule.
- Patients with a known hypersensitivity to the contrast medium may benefit from premedication with corticosteroids and diphenhydramine; the use of nonionic contrast or an alternative noncontrast imaging study, if available, may be considered for patients who have severe asthma or who have experienced moderate to severe reactions to ionic contrast medium.
Complications:
- Establishing an IV site is an invasive procedure that can cause rare complications such as bleeding from the puncture site (related to a bleeding disorder or the effects of natural products and medications with known anticoagulant, antiplatelet, or thrombolytic properties), nerve injury (which might occur if the needle strikes a nerve), hematoma (related to blood leakage into the tissue following needle insertion), or infection (which might occur if bacteria from the skin surface is introduced at the puncture site).
- The use of contrast may introduce additional nursing implications related to nephrotoxicity (a deterioration of renal function associated with contrast administration), risk for allergic reaction (related to contrast reaction), or tissue damage (related to extravasation or leaking of contrast into the tissues during injection).
Radiation Safety
- The goal for diagnostic studies and medical treatments using radioisotopes or imaging equipment that emits radiation is to prevent unnecessary exposure of staff and patient while meeting clinical diagnostic goals.
- The three most common types of radioactive emissions are alpha, beta, and gamma. Alpha rays are relatively harmless because they do not travel far from the source and do not penetrate most materials. Beta rays can travel several feet from the source, have a lot of energy, and are very small; they can penetrate clothing and skin, making them somewhat more dangerous. Gamma rays have the most energy and are able to penetrate most forms of matter (e.g., air, liquids, solids); they represent a highly dangerous type of exposure that can produce extreme damage.
- Radiation exposure can be external or internal. External exposure can occur either using well-controlled technology to perform diagnostic studies or negligently through inadequate time, distance, and shielding from the radiation source. Internal exposure occurs purposefully through diagnostic or therapeutic means. It can also take place unknowingly with the inhalation of radioactive gas, ingestion of contaminated food or fluids, and absorption of radiation through exposure to contaminated urine, emesis, or other body fluids. The best way to control exposure is to follow the facility’s radiation safety policies and procedures.
Pediatric Imaging Radiation risk is higher in young patients because they have more rapidly dividing cells than adults, and radiation damage occurs during cell division. Therefore, the younger the patient, the more radiation-sensitive the patient is. The Image Gently Campaign is an initiative of the Alliance for Radiation Safety in Pediatric Imaging. Information on the Image Gently Campaign can be found at the Alliance for Radiation Safety in Pediatric Imaging (www.imagegently.org/). The campaign goal is to change practice by increasing awareness of the opportunities to promote radiation protection in the imaging of children. Three unique considerations in pediatric imaging are as follows:
- Children are considerably more sensitive to radiation than adults, which is evidenced in epidemiological studies of exposed populations.
- Children have a longer life expectancy than adults, resulting in a larger window of opportunity for showing radiation damage.
- Children may receive a higher radiation dose than necessary if settings are not adjusted for their small size.
- Some older adults may receive a higher radiation dose than necessary if settings are not adjusted for their small size.
Risks are associated with the use of contrast media, especially iodinated contrast mediums. Pediatric patients have immature or incompletely developed organ and immune systems that do not tolerate the rigors of diagnostic testing as well as adults. Older adults are also potentially less able to tolerate some procedures because their systems are weakened by the natural aging process and interactions that may occur due to the presence of complex multisystem diseases.
- Care should be taken if iodinated contrast medium is scheduled to be used in patients with preexisting renal insufficiency (e.g., chronic kidney disease, single kidney transplant, nephrectomy, diabetes, multiple myeloma, treatment with aminoglycosides and NSAIDs) because iodinated contrast is nephrotoxic. Consideration should also be given to patients who are chronically dehydrated before the test, especially older adults and patients whose health is already compromised, because of their risk of contrast-induced acute kidney injury.
- If iodinated contrast medium is scheduled to be used in patients receiving metformin or medications containing metformin for type 2 diabetes, the drug may be discontinued on the day of the test and continue to be withheld for 48 hr after the test. Failure to withhold metformin may indirectly result in drug-induced lactic acidosis, a dangerous and sometimes fatal side effect of metformin (related to renal impairment that does not support sufficient excretion of metformin). Kidney function should be assessed per facility protocol before use of metformin is resumed (e.g., Cr, eGFR, hydration, or clinical assessment).
Figure A–1 Obtaining an informed and signed consent.
Figure A–2 Site selection. Capillary puncture of the finger.
Figure A–3 Site selection. Capillary puncture of the heel.
Figure A–4 Site selection. Venipuncture arm/hand.
Figure A–5 Site selection. Arterial arm/hand.
Figure A–6 Allen test.
Figure A–7 Arterial puncture.
Figure A–8 Site selection. Starting an IV.
Figure A–9 Urine collection from an indwelling catheter.
Figure A–10 Suprapubic aspiration of a urine specimen.
Figure A–11 Pediatric urine collection.