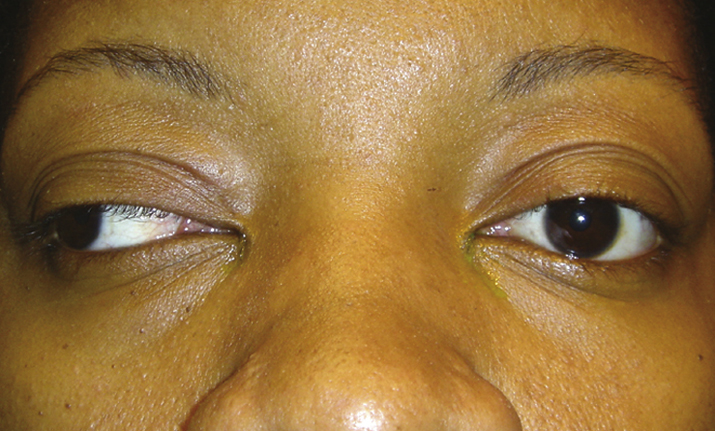
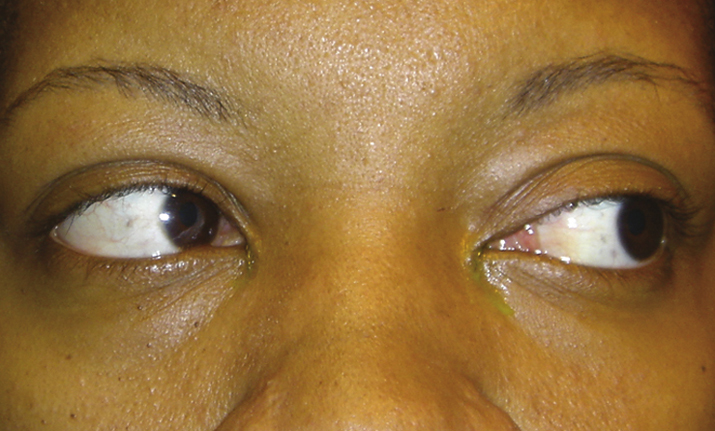
(See Figures 10.13.1 and 10.13.2.).
Critical
Weakness or paralysis of adduction, with horizontal jerk nystagmus of the abducting eye.
INO is localized to the side with the weak adduction. |
Other
May be unilateral or bilateral (WEBINO: “wall-eyed,” bilateral INO). Upbeat nystagmus on upgaze may occur when INO is unilateral or bilateral. The involved eye can sometimes turn in when attempting to read (intact convergence). A skew deviation (relatively comitant vertical deviation not caused by neuromuscular junction disease or intraorbital pathology) may be present; brainstem and posterior fossa pathology should be ruled out. With skew deviation, the three-step test cannot isolate a specific muscle. See 10.7, ISOLATED FOURTH CRANIAL NERVE PALSY. In addition, presence of other neurologic signs, including gaze-evoked nystagmus, gaze palsy, dysarthria, ataxia, and hemiplegia, favors skew deviation rather than fourth cranial nerve palsy.