Acute retinal break: Flashes of light, floaters (“cobwebs,” “hair,” or “film” that changes position with eye movement) with or without visual acuity changes. Can be identical to PVD symptoms, though may be more substantial.
Chronic retinal breaks or atrophic retinal holes: Usually asymptomatic.
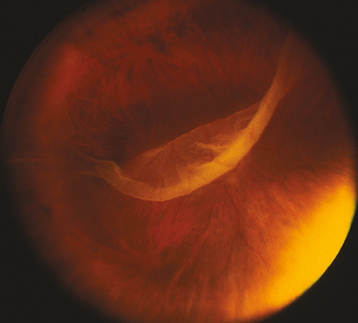
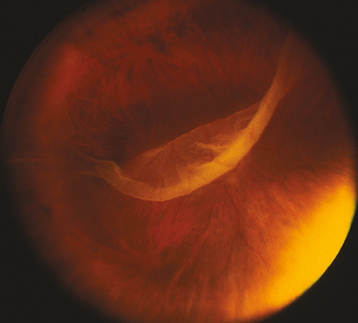
(See Figure 11.2.1.)
Figure 11.2.1: Giant retinal tear.
Critical
A full-thickness retinal defect, usually seen in the periphery.
Other
Acute retinal break: Pigmented cells in the anterior vitreous, VH, PVD, retinal flap, subretinal fluid (SRF), or an operculum (a free-floating piece of retina suspended above an RT).
Chronic retinal break: Surrounding pigmentation ring or demarcation line between attached and detached retina and signs (but not necessarily symptoms) of an acute retinal break.
Predisposing Conditions
Lattice degeneration, high myopia, aphakia, pseudophakia, history of previous retinal break or detachment in the fellow eye, family history of retinal break or detachment, collagen vascular disorders, and trauma.
Complete ocular examination with a slit lamp and indirect ophthalmoscopy of both eyes with scleral depression. After trauma, scleral depression may be gently performed once open globe injury has been ruled out. B-scan US may be helpful when the retina is not visible (e.g., VH, dense cataract, etc.).
In general, laser therapy or cryotherapy is required within 24 hours for acute retinal breaks. Treatment may be less urgent for chronic breaks. However, each case must be individualized based on patient risk factors. We follow these general guidelines:
Treatment is recommended for:
Acute symptomatic break (e.g., a horseshoe or operculated tear).
Acute traumatic break (including a dialysis).
Asymptomatic retinal break that is large (e.g., ≥1.5 mm), above the horizontal meridian, or both, particularly in the absence of PVD.
Asymptomatic retinal break in an aphakic or pseudophakic eye, a highly myopic eye, or an eye in which the involved or contralateral eye has had an RD.