Clinical Algorithm for the Approach to Pts with Community-Acquired Infectious Diarrhea or Bacterial Food Poisoning
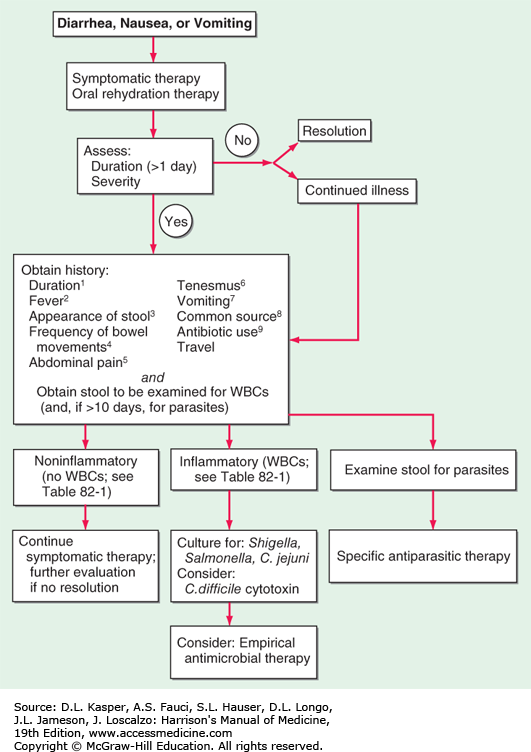
Clinical algorithm for the approach to pts with community-acquired infectious diarrhea or bacterial food poisoning. Key to superscripts: 1. Diarrhea lasting >2 weeks is generally defined as chronic; in such cases, many of the causes of acute diarrhea are much less likely, and a new spectrum of causes needs to be considered. 2. Fever often implies invasive disease, although fever and diarrhea may also result from infection outside the GI tract, as in malaria. 3. Stools that contain blood or mucus indicate ulceration of the large bowel. Bloody stools without fecal leukocytes should alert the laboratory to the possibility of infection with Shiga toxin-producing enterohemorrhagic Escherichia coli. Bulky white stools suggest a small-intestinal process that is causing malabsorption. Profuse “rice-water” stools suggest cholera or a similar toxigenic process. 4. Frequent stools over a given period can provide the first warning of impending dehydration. 5. Abdominal pain may be most severe in inflammatory processes like those due to Shigella, Campylobacter, and necrotizing toxins. Painful abdominal muscle cramps, caused by electrolyte loss, can develop in severe cases of cholera. Bloating is common in giardiasis. An appendicitis-like syndrome should prompt a culture for Yersinia enterocolitica with cold enrichment. 6. Tenesmus (painful rectal spasms with a strong urge to defecate but little passage of stool) may be a feature of cases with proctitis, as in shigellosis or amebiasis. 7. Vomiting implies an acute infection (e.g., a toxin-mediated illness or food poisoning) but can also be prominent in a variety of systemic illnesses (e.g., malaria) and in intestinal obstruction. 8. Asking pts whether anyone else they know is sick is a more efficient means of identifying a common source than is constructing a list of recently eaten foods. If a common source seems likely, specific foods can be investigated. 9. Current antibiotic therapy or a recent history of treatment suggests Clostridium difficile diarrhea. Stop antibiotic treatment if possible and consider tests for C. difficile toxins. Antibiotic use may increase the risk of chronic intestinal carriage after salmonellosis. (After Steiner TS, Guerrant RL: Principles and syndromes of enteric infection, in Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 7th ed, GL Mandell et al [eds]. Philadelphia, Churchill Livingstone, 2010, pp 1335-1351; RL Guerrant, DA Bobak: N Engl J Med 325:327, 1991; with permission.)