Decreased central vision; may be sudden or gradual.
Critical
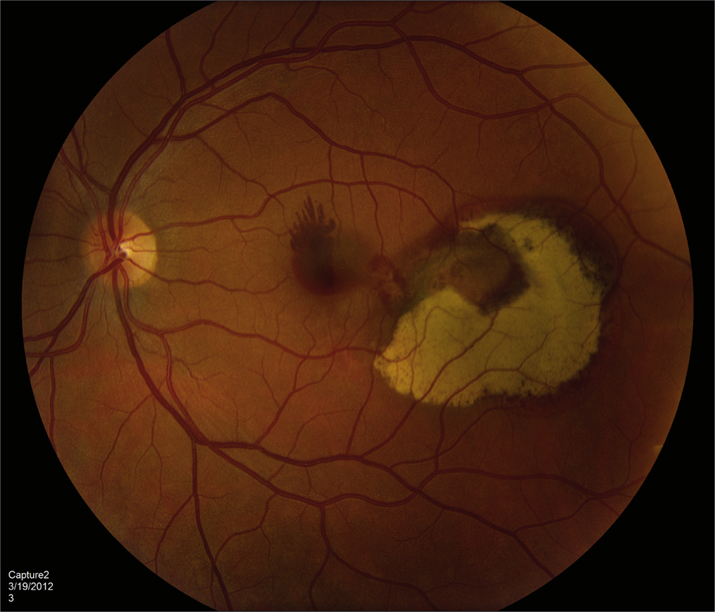
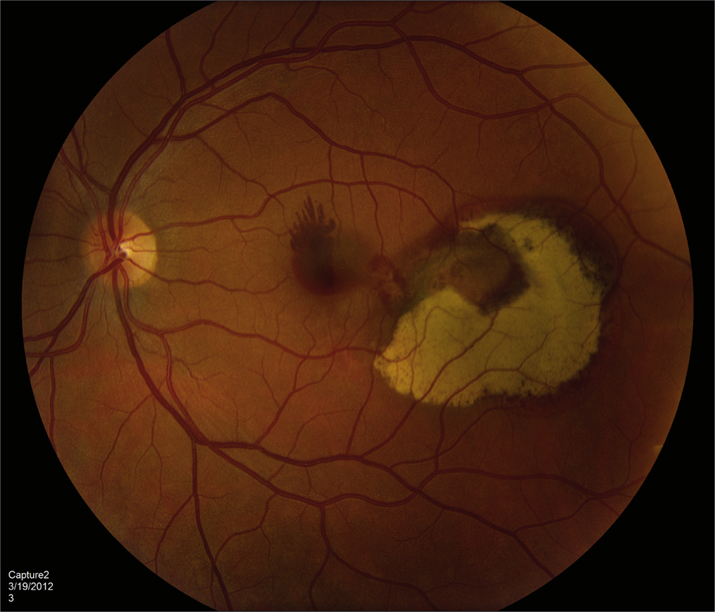
Subretinal red-orange, polyp-like lesions of the choroidal vasculature. Can be macular (more symptomatic) or peripapillary (see Figure 11.18.1).
11-18.1 Polypoidal choroidal vasculopathy OS.
Other
Bilateral subretinal and/or sub-RPE blood, VH, circinate subretinal exudates, subretinal fibrosis (disciform scar), SRF, atypical CNV, and multiple serous PEDs.
Risk Factors
More common in females, individuals of African or Asian descent, and in patients with HTN. Can occur at a younger age compared to neovascular AMD, but usually without significant drusen or geographic atrophy.
Cheung CMG, Lai TYY, Ruamviboonsuk P, et al. Polypoidal choroidal vasculopathy: definition, pathogenesis, diagnosis, and management. Ophthalmology. 2018;125(5):708-724.Koh A, Lai TYY, Takahashi K, et al. Efficacy and safety of ranibizumab with or without verteporfin photodynamic therapy for polypoidal choroidal vasculopathy: a randomized clinical trial. JAMA Ophthalmol. 2017;135:1206-1213.
Asymptomatic lesions may be observed and may resolve spontaneously. IPCV with exudation and/or hemorrhagic complications has been treated with anti-VEGF monotherapy, PDT, or a combination. The EVEREST-II and PLANET studies demonstrated level I evidence that anti-VEGF monotherapy as well as combination therapy give excellent functional visual outcomes in patients presenting with symptomatic IPCV. Thermal laser photocoagulation, feeder vessel treatment, and pneumatic displacement of large submacular hemorrhage have also been used with varying success.
The prognosis of IPCV is generally better than for neovascular AMD. Symptomatic or macular IPCV is followed every 1 to 2 months with periodic OCT, IVFA, and ICGA as needed for disease progression. Consider treatment, or retreatment, if symptomatic, persistent, or new leakage occurs.