Sudden, painless visual loss of moderate degree, initially unilateral, but may become bilateral. Typically occurs in patients 40 to 60 years of age, but well-documented cases have been reported in patients in their teenage years. In younger patients, NAION should be suspected when painless visual loss develops with a contralateral “disc at risk” (i.e., crowded disc with small or absent optic cup [cup:disc ratio less than 0.3]) and normal MRI scan. The visual deficit may improve. Hyperlipidemia, labile hypertension, and sleep apnea are the common risk factors for younger patients.
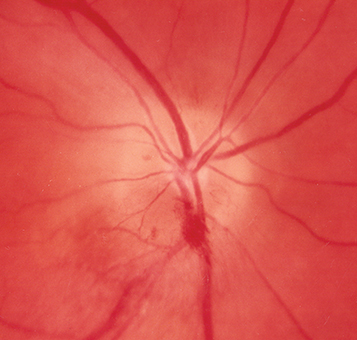
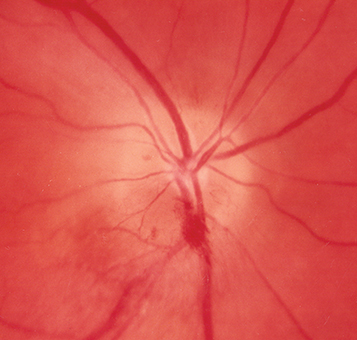
(See Figure 10.18.1.)
Figure 10.18.1: Nonarteritic ischemic optic neuropathy with segmental disc edema and hemorrhage.
Critical
Afferent pupillary defect, pale disc swelling (often segmental), flame-shaped hemorrhages, normal ESR and CRP.
Nonprogressive NAION: Sudden initial decrease in visual acuity and visual field, which stabilizes.
Progressive NAION: Sudden initial decrease in visual acuity and visual field followed by worsening in visual acuity or visual field days to weeks later. As many as 35% of NAION cases may be progressive.
Other
Reduced color vision, altitudinal or central visual field defect, optic atrophy without cupping (segmental or diffuse) after the edema resolves. Crowded or congenitally anomalous disc with small or absent cup in fellow eye.
See 10.17, Arteritic Ischemic Optic Neuropathy (Giant Cell Arteritis).
Idiopathic: Arteriosclerosis, diabetes, hypertension, hyperlipidemia, hyperhomocysteinemia, anemia, and sleep apnea are associated risk factors, but causation has never been proven. Relative nocturnal hypotension may play a role, especially in patients taking antihypertensive medication. We recommend avoiding antihypertensive medications at night.
|
 NOTE NOTECurrently, phosphodiesterase-5 inhibitors (e.g., sildenafil, vardenafil, and tadalafil) often used for erectile dysfunction have not been proven to cause NAION. However, the FDA has issued a warning regarding a possible association with these medications and NAION. It is recommended that patients with risk factors for NAION (listed previously) be counseled against the use of these medications. |