Blind spot in the visual field or loss of vision, usually unilateral.
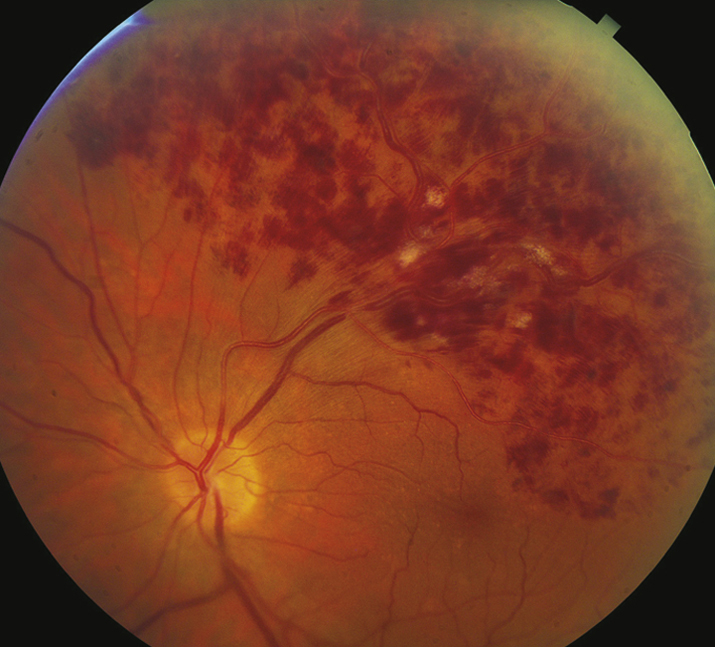
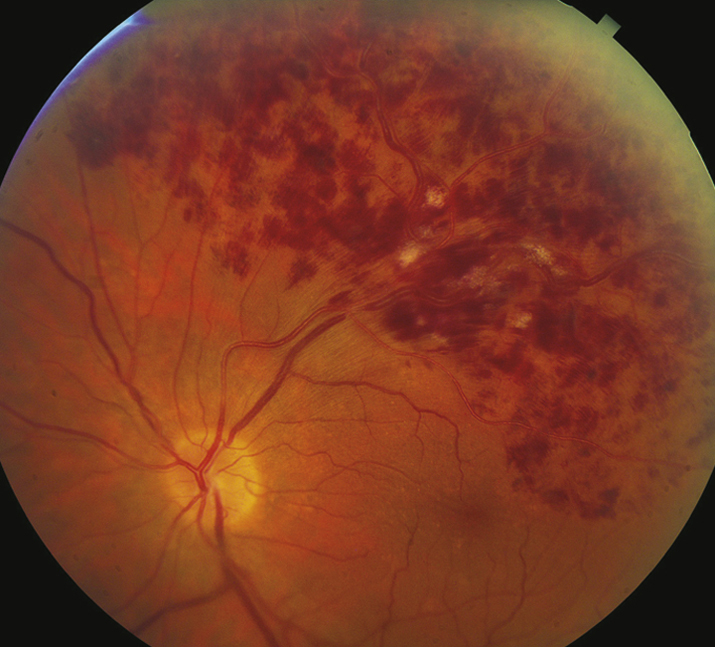
(See Figure 11.9.1.)
Critical
Superficial hemorrhages in a sector of the retina along a retinal vein. The hemorrhages usually do not cross the horizontal raphe (midline).
Other
CWSs, retinal edema, a dilated and tortuous retinal vein, narrowing and sheathing of the adjacent artery, retinal neovascularization, VH.
11-9.1 Branch retinal vein occlusion.
Disease of the adjacent arterial wall (usually secondary to HTN, arteriosclerosis, or diabetes) compresses the venous wall at a crossing point.
Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010;117(6):1102-1112.Varma R, Bressler NM, Suñer I, et al. Improved vision-related function after ranibizumab for macular edema after retinal vein occlusion: results from the BRAVO and CRUISE trials. Ophthalmology. 2012;119(10): 2108-2118.
In general, every month initially, with gradual interval taper based on vision, presence of ME, and treatment response. At each visit, the patient should be checked for neovascularization and ME.