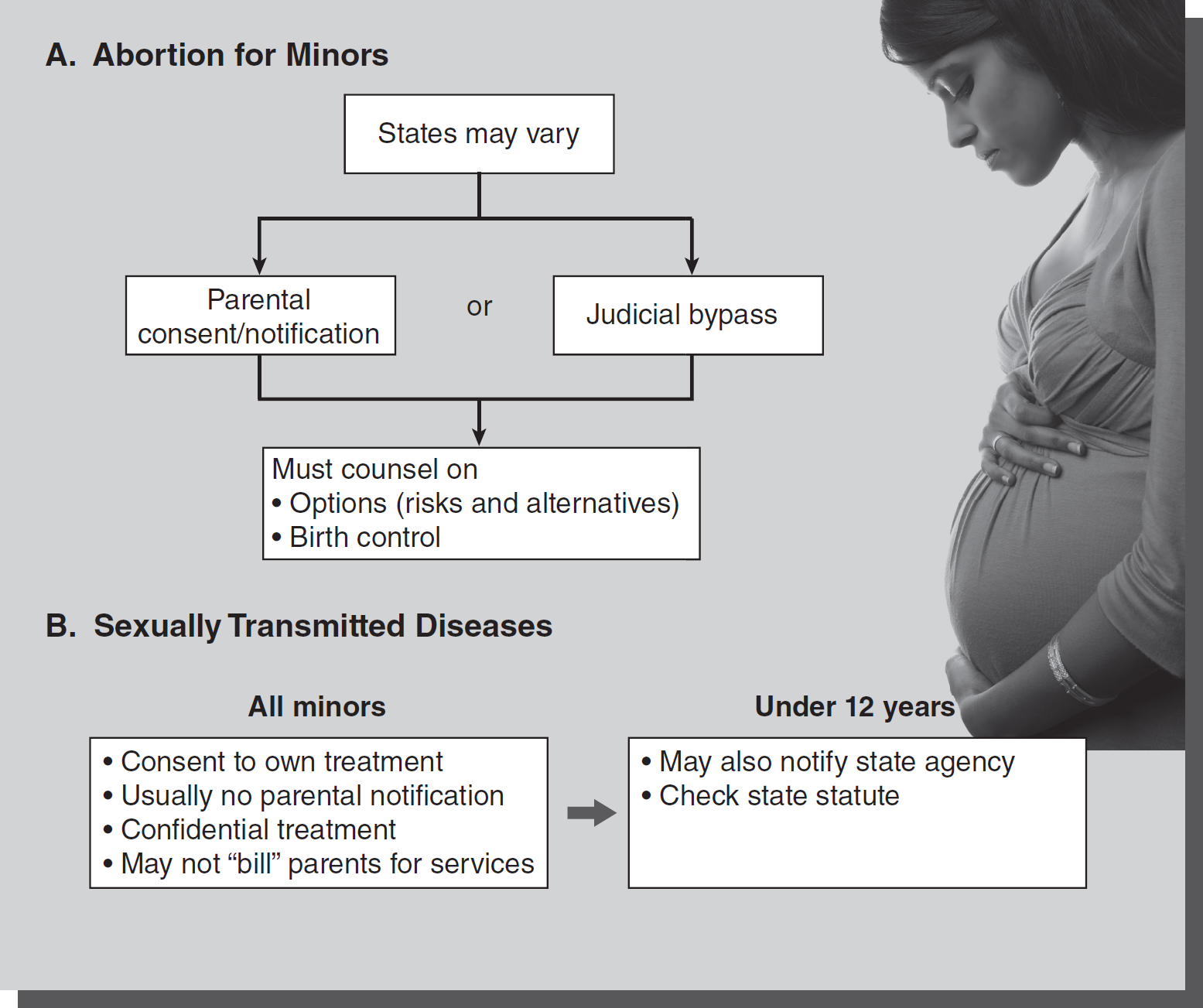
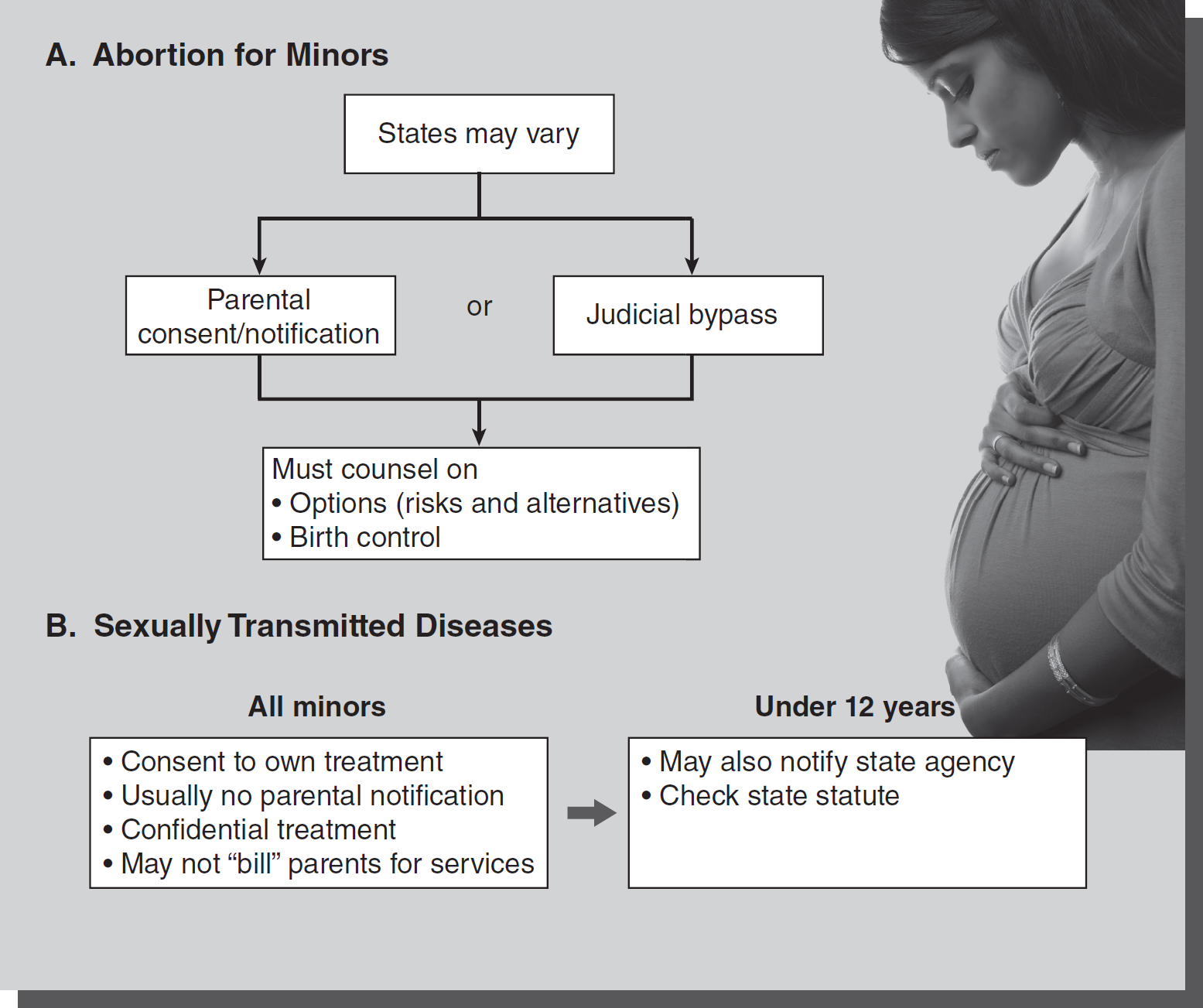
Figure 21-1 Reproductive services for minors.
© Jones & Bartlett Learning; © Hemera/Thinkstock
Patients have a right to privacy and a right to make informed healthcare decisions based on full disclosure of information. Healthcare providers have an obligation to inform the patient of all healthcare choices that are legal. Healthcare providers can objectively discuss reproductive services such as abortion, contraception, and treatment of sexually transmitted
diseases (STDs) and need to be aware of the informed consent and notification issues involving the treatment of minors (see
Figure 21-1).
Termination of pregnancy is not an absolute right, with each state setting limitations for adults and minors. The recent landmark 2022 U.S. Supreme Court case of Dobbs v. Jackson Women's Health Organization further changed and restricted these rights as the court overruled the previous longstanding federal right to abortion as based on the Roe. V. Wade case and its trimester framework decided in 1973. Currently, this right to abortion depends on which state a person resides in, causing confusion, differing rights, and access barriers for many seeking these services. The law is continually evolving in this area, and practitioners must consult current state statutes to be informed and compliant with requirements. The area of abortion rights remains a controversial and divisive area of concern for healthcare practitioners and citizens.
Adults-Historical Perspective and Evolution-Pre-Dobbs
A patient's right to privacy included the decision to continue with or terminate a pregnancy up to the point of fetal viability under the previous Roe v. Wade trimester framework. When the point of fetal viability was reached (somewhere in the second trimester), the state was viewed as having some interest in preserving life and could put some limits on abortion. However, these limitations could not cause an undue burden on the patient. Undue burden has not been completely defined and has been determined on a case-by-case analysis. The court has upheld a restriction on federal and state funding for abortions (Maher v. Roe, 1977), but struck down provisions requiring a woman to obtain a spouse's written consent (Planned Parenthood of Missouri v. Danforth, 1976). Spouses may not compel their spouse to complete or terminate a pregnancy.
Historically, the court has also struck down a state provision requiring physicians to follow a specified informed consent form prior to completing abortions. The court found it too intrusive on the physician-patient relationship, because the consent form disregarded the physician's judgment on what was relevant to each individual's case. The court has also upheld a statute requiring physicians to test fetal viability when the pregnancy is around the 20th week. Technology has changed in the years since the Roe v. Wade 1973 decision, enabling younger fetuses to survive longer. Some states have a medical emergency exception that permits dispensing with the informed-consent requirement when the physician makes a good faith conclusion that medical complications of pregnancy necessitate a therapeutic abortion. This exception sometimes includes serious mental health issues. Each state specifically enumerates what constitutes a medical emergency (such as loss of life or major bodily function).
Minors
Each state has statutes governing abortions on minors (see Figure 21-1A). Nurses who practice in areas providing abortion to minors must be concerned with parental notification and counseling. There are variations in each state on whether a minor may receive an abortion without parental consent. The U.S. Supreme Court answered the question of whether the right to privacy included a minor's right to an abortion in Planned Parenthood v. Danforth (1976) and Bellotti v. Baird (1979). An unemancipated minor's right to reproductive choice is not equal with that of an adult, even in the early stages of pregnancy. No state provision may categorically deny a minor the right to an abortion, and parents may not have absolute veto power over the minor's decision. Although states and parents may not exercise absolute veto power over a minor's reproductive choice, a minor has no absolute right to exercise that choice without authorization from a parent, guardian, or judge. Therefore, states may involve parents by requiring parental notification without giving parents the power of consent. States must be consistent in ensuring that third parties do not have absolute power over another's decision to terminate a pregnancy. Constitutionally, states may require parental consent (usually only one parent is needed to meet statutory requirements), but the state must also include an alternative to parental consent. This alternative has become known as a bypass provision. The bypass provision grants courts the power to determine if a minor is mature enough to consent to an abortion without parental consent or notification. This alternative recognizes that parental consent is not always in the best interest of the minor. Abusive or strained relationships may only worsen when parental consent or notification is required.
All minors must be counseled on options, such as adoption and keeping the baby. Minors must sign a form stating they were not coerced and that they understand the risks and alternatives. Birth control options also must be discussed. States may additionally require the healthcare providers to counsel minors on available clinics for birth control services as part of abortion informed consent.
Treating a minor without parental consent for a “morning after pill” to prevent pregnancy was found not to be a violation of the parents' constitutional rights to parental liberty or the minor's due process rights because the minor sought treatment. The parents brought suit against the city clinic when the minor became sick from the treatment. The court held the conduct the parents complained of was devoid of any compulsion or constraint, and under these circumstances, neither the due process clause nor other constitutional provisions required the parent to be notified (Anspach et al. v. City of Philadelphia et al., 2007).
Restrictions on Abortions-Post-Roe v. Wade
In recent years, states have imposed various restrictions on the right to abortions, which have undermined the Roe v. Wade 1973 decision. Some commentators suggest that Roe was being chipped away to the point of losing its force and the right to unrestricted abortions within the parameters of the Roe decision, and in fact the Dobbs decision all but overrules Roe v. Wade at this time. The negative effects of this movement affect marginalized populations and those of limited financial means to a greater extent, thus impairing reproductive rights for these vulnerable populations. According to the Guttmacher Institute, a leading research and policy organization committed to advancing sexual and reproductive health rights (SRHR) worldwide, abortion rights have been regulated and eroded by states in the following ways:
- Physician and Hospital Requirements: Thirty-eight states require an abortion to be performed by a licensed physician. Nineteen states require an abortion to be performed in a hospital after a specified point in the pregnancy.
- Gestational Limits: Forty-three states prohibit abortions after a specified point in pregnancy, with some exceptions provided. The allowable circumstances are generally when an abortion is necessary to protect the patient's life or health.
- “Partial-Birth” Abortion: Twenty-one states have laws in effect that prohibit “partial-birth” abortion. Three of these laws apply only to postviability abortions.
- Public Funding: Sixteen states use their own funds to pay for all or most medically necessary abortions for Medicaid enrollees in the state. Thirty-three states and the District of Columbia prohibit the use of state funds except in those cases when federal funds are available: where the patient's life is in danger or the pregnancy is the result of rape or incest. South Dakota limits funding to cases of life endangerment only.
- Coverage by Private Insurance: Twelve states restrict coverage of abortion in private insurance plans, most often limiting coverage only to when the patient's life would be endangered if the pregnancy were carried to term. Most states allow the purchase of additional abortion coverage at an additional cost.
- Refusal: Forty-five states allow individual healthcare providers to refuse to participate in an abortion. Forty-five states allow institutions to refuse to perform abortions, sixteen of which limit refusal to private or religious institutions.
- State-Mandated Counseling: Eighteen states mandate that individuals be given counseling before an abortion that includes information on at least one of the following: the purported link between abortion and breast cancer (5 states), the ability of a fetus to feel pain (13 states) or long-term mental health consequences for the patient (8 states).
- Waiting Periods: Twenty-five states require people seeking an abortion to wait a specified period of time, usually 24 hours, between when they receive counseling and the procedure is performed. Twelve of these states have laws that effectively require the patient to make two separate trips to the clinic to obtain the procedure.
- Parental Involvement: Thirty-seven states require some type of parental involvement in a minor's decision to have an abortion. Twenty-seven states require one or both parents to consent to the procedure, while ten require that one or both parents be notified (Guttmacher Institute, 2021).
Post-Dobbs Abortion Rights
Since the 2022 U.S. Supreme Court's Dobbs decision, states have various laws in effect. These laws have individual provisions and requirements that have resulted in different rights and access to abortions for those who are residents of different states. Healthcare practitioners must be familiar with the laws of the state where they provide care to be sure they are in compliance with these state laws. State location, local and state policies, financial burdens, and access to healthcare practitioners present obstacles to fair and equal access to abortions and related procedures. According to Casas (2020), the Supreme Court in Dobbs v. Jackson Women's Health Organization (2022) eliminated federal protection and access to numerous abortion services. At present, many states greatly limit abortion services, or ban them all together. Healthcare practitioners must be familiar with various state laws regarding abortion, so legally permitted services can be provided and explained to patients. Rights and access to abortions vary from state to state. For example, Pennsylvania restricts abortions after 24 weeks, but in Ohio this is a 6-week ban. The Guttmacher Institute maintains current information on states where abortion remains legal (Casas et al., 2022). Additionally, the Hyde Amendment prohibits use of federal funds to pay for abortions except in cases of life endangerment, incest, or rape. Funds to pay for abortions may not be available through Medicaid in many states, and coverage under private insurance or through the Affordable Care Act (ACA) is also variable (Casas, 2020). Often there are extra expenses and obstacles for patients when they must travel to a different state for needed services. These burdens may make abortion services unattainable for many patients. Nurses, and especially advanced practice registered nurses (APRNs), need to check not only practice guidelines for abortion services, but be familiar with the ever-changing rights for patients in this evolving area of practice. Patients need to be supported and assisted to meet their reproductive needs within the requirements of the law, while considering ethical standards. The Casas article contains a helpful table of comprehensive and up-to-date resources for patients and practitioners (p. 4273).
Nurses and especially advanced practice nurses and midwives are cautioned to carefully review the laws of any state they are practicing in, since these abortion laws are state specific and may be subject to change.
Minors have the highest STD rate of any age group, yet they seek treatment the least because they fear parental notification by healthcare providers. Healthcare providers in the position of treating minors must be aware of the specific state legislation on minors. Most healthcare providers treating minors for STDs are concerned with parental consent even though litigation against providers in this area is uncommon. State statutes enumerate the age of minority for consenting to reproductive services, which include testing for HIV and STDs (see Figure 21-1B). Some states may require that the state public health or family advocate services be notified that a minor under a certain age (usually 12 years) is seeking reproductive services. This is not the same as parental notification.
When a minor is diagnosed and treated for an STD, the confidentiality statutes require that all information related to the treatment be given only to the young patient. State statutes may require parental notification that a minor has been hospitalized for STD-related treatment if the minor will be hospitalized for greater than a set amount of time (such as 12 or 16 hours).
The state, however, may compel a clinic that provides treatment to minors for sexually transmitted diseases to notify the state when the clinic becomes aware of sexual contact between a minor and an adult or other of disparate age when the conduct is in violation of the state statutory rape laws. In The People ex. Re. Eichenberger v. Stockton Pregnancy Control Medical Clinic, Inc. (1988), the appeals court held the state had a compelling interest in the sexual conduct of a minor 14-year-old and another of disparate age, which constituted a felony sexual assault. The violation of the minor's privacy was justified.
Communicable disease reporting and public health notification requirements are the exception to this. Confidential treatment includes the billing process. The minor is responsible to pay for services, and the parents may not be billed, thus preserving the minor's confidentiality for treatment. Healthcare providers must obtain the minor's informed consent to treatment and determine whether the minor understands the nature, risks, and benefits of the procedure, as well as any alternative treatments.
Several states have statutes that authorize providers to treat minors for sexual assault with the minor's consent to treatment and education on sexually transmitted diseases. Parental notification is required unless the parent is suspected of the assault. Absent a specific state statute to treat, the institution should have guidelines for treating minors in this situation under the mature minor exception or emergency exception.
Emergency contraception reduces the likelihood of pregnancy by 81-90% if taken within 72 hours of intercourse. Although emergency contraception has been available in the United States for several years, less than half of the states have legislation regarding emergency contraception. States laws either mandate emergency departments to offer the contraception to patients who experienced sexual assault or allow pharmacists to dispense directly to patients without a physician's prescription. Currently, some states provide for both. This continues to be an area of developing law where healthcare practitioners must consult state statutes.
Recently, the U.S. Department of Health and Human Services (HHS) added additional protections for reproductive information. On April 22, 2024, a Final Rule was issued by Office for Civil Rights (ORC), entitled HIPAA Privacy Rule to Support Reproductive Health Care Privacy. The Final Rule expands the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule by prohibiting the disclosure of protected health information (PHI) related to lawful reproductive health care in certain circumstances. HHS issued this Final Rule to better protect patient confidentiality and prevent medical records from being used against people for providing or obtaining lawful reproductive health care. This Final Rule enhances privacy and patient-provider confidentiality to foster trust and open communication between individuals and their healthcare providers or health plans (HHS, 2024).