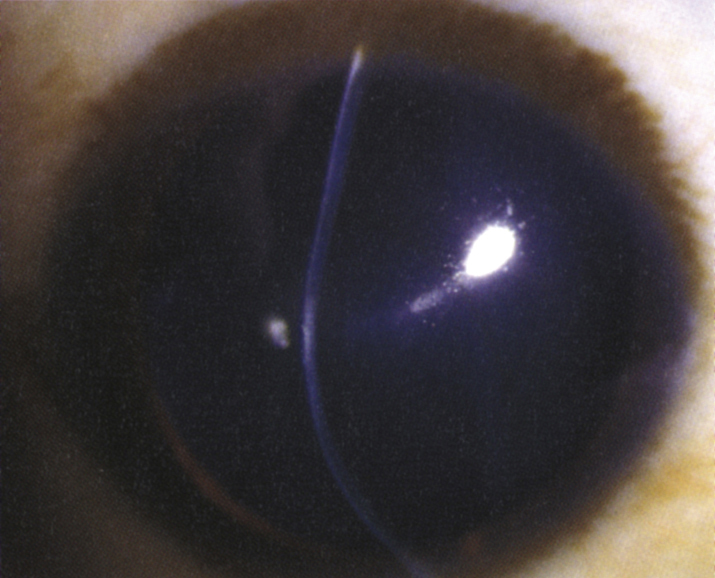
(See Figure 4.24.1.)
Critical
Non-inflammatory ectasia of corneal stroma seen as slowly progressive irregular astigmatism resulting from paracentral (usually inferior) thinning and bulging of the cornea (maximal thinning near the apex of the protrusion), vertical tension lines in the posterior cornea (Vogt striae), an irregular corneal retinoscopic reflex (scissor reflex), and egg-shaped mires on keratometry. Inferior steepening is seen on corneal topographic evaluation, and inferocentral posterior elevation and thinning are seen on tomographic evaluation. Almost always bilateral but often asymmetric.
Other
Fleischer ring (epithelial iron deposits at the base of the cone), bulging of the lower eyelid when looking downward (Munson sign), superficial apical scarring. Corneal hydrops (sudden development of corneal edema) results from a rupture in Descemet membrane (see Figure 4.24.2).
Associations
Keratoconus is associated with sleep apnea, floppy eyelid syndrome, Down syndrome, atopic disease, Turner syndrome, Leber congenital amaurosis, mitral valve prolapse, retinitis pigmentosa, and Marfan syndrome. It frequently is related to chronic eye rubbing. Family history of keratoconus is also a risk factor.