Eye pain, decreased vision, or may be asymptomatic; often suggestive history (e.g., hammering metal or sharp object entering globe).
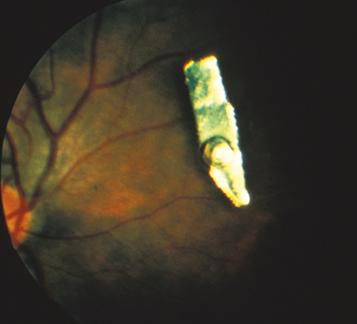
(See Figure 3.11.1.)
May have a clinically detectable corneal or scleral perforation site, hole in the iris, focal lens opacity, or an IOFB. IOFBs are often seen on CT scan (thin cuts), B-scan US, and/or UBM.
See 3.10, Ruptured Globe and Penetrating Ocular Injury. Also, microcystic (epithelial) edema of the peripheral cornea (a clue that a foreign body may be hidden in the AC angle in the same sector of the eye). Long-standing iron-containing IOFBs may cause siderosis, manifesting as anisocoria, heterochromia, corneal endothelial and epithelial deposits, anterior subcapsular cataracts, lens dislocation, retinopathy, and optic atrophy.
Frequently produce severe inflammatory reactions and may encapsulate within 24 hours if on the retina.
Inert foreign bodies: Carbon, gold, coal, glass, lead, gypsum plaster, platinum, porcelain, rubber, silver, and stone. Brass, an alloy of copper and zinc, is also relatively nontoxic. However, even inert foreign bodies can be toxic because of a coating or chemical additive. Most ball bearings (BBs) and gunshot pellets are made of 80% to 90% lead and 10% to 20% iron.
History: Mechanism of trauma? Use of protective eyewear? Composition of foreign body? Time of last meal?
Perform ocular examination, including visual acuity and careful evaluation of globe integrity. If there is an obvious perforation site, the remainder of the examination may be deferred until surgery. If there does not appear to be a risk of extrusion of intraocular contents, the globe is inspected gently to localize the perforation site and to detect the foreign body.
Slit-lamp examination; search the AC and iris for a foreign body and look for an iris TID. Examine the lens for disruption, cataract, or embedded foreign body. Check IOP.
Consider careful gonioscopy of the AC angle if no wound leak can be detected and the globe appears intact.
Obtain a CT scan of the orbits and brain (coronal, axial, and parasagittal views with no larger than 1-mm sections through the orbits). MRI is contraindicated in the presence of a metallic foreign body. It may be difficult to visualize wood, glass, or plastic on a CT scan, especially acutely. Suspicion of a nonmetallic IOFB should specifically be mentioned to the reading radiologist.
Gentle B-scan US of the globe and orbit. Intraocular air can mimic a foreign body. Consider UBM to inspect the AC if IOFB is not visible on clinical examination (e.g., foreign body in the AC angle or sulcus). These steps should be deferred in patients with a definitive or suspected anterior rupture given the risk for extrusion of intraocular contents.
Determine whether the foreign body is magnetic (e.g., examine material from which the foreign body came).
Place a protective rigid shield over the involved eye. Do not patch the eye.
Tetanus toxoid as needed (see Appendix 2, Tetanus Prophylaxis).
Broad-spectrum gram-positive and gram-negative antibiotic coverage (e.g., vancomycin 1 g i.v. q12h and ceftazidime 1 g i.v. q12h; alternatively ciprofloxacin 400 mg i.v. q12h or moxifloxacin 400 mg i.v. daily).
Cycloplegia (e.g., atropine 1% b.i.d.) for posterior-segment foreign bodies.
Urgent surgical removal of any acute IOFB is advisable to reduce the risk of infection and development of proliferative vitreoretinopathy (PVR). For some metallic foreign bodies, a magnet may be useful during surgical extraction. Copper or contaminated foreign bodies require especially urgent removal. If urgent removal cannot be performed, intravitreal and systemic antibiotics can help reduce the risk of endophthalmitis. A chronic IOFB may require removal if associated with severe recurrent inflammation, if in the visual axis, or if causing siderosis.
If endophthalmitis is present, treat as per 12.16, Traumatic Endophthalmitis.
Observe the patient closely in the hospital for signs of inflammation or infection. If the surgeon is uncertain as to whether the foreign body was entirely removed, postoperative imaging should be considered with CT, B-scan US, or UBM as above. Periodic follow-up for years is required; watch for a delayed inflammatory reaction in both the traumatic and nontraumatic eye. When an IOFB is left in place, an electroretinogram (ERG) should be obtained as soon as it can be done safely. Serial ERGs should be followed to look for toxic retinopathy, which will often reverse if the foreign body is removed.