Decreased vision, foreign body sensation, photophobia, and corneal whitening; may be asymptomatic.
Critical
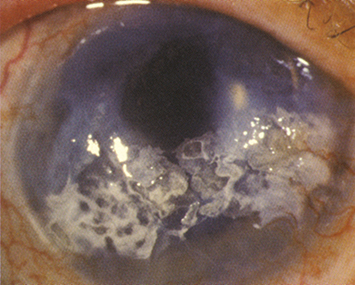
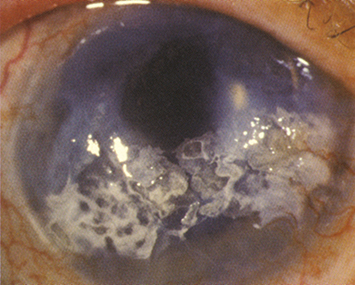
Gray-white anterior corneal plaque of calcium at the level of Bowman membrane, typically within the interpalpebral fissure, and separated from the limbus by clear cornea. Lucid spaces may be present in the plaque (due to corneal nerves penetrating through Bowman layer), giving it a Swiss cheese appearance. The plaque usually begins at the 3-o’clock and 9-o’clock positions, adjacent to the limbus (see Figure 4.11.1).
Figure 4.11.1: Band keratopathy.
Other
May have other signs of chronic eye disease.
More Common
Chronic uveitis (e.g., juvenile idiopathic arthritis [JIA]), IK, corneal edema, trauma, phthisis bulbi, long-standing glaucoma, dry eye, ocular surgery (especially retinal detachment repair with silicone oil), and idiopathic.
Less Common
Hypercalcemia (may result from hyperparathyroidism, renal failure, sarcoidosis, multiple myeloma, Paget disease of bone, vitamin D excess, etc.), hyperphosphatemia, gout, sarcoidosis, corneal dystrophy, myotonic dystrophy, long-term exposure to irritants (e.g., mercury fumes), and other causes.
Mild (e.g., Foreign Body Sensation)
Artificial tears, preferably preservative-free, four to six times per day and artificial tear ointment q.h.s. to q.i.d. as needed, add antibiotic ointment (e.g., bacitracin, bacitracin-polymyxin or erythromycin) if irregular epithelium or epithelial defects over calcium deposition. Consider a bandage soft contact lens for comfort.
Severe (e.g., Obstruction of Vision, Irritation Not Relieved by Lubricants, Cosmetic Problem)
Removal of the calcium plaque may be performed at the slit lamp or under the operating microscope by chelation using disodium ethylenediamine tetraacetic acid (EDTA):
Disodium EDTA 3% to 4% is obtained from a compounding pharmacy.
Anesthetize the eye with a topical anesthetic (e.g., proparacaine, lidocaine gel) and place an eyelid speculum.
Debride the corneal epithelium overlying the calcium with a sterile blade or a sterile cotton-tipped applicator.
Apply a cellulose sponge, corneal light shield, or cotton swab saturated with the EDTA solution over the band keratopathy until the calcium clears (which may take 10 to 60 minutes).
Irrigate with normal saline, apply an antibiotic drop, a cycloplegic drop (e.g., cyclopentolate 1% to 2%), and place a bandage soft contact lens. Prescribe a topical antibiotic drop (e.g., moxifloxacin, gatifloxacin q.i.d.) until the epithelium has healed.
Consider giving the patient a systemic analgesic (e.g., acetaminophen with codeine).
|
 NOTE NOTEIn order to minimize recurrence of band keratopathy after treatment, it is important to also treat or manage the underlying cause to the best extent possible. |