Itching, mucous discharge, contact lens intolerance, increased contact lens awareness, and excessive lens movement.
Critical
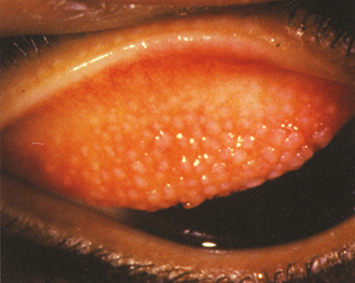
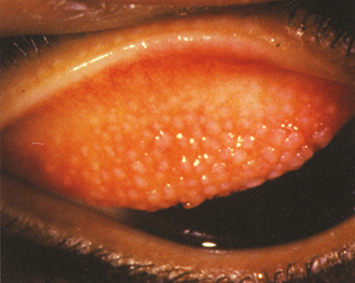
Giant papillae on the superior tarsal conjunctiva (see Figure 4.22.1).
Figure 4.22.1: Giant papillary conjunctivitis.
|
 NOTE NOTEThe upper eyelid must be everted to make the diagnosis. Upper eyelid eversion should be part of the routine eye examination in any patient who wears contact lenses. |
Other
Contact lens coatings, high-riding lens, mild conjunctival injection, ptosis (usually a late sign).
Modify contact lens regimen as follows:
Mild-to-Moderate Giant Papillary Conjunctivitis
Replace and refit the contact lens. Consider planned replacement or daily-disposable lenses (daily-disposable lenses preferred).
Reduce contact lens wearing time (switch from extended-wear contact lens to daily-wear).
Have the patient clean the lenses more thoroughly, preferably by using preservative-free solutions, preservative-free saline, and a hydrogen peroxide–based disinfection system.
Increase enzyme use (use at least every week).
Severe Giant Papillary Conjunctivitis
Suspend contact lens wear.
Restart with a new contact lens when the symptoms and signs clear (usually 1 to 4 months), preferably with daily-disposable soft contact lenses.
Careful lens hygiene as described earlier.
Start a topical mast cell stabilizer or combination antihistamine/mast cell stabilizer (e.g., pemirolast, nedocromil, lodoxamide, cromolyn, alcaftadine, olopatadine, bepotastine, or epinastine).
In unusually severe cases, short-term use of a low-dose topical steroid may be considered (e.g., loteprednol 0.5%, fluorometholone 0.1%, or fluorometholone acetate 0.1% q.i.d.). Contact lenses should not be worn while using a topical steroid.
Steroid-sparing topical anti-inflammatory agents such as cyclosporine 0.05% to 0.1% or lifitegrast 5% may be beneficial if long-term treatment is needed.
In 2 to 4 weeks. The patient may resume contact lens wear once the symptoms are resolved. Symptoms may improve before papillae resolve. Mast cell stabilizers are continued while the signs remain, and they may need to be used chronically to maintain contact lens tolerance. If topical steroids are used, they are usually slowly tapered and patients need to be monitored for steroid side effects.
|
 NOTE NOTEGiant papillary conjunctivitis can result not only from contact lens wear and atopic/vernal conjunctivitis, but also from an exposed suture or an ocular prosthesis. Exposed sutures are removed. Prostheses should undergo routine cleaning and polishing. A coating can be placed on the prosthesis to reduce giant papillary conjunctivitis. Otherwise, these entities are treated as described earlier. |