Treatment should be instituted IMMEDIATELY, even before testing vision, unless an open globe is suspected.
This includes alkali (e.g., lye, cements, plasters, airbag powder, bleach, ammonia), acids (e.g., battery acid, pool cleaner, vinegar), solvents, detergents, and irritants (e.g., mace). |
- Copious but gentle irrigation using saline or Ringer lactate solution. Tap water can be used in the absence of these solutions and may be more efficacious in inhibiting elevated intracameral pH than normal saline for alkali burns. NEVER use acidic solutions to neutralize alkalis or vice versa as acid–base reactions themselves can generate harmful substrates and cause secondary thermal injuries. An eyelid speculum and topical anesthetic (e.g., proparacaine) may be placed prior to irrigation. Upper and lower fornices must be everted and irrigated. After exclusion of open globe injury, particulate matter should be flushed or manually removed. Manual use of intravenous tubing connected to an irrigation solution best facilitates the irrigation process.
- Wait 5 to 10 minutes after irrigation is stopped to allow the dilutant to be absorbed; then check the pH in the fornices using litmus paper. Irrigation is continued until neutral pH is achieved (i.e., 7.0 to 7.4). The pH should be read before the litmus paper dries.
- Conjunctival fornices should be swept with a moistened cotton-tipped applicator to remove any sequestered particles of caustic material and necrotic conjunctiva, especially in the case of a persistently abnormal pH. If there is concern for retained material, double eversion of the eyelids with Desmarres eyelid retractors may be performed to identify and remove particles in the deep fornix.
- Acidic or basic foreign bodies embedded in the conjunctiva, cornea, sclera, or surrounding tissues may require surgical excision.
The volume of irrigation fluid required to reach neutral pH varies with the chemical and with the duration of the chemical exposure. The volume required may range from a few liters to many liters (over 10 L). |
Mild to Moderate Burns
Signs
Critical
Corneal epithelial defects range from scattered superficial punctate keratopathy (SPK), to focal epithelial loss, to sloughing of the entire corneal epithelium. No significant areas of perilimbal ischemia are seen (i.e., no blanching of the conjunctival or episcleral vessels).
Other
Focal areas of conjunctival epithelial defect, chemosis, hyperemia, hemorrhages, or a combination of these; mild eyelid edema; mild anterior chamber (AC) reaction; first- and second-degree burns of the periocular skin with or without lash loss.
If you suspect a corneal epithelial defect but do not see one with fluorescein staining, repeat the fluorescein application to the eye. Sometimes the defect is slow to take up the dye. If the entire epithelium sloughs off, only Bowman membrane remains, which may take up fluorescein poorly. |
Workup
- History: Time of injury? Specific type of chemical? Time from exposure until irrigation started? Duration, amount, and type of irrigation? Eye protection? Sample of agent, package/label, or material safety data sheets are helpful in identifying and treating the exposing agent.
- Slit lamp examination with fluorescein staining. Eyelid eversion to search for foreign bodies. Evaluate for and diagram conjunctival and corneal epithelial defects and ulcerations. Check the intraocular pressure (IOP). In the presence of a distorted cornea, IOP may be most accurately measured with a Tono-Pen, pneumotonometer, or rebound tonometer. Gentle palpation may be used if necessary.
Treatment
- See EMERGENCY TREATMENT above.
- Consider cycloplegic (e.g., cyclopentolate 1% or 2%, homatropine 5% b.i.d. to t.i.d.) if significant photophobia, pain, or AC inflammation. If limbal ischemia is suspected, avoid phenylephrine because of its vasoconstrictive properties.
- Frequent (e.g., q1–2h while awake) use of preservative-free artificial tear drops, artificial tear, or antibiotic ointment (e.g., erythromycin, bacitracin) depending on presence and size of corneal and/or conjunctival epithelial defects.
- Consider topical steroids (e.g., prednisolone acetate 1% q.i.d.) as adjunctive treatment with topical antibiotic (e.g., trimethoprim/polymyxin B or fluoroquinolone drops q.i.d.) for a week even if epithelial defect is present, especially for an alkali injury.
- Oral pain medication (e.g., acetaminophen with or without codeine) as needed.
- If IOP is elevated, acetazolamide 250 mg p.o. q.i.d., acetazolamide 500 mg sequel p.o. b.i.d., or methazolamide 25 to 50 mg p.o. b.i.d. or t.i.d. may be given. Electrolytes, especially potassium, should be monitored in patients on these medications. Add a topical beta-blocker (e.g., timolol 0.5% b.i.d.) if additional IOP control is required. Alpha-agonists should be avoided because of their vasoconstrictive properties, especially if limbal ischemia is present.
Follow Up
Initially daily, then every few days until corneal epithelial defect is healed. Topical steroids should be initiated if there is significant inflammation. Monitor for corneal epithelial breakdown, stromal thinning, and infection.
Severe Burns
Signs (in addition to the above)
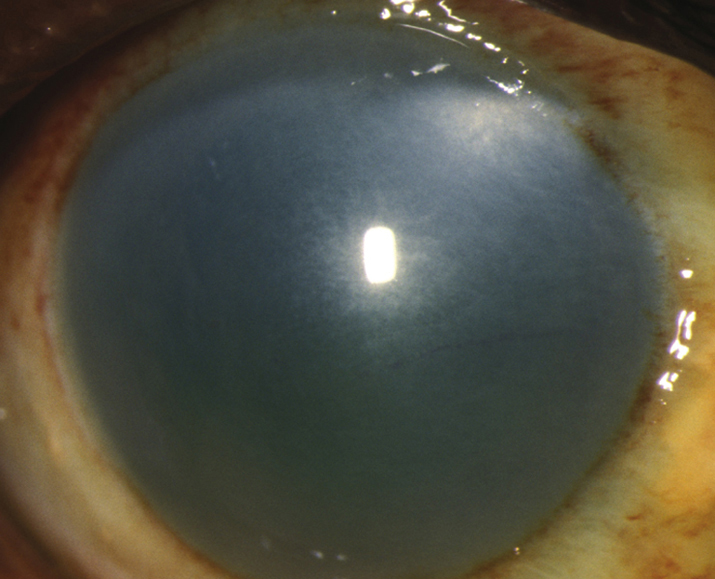
(See Figure 3.1.1.)
Critical
Pronounced chemosis and conjunctival blanching, corneal edema and opacification, a moderate to severe AC reaction (may not be appreciated if the cornea is opaque).
Other
Increased IOP, second- and third-degree burns of the surrounding skin, and local necrotic retinopathy as a result of direct penetration of alkali through the sclera.
Workup
Same as for mild-to-moderate burns.
Treatment
- See EMERGENCY TREATMENT above.
- Hospital admission may be needed for close monitoring of IOP and corneal healing.
- Debride necrotic tissue containing foreign matter.
- Cycloplegic (e.g., cyclopentolate 1% or 2% b.i.d. to t.i.d., homatropine 5% b.i.d. to t.i.d., or atropine 1% daily to b.i.d.). Avoid phenylephrine due to vasoconstriction.
- Topical antibiotic (e.g., trimethoprim/polymyxin B or fluoroquinolone drops q.i.d.; erythromycin or bacitracin ointment q.i.d. to q2h while awake). Caution with ciprofloxacin and large epithelial defects as it can precipitate in the cornea.
- Topical steroid (e.g., prednisolone acetate 1% or dexamethasone 0.1% q.i.d. to q2h while awake) with concurrent antibiotic coverage even in the presence of an epithelial defect, especially if significant AC or corneal inflammation is present. May use a combination antibiotic/steroid such as tobramycin/dexamethasone drops or ointment q1–2h while awake.
- IOP-lowering medications as above if the IOP is increased or cannot be determined.
- Frequent (e.g., q1h while awake) use of preservative-free artificial tears or gel if not using frequent ointments.
- Oral tetracyclines and vitamin C may also reduce collagenolysis and stromal melting (e.g., doxycycline 100 mg p.o. b.i.d. and vitamin C 1,000 mg p.o. daily).
- Lysis of conjunctival adhesions b.i.d. by sweeping the fornices may be helpful. If symblepharon begins to form despite attempted lysis, consider using an amniotic membrane ring (e.g., ProKera Plus Ring) or scleral shell to maintain the fornices.
- In severe cases with large areas of epithelial loss on the bulbar and forniceal conjunctival surfaces, consider suturing a very large amniotic membrane into the fornices.
- Other considerations:
- For poorly healing epithelial defects, a therapeutic soft contact lens, collagen shield, amniotic membrane graft (e.g., sutured/glued or self-retained membrane), or tarsorrhaphy may be considered.
- Ascorbate and citrate for alkali burns has been reported to speed healing time and allow better visual outcome. Administration has been studied intravenously (i.v.), orally (ascorbate 500 to 2,000 mg daily), and topically (ascorbate 10% q1h). Caution in patients with renal compromise secondary to potential renal toxicity.
- If any melting of the cornea occurs, other collagenase inhibitors may be used (e.g., acetylcysteine 10% to 20% drops q4h while awake).
- Topical biologic fluids including autologous serum tears, platelet-rich plasma, umbilical cord serum, and amniotic membrane suspensions may be useful to promote epithelialization.
- If the melting progresses (or the cornea perforates), consider cyanoacrylate tissue adhesive. An emergency patch graft or corneal transplantation may be necessary; however, the prognosis for grafts is better if performed long after initial injury (over 12 to 18 months).
Follow Up
These patients need to be monitored closely, either as inpatients or daily initially as outpatients. Topical steroids should be tapered after 7 to 14 days, because they can promote corneal melting. If prolonged anti-inflammatory treatment is needed, consider switching to medroxyprogesterone acetate 1% to prevent corneal stromal melting. Long-term use of preservative-free artificial tears q1–6h and lubricating ointments q.h.s. to q.i.d. may be required. A severely dry eye may require a tarsorrhaphy or a conjunctival flap. Conjunctival or limbal stem cell transplantation from the fellow eye may be performed in unilateral injuries that fail to heal within several weeks to several months.
Super Glue (Cyanoacrylate) Injury to the Eye
Rapid-setting super glues harden quickly on contact with moisture. |
Treatment
- If the eyelids are glued together, they can often be separated with gentle traction. Lashes may need to be cut to separate the eyelids. Misdirected lashes, hardened glue mechanically rubbing the cornea, and glue adherent to the cornea should be carefully removed with fine forceps. Copious irrigation with warm normal saline, warm compresses, or ointment may be used to loosen hardened glue on the eyelids, eyelashes, cornea, or conjunctiva.
- Epithelial defects are treated as corneal abrasions (see 3.2, CORNEAL ABRASION).
- Warm compresses q.i.d. may help remove any remaining glue stuck in the lashes that did not require urgent removal.
- If complete removal of glue is not possible from the eyelid margin, a bandage contact lens may be applied along with topical antibiotic drop therapy until the glue falls off.
Follow Up
Initially daily, then every few days until all corneal epithelial defects are healed.