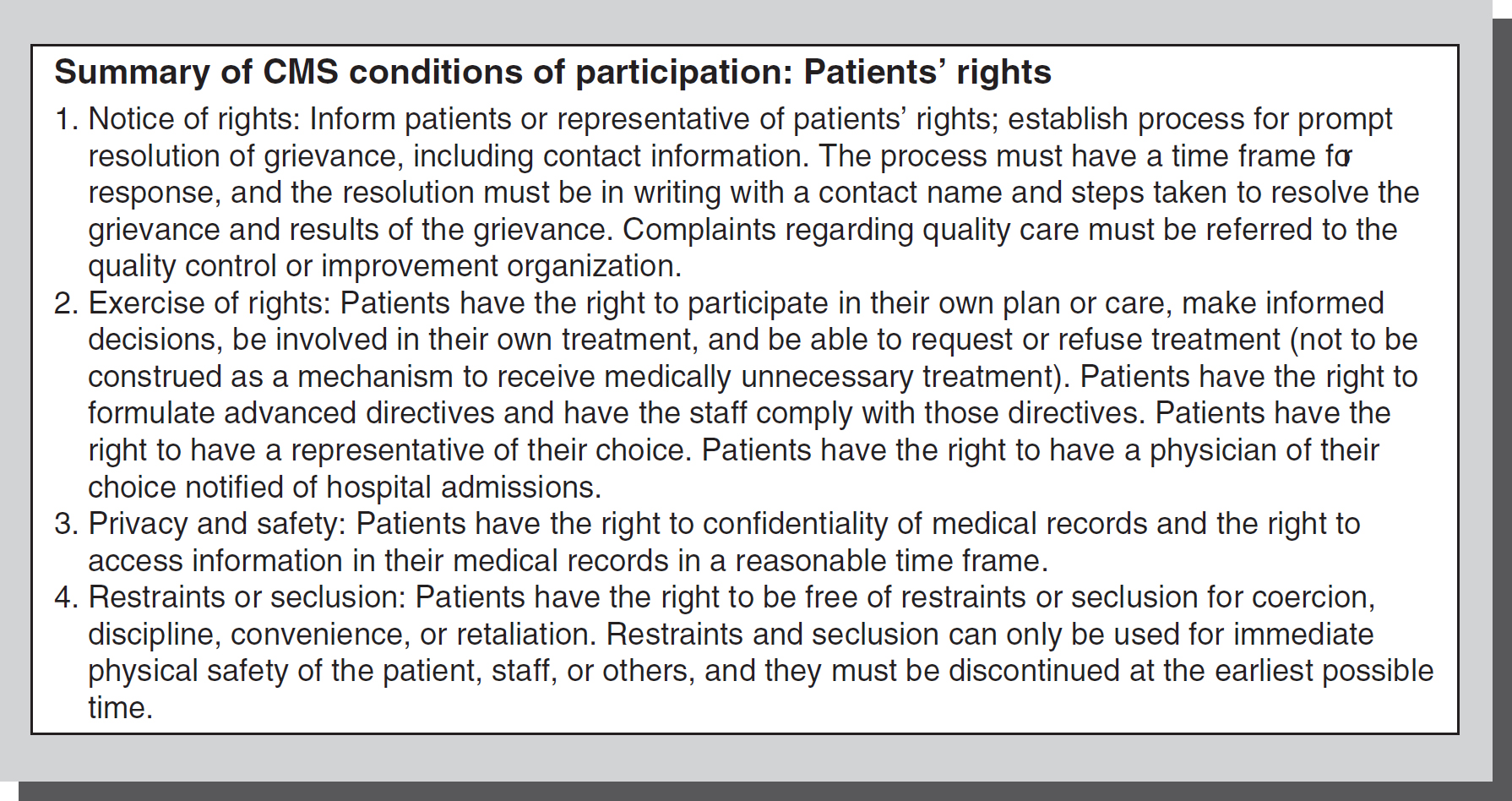
Figure 11-1 Sources of patients' rights and responsibilities.
Over the years, several organizations have enumerated various patients' rights, the most prominent lists of which have come from the American Nurses Association (ANA), American Hospital Association (AHA), and the American Medical Association (AMA). These patients' bills of rights had no legal mandate for participation. Thereafter, the Centers for Medicare and Medicaid Services (CMS) established patients' rights, which mandate that hospitals establish a process to promptly resolve a patient's grievance and establish procedures for confidentiality, privacy, safety, and the right to participate in one's own healthcare treatment plan (
CMS Conditions of Participation: Patients' Rights, 2006). There have been updates to the CMS conditions of participation regarding patients' rights which include the federal 2022 “No Surprise Act” (NSA) which protects healthcare consumers from surprise bills for some types of medical services (
CMS.gov). Without knowledge of these regulatory rights or rights established by state statutes, nurses cannot successfully protect and support those rights under regulatory mandates or prevent professional liability for patient harm when rights are deprived.
Since the 1970s, public entities and the legal system have worked to provide the basis for what we now know as patients' rights (see Figure 11-1). Beginning with the right to informed consent, other important issues evolved through landmark case law, such as the right to refuse medical treatment (In Re Karen Quinlan, 1976) as an established right.
The Patient Self-Determination Act (PSDA) of 1990 also provided the legal means by which patients could, by law, obtain more control over their health care, treatment, and decisions pertaining to both. The act requires all providers that receive Medicaid funds to provide individuals with written information regarding their rights to make decisions about their medical care. Medical providers are also required to inform patients about their rights to establish advance directives at the time of admission.
In addition, the President's Advisory Commission on Consumer Protection and Quality in the Health Care Industry (1997, 1998) issued a proposal for a national bill of patients' rights. It was the responsibility of the commission to promote and assure healthcare quality and to protect consumers and workers in the healthcare system. The commission enumerated seven patients' rights and one responsibility. These rights include rights to information, to choose healthcare providers, access to emergency services, being a full partner in healthcare decisions, care without discrimination, right to privacy, right to speedy complaint resolution, and taking on greater responsibility in one's own health care.
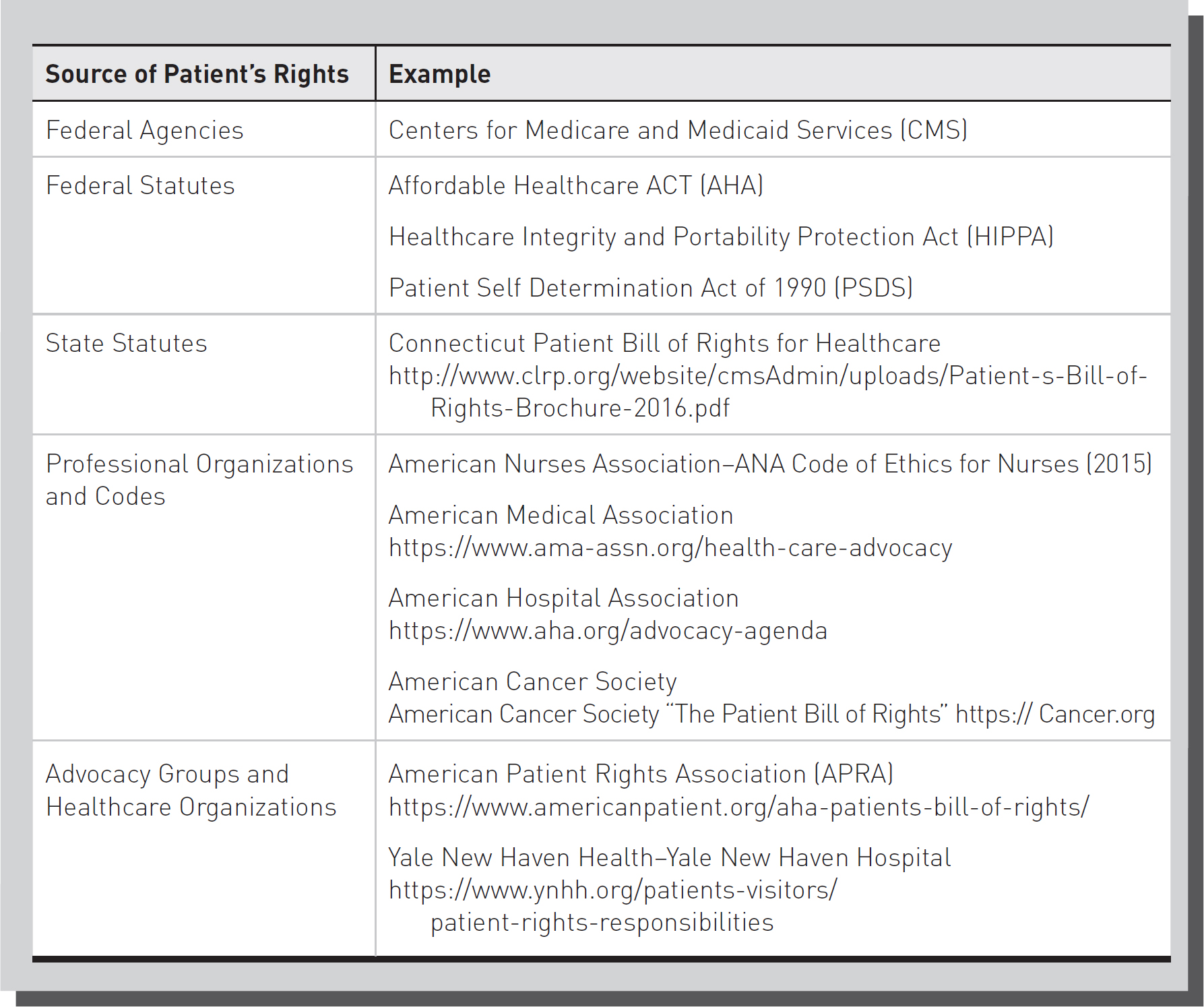
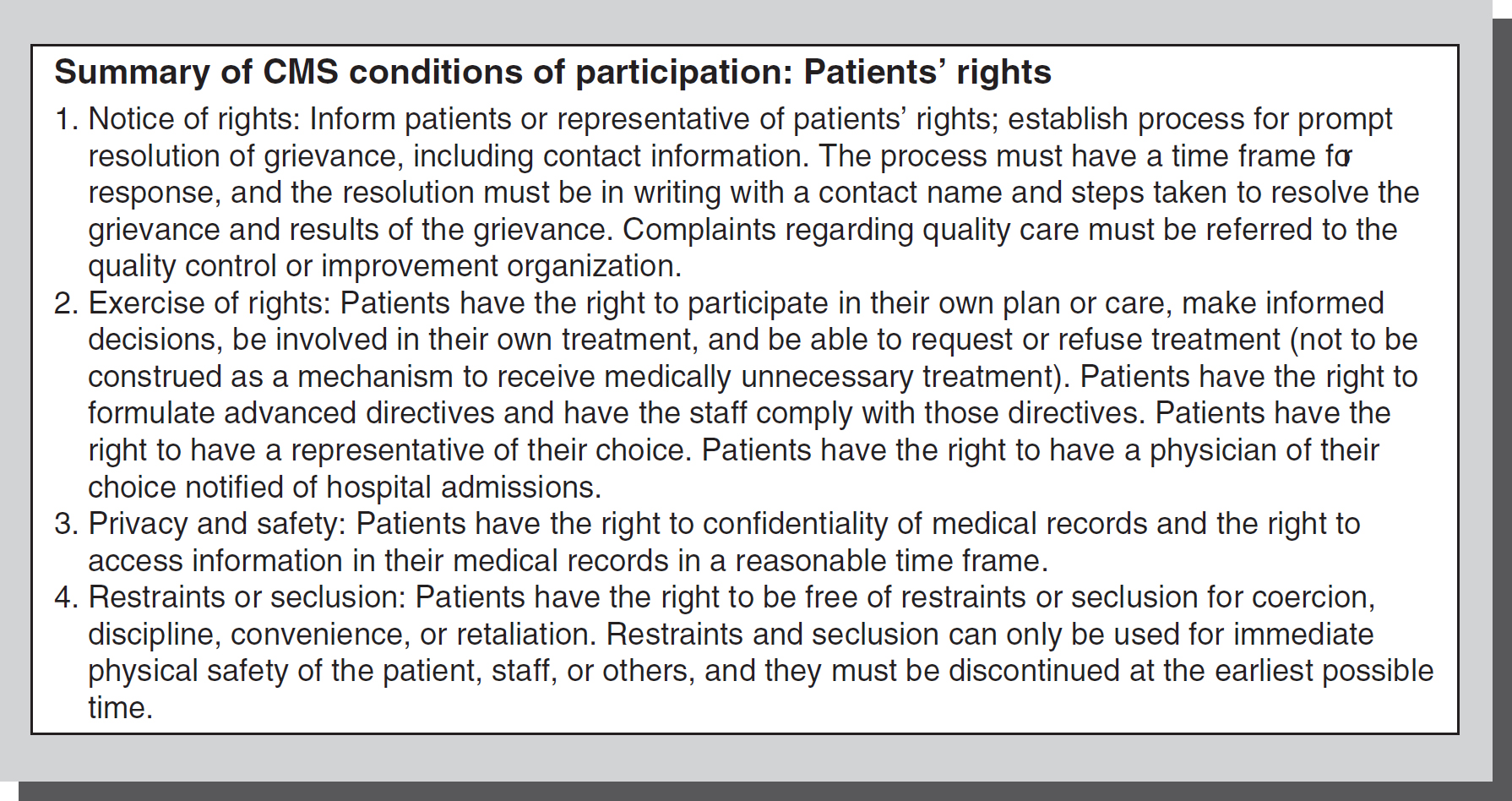
The Centers for Medicare and Medicaid Services has the strongest patients' rights protections. CMS has the enforcement tools of suspending payments for participating institutions and civil monetary penalties. To receive payments under Medicare and Medicaid, the hospital must protect and promote patients' rights under the following standards:
- Notice of rights
- Exercise of rights
- Privacy and safety
- Confidentiality of medical records
- Restraint or seclusion (including staff training requirements and death notification requirements)
These conditions of participation are summarized in Figure 11-2.
Figure 11-2 Summary of CMS conditions of participation: patients' rights (2006, amended 2019).
© Jones & Bartlett Learning
Accreditation by The Joint Commission also includes establishing procedures that ensure patients' rights. The right to be included in planning and treatment, informed consent (including before any pictures or filming occurs for purposes other than diagnosis, identification, and treatment), information on providers who are responsible for care and treatment, and the right to refuse care. Respect for end-of-life decisions includes assistance with advance directives, documentation on executing a signed directive, and procedures for honoring organ donation wishes. Unexpected outcomes must be disclosed. Patients have the right to effective communication in a manner they understand, including interpretative services and access to advocacy programs. Confidentiality and privacy will be protected, and proper pain management procedures will be in place. CMS also emphasizes that there are federal laws to ensure patients' rights, including to obtain their medical records and keep them private. Many states and healthcare organizations also have additional patient bills of rights. Another right is to informed consent for any major medical procedure or treatment decision. Insurance related bills of rights, and those pertaining to the Affordable Care Act (ACA) and Medicare can also be found on the government website (HHS.gov). Additional sources of patient rights statements are from state resources, advocacy groups, professional and healthcare organizations, and specialty organizations, such as the American Cancer Society.
Certain elements for performance under patients' rights must be measured for success by the accredited institution. Success is determined by a quantifiable measure, such as an audit of charts for pain management Assessment, Intervention, and Reassessment (AIR cycles) or the signature of an interpreter on an informed consent form for a patient with partial hearing loss.
In 2003, the American Hospital Association replaced the patient's bill of rights with a brochure titled “The Patient Care Partnership: Understanding Expectations, Rights, and Responsibilities.” This brochure explains what to expect during the hospital stay and includes patients' rights to:
- High-quality hospital care
- A clean and safe environment
- Involvement in their own care
- Protection of privacy
- Help when leaving the hospital
- Help with billing claims (AHA, 2003)
Recipients of mental health services have specific state statutory patient right protections: informed consent, access to medical records, confidentiality of medical treatment, privacy, and to be free of abuse or coercion. In addition, patients have the right to be free of being observed through one-way glass (or video- and audiotaping) without consent. Exceptions to this rule may apply to any patient who has made a threat to a healthcare provider serious enough to require notification to security or the police, as well as to the person who has been threatened. Notification of formal voluntary and involuntary admissions must be given.
The 2015 ANA “Code for Nurses with Interpretative Statements” sets forth the nurse's moral and professional obligation to patients based on a value belief system. The nurse's primary commitment is to the recipients of healthcare services whether individuals, families, groups, communities, or populations. This philosophy of self-determination fosters and supports the patient's need for autonomy to the greatest extent possible. The nurse needs to take into account the inherent rights of patients. The nurse has a responsibility to protect patients' ability to manage their own health care and treatment. The ANA code for nurses requires that nurses treat and provide services to their patients with respect for the human dignity and uniqueness of each person by recognizing each patient's rights. The ANA Nursing: Scope and Standards of Practice (2021) includes a standard of professional performance for ethics. Within this standard are expectations for nurses to advocate for healthcare consumer perspectives and respect their autonomy, safeguard sensitive information, and respect the ethical principles of beneficence, fidelity, non-malfeasance, and justice. Included within the justice requirement is the need to integrate principles of social justice in nursing practice.
In conjunction with the mandate to protect and facilitate the delivery of medical care based on these rights, the nurse also has an obligation to the health profession to ensure that the patient is not acting in a manner that would thwart treatment or exacerbate a medical condition.
While patients' rights have far-reaching incentives for compliance in institutions that participate in Medicare/Medicaid payments or those accredited by The Joint Commission, state statutes that enumerate certain patients' rights may give a private right of action for liability when those rights are negligently deprived and patient injury occurs. Each state that codified patients' rights did so in a similar fashion to CMS and accreditation bodies. Some states' patients' rights laws are specific to certain organizations, such as long-term care or managed care organizations.
In one case alleging violation of states' rights, an administrator of her sister's estate brought several claims against her sister's nursing home after she died of a Salmonella outbreak, including negligence, civil conspiracy, and violation of the state patients' bill of rights. The violation of the bill of rights stemmed from failure to inform the decedent of her medical condition, failure to afford the decedent an opportunity to participate in her care, failure to inform her of her rights and assistance in exercising her patient rights, and failure to treat her with respect and consideration. The applicable statute states that any facility that negligently deprives a patient of a right established in the statute is liable for injuries that occurred as a result of the negligent deprivation. In this case, however, liability on this issue was never determined because the count alleged under the bill was brought past the statute of limitations. This case demonstrates that states do allow a private cause of action for violation of enumerated patient's rights (Durkin v. First Healthcare Corporation et al., 1990).
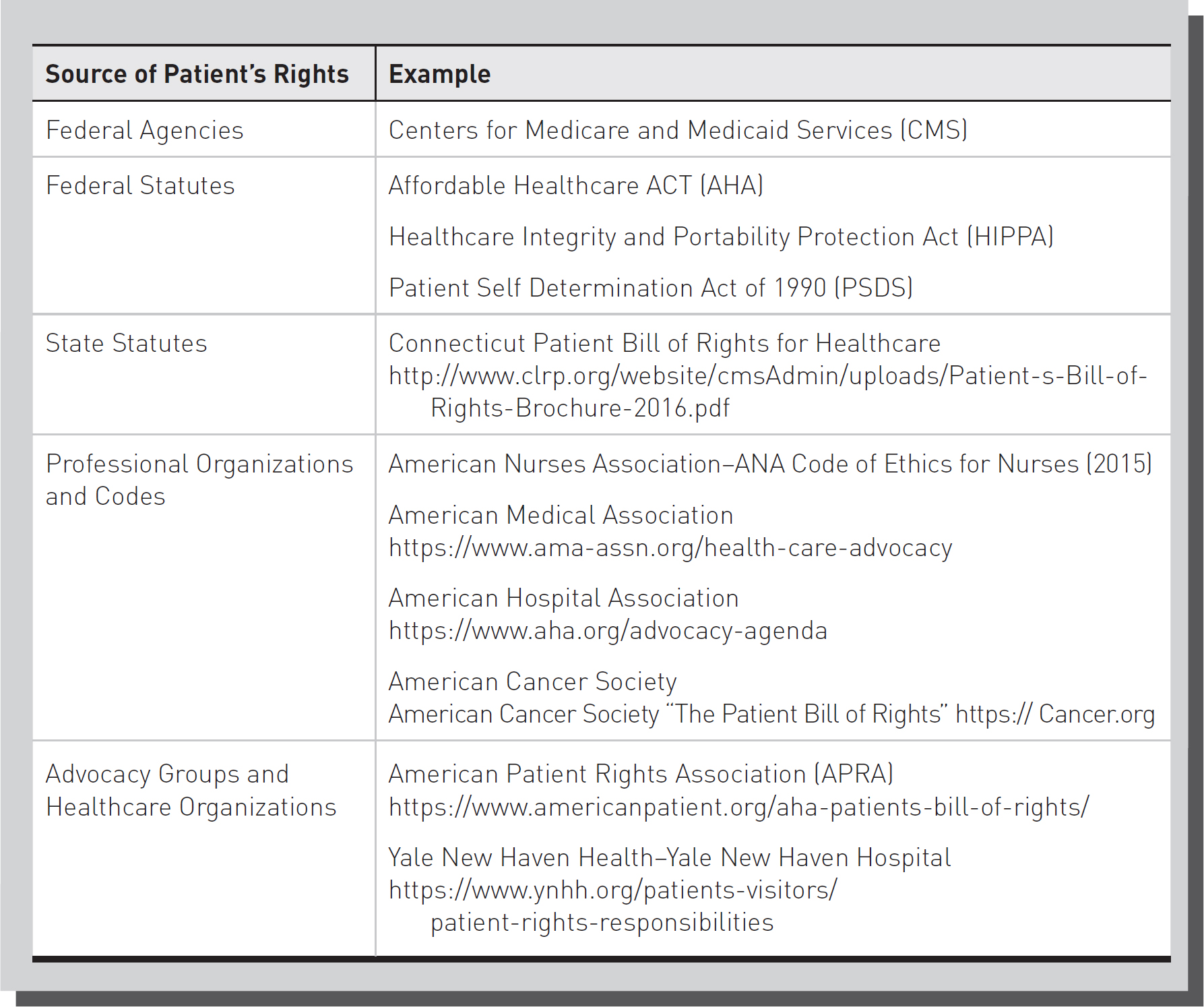 Over the years, several organizations have enumerated various patients' rights, the most prominent lists of which have come from the American Nurses Association (ANA), American Hospital Association (AHA), and the American Medical Association (AMA). These patients' bills of rights had no legal mandate for participation. Thereafter, the Centers for Medicare and Medicaid Services (CMS) established patients' rights, which mandate that hospitals establish a process to promptly resolve a patient's grievance and establish procedures for confidentiality, privacy, safety, and the right to participate in one's own healthcare treatment plan (CMS Conditions of Participation: Patients' Rights, 2006). There have been updates to the CMS conditions of participation regarding patients' rights which include the federal 2022 “No Surprise Act” (NSA) which protects healthcare consumers from surprise bills for some types of medical services (CMS.gov). Without knowledge of these regulatory rights or rights established by state statutes, nurses cannot successfully protect and support those rights under regulatory mandates or prevent professional liability for patient harm when rights are deprived.
Over the years, several organizations have enumerated various patients' rights, the most prominent lists of which have come from the American Nurses Association (ANA), American Hospital Association (AHA), and the American Medical Association (AMA). These patients' bills of rights had no legal mandate for participation. Thereafter, the Centers for Medicare and Medicaid Services (CMS) established patients' rights, which mandate that hospitals establish a process to promptly resolve a patient's grievance and establish procedures for confidentiality, privacy, safety, and the right to participate in one's own healthcare treatment plan (CMS Conditions of Participation: Patients' Rights, 2006). There have been updates to the CMS conditions of participation regarding patients' rights which include the federal 2022 “No Surprise Act” (NSA) which protects healthcare consumers from surprise bills for some types of medical services (CMS.gov). Without knowledge of these regulatory rights or rights established by state statutes, nurses cannot successfully protect and support those rights under regulatory mandates or prevent professional liability for patient harm when rights are deprived.