Critical
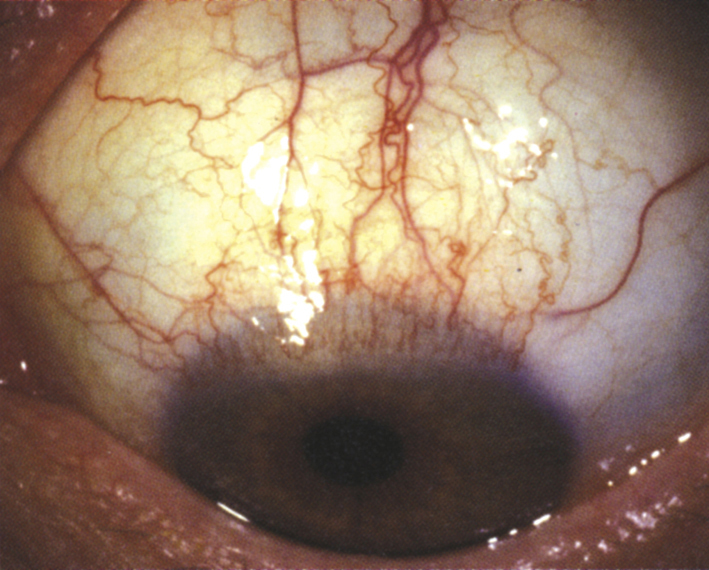
Sectoral thickening, inflammation, and radial injection of the superior bulbar conjunctiva, especially at the limbus. Superior bulbar conjunctivochalasis often present (see Figure 5.4.1).
Other
Fine papillae on the superior tarsal conjunctiva; fine punctate fluorescein staining on the superior cornea, limbus, and conjunctiva; superior corneal micropannus and filaments. Usually bilateral, frequently asymmetric.