Because potassium (K+ ) is the major intracellular cation, discussion of disorders of K+ balance must take into consideration changes in the exchange of intra- and extracellular K+ stores. (Extracellular K+ constitutes <2% of total-body K+ content.) Insulin, β2-adrenergic agonists, and alkalosis tend to promote K+ uptake by cells; acidosis, insulinopenia, or acute hyperosmolality (e.g., after treatment with mannitol or D50W) promotes the efflux or reduced uptake of K+ . A corollary is that tissue necrosis and the attendant release of K+ can cause severe hyperkalemia, particularly in the setting of acute kidney injury. Hyperkalemia due to rhabdomyolysis is thus particularly common, due to the enormous store of K+ in muscle; hyperkalemia may also be prominent in tumor lysis syndrome.
The kidney plays a dominant role in K+ excretion. Although K+ is transported along the entire nephron, it is the principal cells of the connecting segment and cortical collecting duct that play a dominant role in K+ excretion. Apical Na+ entry into principal cells via the amiloride-sensitive ENaC generates a lumen-negative potential difference, which drives passive K+ exit through apical K+ channels. This relationship is key to the bedside understanding of potassium disorders. For example, decreased distal delivery of Na+ tends to blunt the ability to excrete K+ , leading to hyperkalemia. Abnormalities in the renin-angiotensin-aldosterone system (RAAS) can cause both hypo- and hyperkalemia; aldosterone has a major influence on potassium excretion, increasing the activity of ENaC channels and the basolateral Na+/K+-ATPase, thus amplifying the driving force for K+ secretion across the luminal membrane of principal cells.
Major causes of hypokalemia are outlined in Table 1-3 Causes of Hypokalemia. Atrial and ventricular arrhythmias are the most serious health consequences of hypokalemia. Pts with concurrent Mg deficit and/or digoxin therapy are at a particularly increased risk of arrhythmias. Hypokalemia can directly prolong the QT interval and is a significant cofactor in arrhythmias due to other causes of a prolonged QT interval. Other clinical manifestations include muscle weakness, which may be profound at serum [K+ ] <2.5 mmol/L, and, if hypokalemia is sustained, hypertension, ileus, polyuria, renal cysts, and even renal failure.
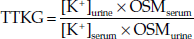
The cause of hypokalemia is usually obvious from history, physical examination, and/or basic laboratory tests. However, persistent hypokalemia may require a more thorough, systematic evaluation (Fig. 1-2. The Diagnostic Approach to Hypokalemia). Initial laboratory evaluation should include electrolytes, BUN, creatinine, serum osmolality, Mg2+ , and Ca2+ , a complete blood count, and urinary pH, osmolality, creatinine, and electrolytes. Serum and urine osmolality are required for calculation of the transtubular K+ gradient (TTKG), which should be <3 in the presence of hypokalemia (see also Hyperkalemia Electrolytes). Alternatively, a urinary K+ -to-creatinine ratio of >13-mmol/g creatinine (>1.5-mmol/mmol creatinine) is compatible with excessive K+ excretion. Further tests such as urinary Mg2+ and Ca2+ and/or plasma renin and aldosterone levels may be necessary in specific cases.
| TREATMENT | ||
HypokalemiaThe goals of therapy in hypokalemia are to prevent life-threatening and/or serious chronic consequences, to replace the associated K+ deficit, and to correct the underlying cause and/or mitigate future hypokalemia. The urgency of therapy depends on the severity of hypokalemia, associated clinical factors (cardiac disease, digoxin therapy, etc.), and the rate of decline in serum K+ . Pts with a prolonged QT interval and/or other risk factors for arrhythmia should be monitored by continuous cardiac telemetry during repletion. Urgent but cautious K+ replacement should be considered in pts with severe redistributive hypokalemia (plasma K+ concentration <2.5 mM) and/or when serious complications ensue; however, this approach has a risk of rebound hyperkalemia following acute resolution of the underlying cause. When excessive activity of the sympathetic nervous system is thought to play a dominant role in redistributive hypokalemia, as in thyrotoxic periodic paralysis, theophylline overdose, and acute head injury, high-dose propranolol (3 mg/kg) should be considered; this nonspecific β-adrenergic blocker will correct hypokalemia without the risk of rebound hyperkalemia. It should be noted that hypokalemia is refractory to correction in the presence of Mg++ deficiency, which also should be corrected when present; renal wasting of both cations may be particularly prominent after renal tubular injury, e.g., from cisplatin nephrotoxicity. Oral replacement with K+ -Cl- is the mainstay of therapy in hypokalemia. Potassium phosphate, oral or IV, may be appropriate in pts with combined hypokalemia and hypophosphatemia. Potassium bicarbonate or potassium citrate should be considered in pts with concomitant metabolic acidosis. The deficit of K+ and the rate of correction should be estimated as accurately as possible; renal function, medications, and comorbid conditions such as diabetes should also be considered so as to gauge the risk of overcorrection. In the absence of abnormal K+ redistribution, the total deficit correlates with serum K+ such that serum K+ drops by approximately 0.27 mM for every 100-mmol reduction in total-body stores. Notably, given the delay in redistributing potassium into intracellular compartments, this deficit must be replaced gradually over 24-48 h, with frequent monitoring of plasma K+ concentration to avoid transient over-repletion and transient hyperkalemia if otherwise appropriate. If hypokalemia is severe (<2.5 mmol/L) and/or if oral supplementation is not feasible or tolerated, IV KCl can be administered through a central vein with cardiac monitoring in an intensive care setting, at rates that should not exceed 20 mmol/h. KCl should always be administered in saline solutions, rather than dextrose; the dextrose-induced increase in insulin can acutely exacerbate hypokalemia. Strategies to minimize K+ losses should also be considered. These measures may include minimizing the dose of non-K+ -sparing diuretics, restricting Na+ intake, and using clinically appropriate combinations of non-K+ -sparing and K+ -sparing medications (e.g., loop diuretics with angiotensin-converting enzyme inhibitors). |
Hyperkalemia
Causes are outlined in Table 1-4 Causes of Hyperkalemia; in most cases, hyperkalemia is due to decreased renal K+ excretion. However, increases in dietary K+ intake can have a major effect in susceptible pts, e.g., diabetics with hyporeninemic hypoaldosteronism and chronic kidney disease (CKD). Drugs that impact on the RAA axis are also a major cause of hyperkalemia.
The first priority in the management of hyperkalemia is to assess the need for emergency treatment (ECG changes and/or K+ ≥6.0 mM). This should be followed by a comprehensive workup to determine the cause (Fig. 1-3. The Diagnostic Approach to Hyperkalemia). History and physical examination should focus on medications (e.g., ACE inhibitors, NSAIDs, trimethoprim/sulfamethoxazole), diet and dietary supplements (e.g., salt substitute), risk factors for acute kidney failure, reduction in urine output, blood pressure, and volume status. Initial laboratory tests should include electrolytes, BUN, creatinine, serum osmolality, Mg2+ , and Ca2+ , a complete blood count, and urinary pH, osmolality, creatinine, and electrolytes. A urine [Na+ ] <20 meq/L suggests that distal Na+ delivery is a limiting factor in K+ excretion; volume repletion with 0.9% saline or treatment with furosemide may then be effective in reducing serum [K+ ] by increasing distal Na+ delivery. Serum and urine osmolality are required for calculation of the TTKG. The expected values of the TTKG are largely based on historic data: <3 in the presence of hypokalemia and >7-8 in the presence of hyperkalemia.
| TREATMENT | ||
HyperkalemiaThe most important consequence of hyperkalemia is altered cardiac conduction, with the risk of bradycardic cardiac arrest. Figure 1-4. Diagrammatic ECGs at Normal and High Serum K shows serial ECG patterns of hyperkalemia; ECG manifestations of hyperkalemia should be considered a true medical emergency and treated urgently. However, ECG changes of hyperkalemia are notoriously insensitive, particularly in pts with CKD; given these limitations, pts with significant hyperkalemia (K+ ≥6-6.5 mmol/L) in the absence of ECG changes should also be aggressively managed. Urgent management of hyperkalemia constitutes a 12-lead ECG, admission to the hospital, continuous cardiac monitoring, and immediate treatment. Treatment of hyperkalemia is divided into three categories: (1) antagonism of the cardiac effects of hyperkalemia, (2) rapid reduction in [K+ ] by redistribution into cells, and (3) removal of K+ from the body. Treatment of hyperkalemia is summarized in Table 1-5 Treatment of Hyperkalemia. Kayexalate, a mainstay of hyperkalemia treatment, has been linked to fatal colonic necrosis; if available, sodium zirconium cyclosilicate (ZS-9) or patiromer, newer potassium binders that do not cause colonic necrosis, should be used in preference to kayexalate. |