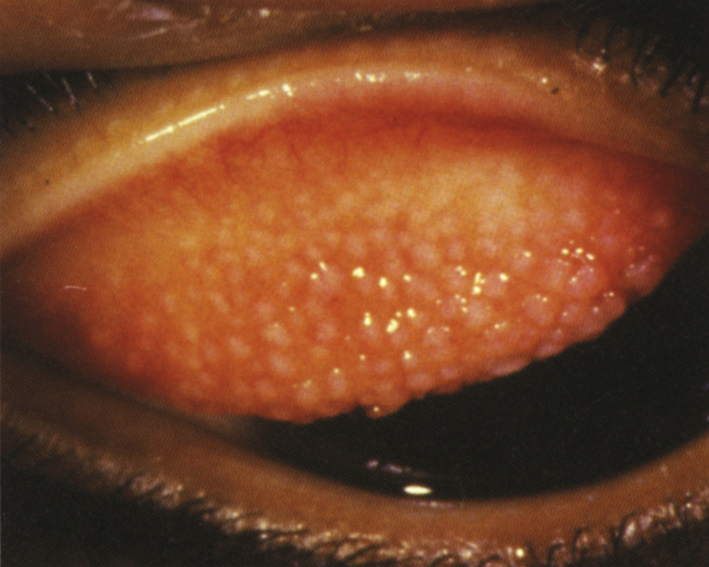
Itching, mucous discharge, contact lens intolerance, increased contact lens awareness, and excessive lens movement.
In 2 to 4 weeks. The patient may resume contact lens wear once the symptoms are resolved. Symptoms may improve before papillae resolve. Mast cell stabilizers are continued while the signs remain, and they may need to be used chronically to maintain contact lens tolerance. If topical steroids are used, they are usually slowly tapered and patients need to be monitored for steroid side effects.
 NOTE: NOTE: |
Giant papillary conjunctivitis can result not only from contact lens wear and atopic/vernal conjunctivitis, but also an exposed suture or an ocular prosthesis. Exposed sutures are removed. Prostheses should undergo routine cleaning and polishing. A coating can be placed on the prosthesis to reduce giant papillary conjunctivitis. Otherwise, these entities are treated as described earlier. |