Approach to the Evaluation and Management of the Patient with Stable Ischemic Heart Disease Based on the Ischemia Trial
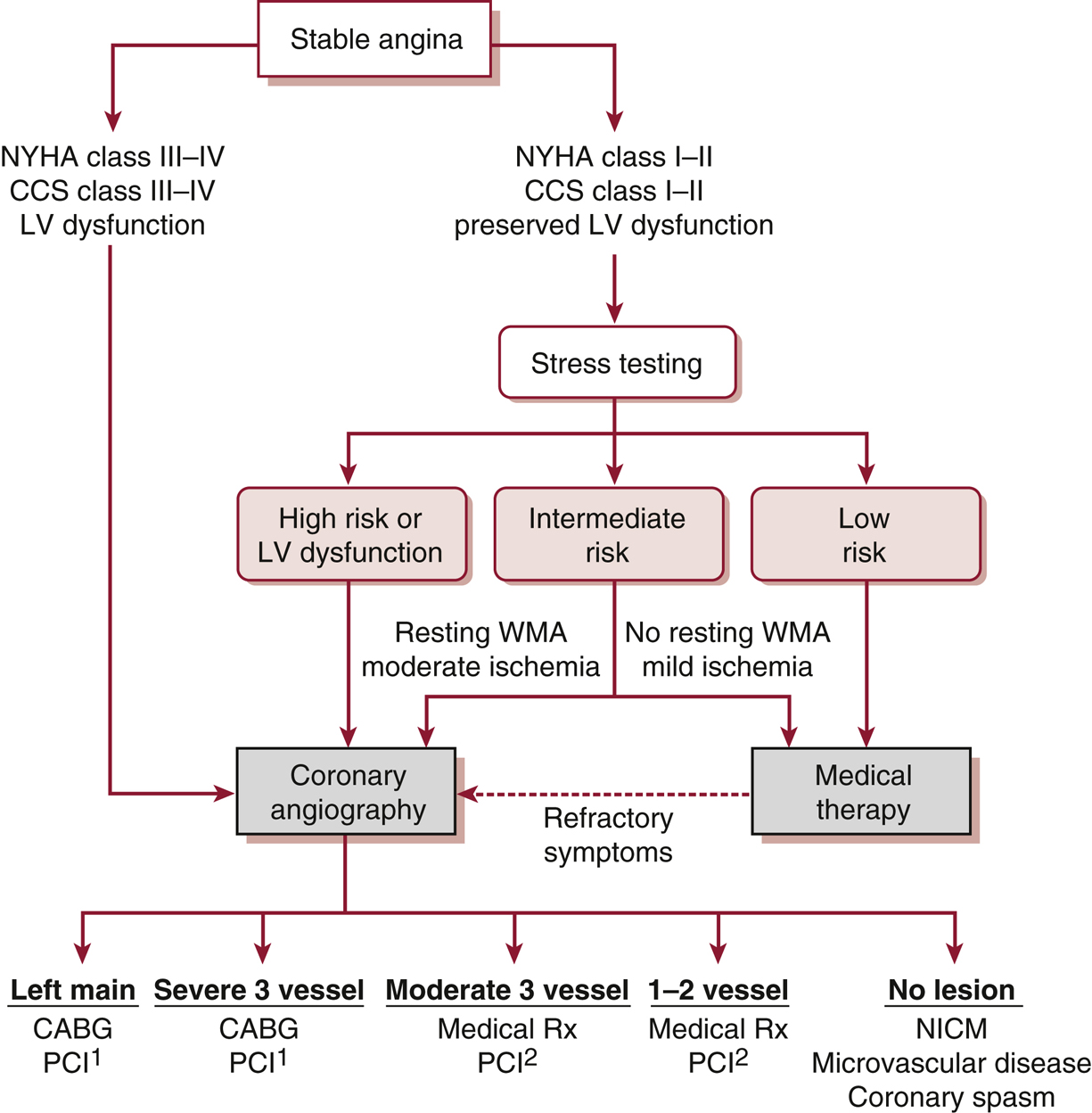
Of note, patients with severe limiting angina, clinical heart failure, or left ventricle (LV) dysfunction should proceed directly to coronary angiography to define underlying coronary artery disease. Patients without these features may first undergo medical optimization with guideline-directed medical therapies (GDMT). If the patient is satisfied with their symptoms on optimal GDMT and is tolerating treatment without significant side effects, coronary CTA should then be obtained to rule out significant left main disease. If no significant left main disease is present, the patient may continue medical therapy without further testing or intervention. If significant left main disease is present, the patient should undergo cardiac catheterization. Patients who are not satisfied with the outcome of optimal GDMT may proceed directly to cardiac catheterization. Information obtained from cardiac catheterization should then be used by a multidisciplinary team to determine whether continued medical therapy, PCI, or CABG should be pursued. 1CABG generally preferred due to known survival advantage over medical therapy alone; however, if the coronary lesions are not complex, PCI may offer similar results to CABG but with a higher need for future revascularizations. 2PCI should be reserved for patients who have high-grade lesions, have severe ischemia, and are refractory to medical therapy. CABG, coronary artery bypass grafting; CCS, Canadian Cardiovascular Society Classification (angina); CTA, computed tomography angiography; NICM, nonischemic cardiomyopathy; NYHA, New York Heart Association; PCI, percutaneous coronary intervention; WMA, wall motion abnormality.