Procedure Steps (See Video: Anterior Chamber Paracentesis)
Place a drop of topical anesthetic (e.g., proparacaine) on the surface of the eye.
Place a drop of topical 5% povidone-iodine on the surface of the eye and allow it to sit on the globe for at least 30 to 60 seconds.
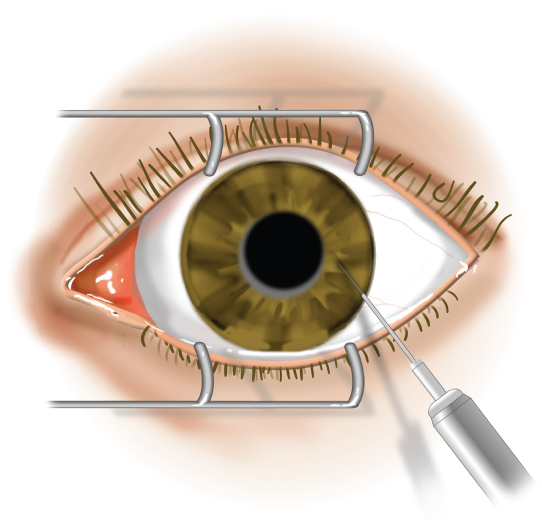
In an eye with normal or elevated intraocular pressure, fixation forceps are not needed.
In eyes with intraocular pressure <8 mm Hg, fixation forceps may be necessary. Anesthetize the base of the lateral rectus muscle by holding a cotton-tipped applicator dipped in the topical anesthetic against the muscle for 1 minute. Grasp the base of the lateral rectus muscle with fixation forceps at the anesthetized site.
Use a 30-gauge short needle on a syringe and remove the plunger.
Enter the eye at an area with a sufficiently formed anterior chamber. Keep the bevel of the needle pointing anteriorly (toward the epithelium) and away from the lens. Keep the tip of the needle over the iris (not the lens) when entering the anterior chamber (see Figure A.13.1).
Leave the tip of the needle in the anterior chamber for about 2 to 3 seconds. Aqueous will passively egress into the plungerless syringe.
Withdraw the needle and place a drop of antibiotic on the eye (e.g., gatifloxacin or moxifloxacin). Consider topical antibiotics q.i.d. for 4 to 7 days.