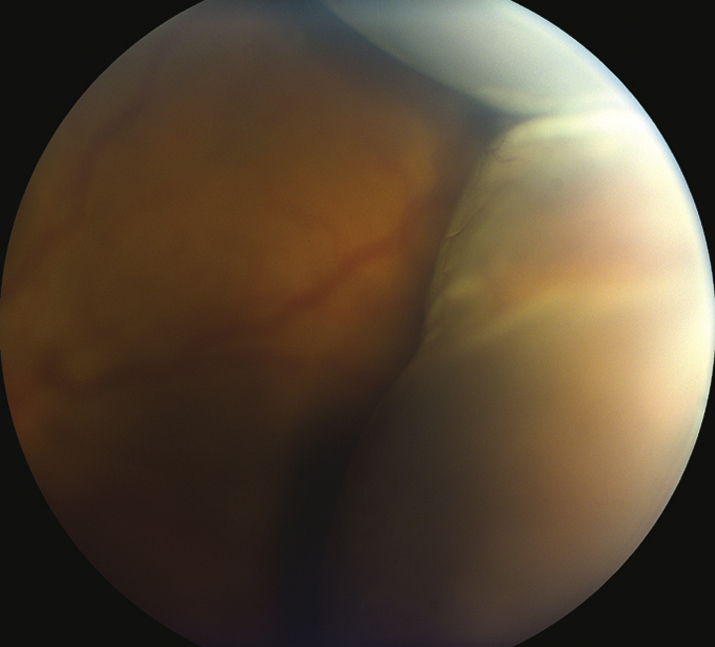
(See Figure 11.27.1.)
Critical
Smooth, bullous, orange-brown elevation of the retina and choroid that usually extends 360 degrees around the periphery in a lobular configuration. The ora serrata can be seen without scleral depression.
Other
Serous choroidal detachment: Low IOP (often <6 mm Hg), shallow anterior chamber with mild cell and flare, positive transillumination.
Hemorrhagic choroidal detachment: High IOP (if detachment is large), shallow anterior chamber with mild cell and flare, no transillumination.