Recurrent attacks of acute ocular pain, photophobia, foreign body sensation, and tearing. The pain may awaken patients from sleep or occur spontaneously with eye opening. There is often a history of prior corneal abrasion in the affected eye.
Critical
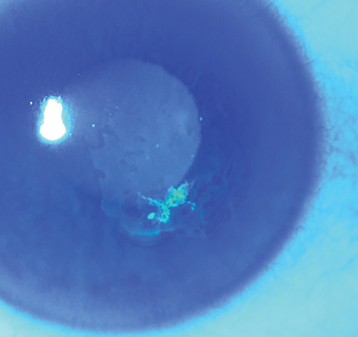
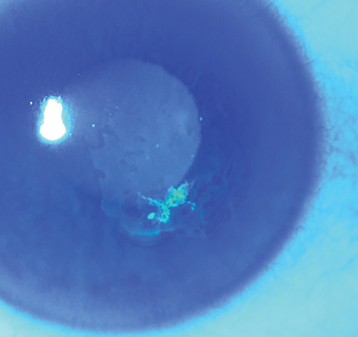
Localized irregularity with loose corneal epithelium (fluorescein dye may outline the area with negative or positive staining) or a corneal abrasion (see Figure 4.2.1). Epithelial changes may resolve within hours of the onset of symptoms so abnormalities may be subtle or absent when the patient is examined.
Figure 4.2.1: Resolving epithelial defect with paracentral area of negative fluorescein staining in recurrent corneal erosion.
Other
Corneal epithelial dots or microcysts, a fingerprint pattern, or map-like lines may be seen in both eyes if epithelial basement membrane (map–dot–fingerprint) dystrophy is present. These findings may also be seen unilaterally and focally in any eye that has recurrent erosions.
Damage to the corneal epithelium or epithelial basement membrane from one of the following:
Anterior corneal dystrophy: Epithelial basement membrane (most common), Reis–Bücklers, Thiel–Behnke, and Meesmann dystrophies.
Previous traumatic corneal abrasion: Injury may have been years before the current presentation.
Stromal corneal dystrophy: Lattice, granular, and macular dystrophies.
Corneal degeneration: Band keratopathy, Salzmann nodular degeneration.
Keratorefractive surgery, corneal transplant surgery, cataract surgery, or any surgery in which the corneal epithelium is removed (either therapeutically or for visualization).
Every 2 to 5 days until the epithelium has healed, and then every 1 to 3 months, depending on the severity and frequency of the episodes. It is important to educate patients that persistent use of lubricating ointment (5% sodium chloride or tear ointment every night) for 3 to 6 months following the initial healing process reduces the chance of recurrence.