Author(s): Nancy M.Wu, Jason M.Lewis
- General considerations
- Intraocular pressure (IOP; normal range 10-22 mm Hg) is principally determined by (1) aqueous volume (the rate of production of aqueous humor in relation to its rate of drainage) and (2) the blood volume within vessels of the eye. Owing to scleral inelasticity, small changes in volume result in large changes in IOP.
- Factors that may increase IOP include hypertension, hypercarbia, hypoxia, laryngoscopy and endotracheal intubation, venous congestion, vomiting, coughing, straining, bucking, external pressure on the eye, succinylcholine, and ketamine.
- Factors that may decrease IOP include hypocarbia, hypothermia, central nervous system (CNS) depressants, ganglionic blockers, most volatile and intravenous (IV) anesthetics, nondepolarizing neuromuscular blockade (NMB), mannitol, diuretics, acetazolamide, and head elevation.
- Glaucoma
- Open-angle glaucoma usually arises from chronic obstruction of the aqueous humor drainage and is characterized by a progressive, insidious course that may be painless.
- Closed-angle glaucoma results from acute aqueous outflow obstruction due to a narrowing of the anterior chamber. This occurs as a result of pupillary dilation or lens edema and is painful.
- Oculocardiac reflex
- The oculocardiac reflex (OCR) is mediated by afferent impulses via the ophthalmic branch (cranial nerve [CN] VI) of the trigeminal nerve and efferents from the vagus nerve (CN X). Increases in IOP, manipulation of the globe, or traction on the extrinsic eye muscles may result in bradycardia, atrioventricular block, ventricular ectopy, or asystole. Administration of ocular regional anesthesia may also elicit this response. OCR is common in patients undergoing strabismus surgery.
- The OCR should be promptly treated by cessation of the stimulus. Atropine (0.01-0.02 mg/kg IV) may be administered if bradyarrhythmias persist. The reflex fatigues quickly with repeated stimulation. However, if the reflex persists, infiltration of local anesthetic near the extrinsic eye muscles or placement of a peribulbar or retrobulbar block is effective. Alternatively, pretreatment with atropine or glycopyrrolate can be helpful in preventing the reflex.
- Commonly used drugs
- Topical. Most ophthalmic medications are highly concentrated solutions that are administered topically and may produce systemic effects.
- Mydriatics
- Phenylephrine eye drops may cause hypertension and reflex bradycardia, especially when administered as a 10% solution. For this reason, a 2.5% solution is commonly used. It dilates the pupil and constricts periocular blood vessels.
- Cyclopentolate, atropine, and scopolamine are anticholinergic agents that can produce CNS toxicity (eg, confusion seizures), particularly in the elderly and young. Additional effects include flushing, thirst, dry skin, and tachycardia.
- Epinephrine 2% topical solution reduces IOP in open-angle glaucoma by decreasing aqueous secretion while improving outflow. Complications can include hypertension, tachycardia, dysrhythmias, and syncope.
- Miotics. Cholinergic drugs (eg, pilocarpine 0.25%-4% solution) may produce bradycardia, salivation, bronchorrhea, and diaphoresis.
- Drugs that decrease IOP
- β-Adrenergic antagonists (eg, timolol or betaxolol) may cause bradycardia, hypotension, congestive heart failure, and bronchospasm.
- Anticholinesterases, such as echothiophate, depress plasma cholinesterase activity for 2 to 4 weeks and may prolong recovery from succinylcholine and mivacurium (not available in the United States).
- Apraclonidine, an α2-adrenergic agonist, is used to reduce IOP by decreasing aqueous production and improving outflow. Systemic side effects may include sedation and drowsiness. Rebound hypertension may result from acute withdrawal after chronic therapy.
- Mydriatics
- Systemic
Acetazolamide, a carbonic anhydrase inhibitor, is administered systemically to decrease aqueous humor secretion, thus lowering IOP. Chronic use can lead to the development of hyponatremia, hypokalemia, and metabolic acidosis.
- Topical. Most ophthalmic medications are highly concentrated solutions that are administered topically and may produce systemic effects.
- Intraocular pressure (IOP; normal range 10-22 mm Hg) is principally determined by (1) aqueous volume (the rate of production of aqueous humor in relation to its rate of drainage) and (2) the blood volume within vessels of the eye. Owing to scleral inelasticity, small changes in volume result in large changes in IOP.
- Anesthetic management
- Preoperative evaluation. Patients undergoing eye surgery are often at the extremes of age, presenting with significant concomitant diseases that may require careful evaluation (eg, the formerly premature infant with bronchopulmonary dysplasia for retinal surgery or the elderly patient with cardiovascular disease for cataract excision). Preoperative testing should be dictated by medical comorbidities. However, recent evidence indicates that even patients with complex conditions undergoing low-risk eye surgery without routine testing have no increased risk of adverse events as compared with those who do undergo evaluation.
- Avoidance of coughing, sudden movement, or straining is essential. Unexpected patient or eye movements during delicate microscopic intraocular surgery can lead to increased IOP, choroidal hemorrhage, expulsion of vitreous material, or loss of vision.
- Regional anesthesia
- Ophthalmic procedures such as cataract extraction, corneal transplant, anterior chamber irrigation, oculoplastic procedures, and even vitreoretinal procedures lasting 3 to 4 hours can be performed under regional anesthesia and light sedation.
- Patient cooperation and lack of head motion are important for the success of this technique. Patients who are unable to participate owing to extremes of age, impaired hearing, psychiatric illness, language barrier, inability to tolerate supine position or maintain a relatively motionless position may not be candidates for regional anesthesia for delicate eye surgery.
- Advantages of regional anesthesia include a lower incidence of coughing, straining, and emesis on emergence, reliable postoperative analgesia, lower perioperative morbidity, and earlier discharge compared with general anesthesia (GA).
- IV sedation may be used perioperatively. Midazolam (0.25-1 mg IV), fentanyl (10-50 μg IV), remifentanil (0.25-1 μg/kg IV), or propofol (5-20 μg IV) can be administered just before the regional injection. Patients should have standard ASA monitors during regional block placement and receive supplemental oxygen if indicated.
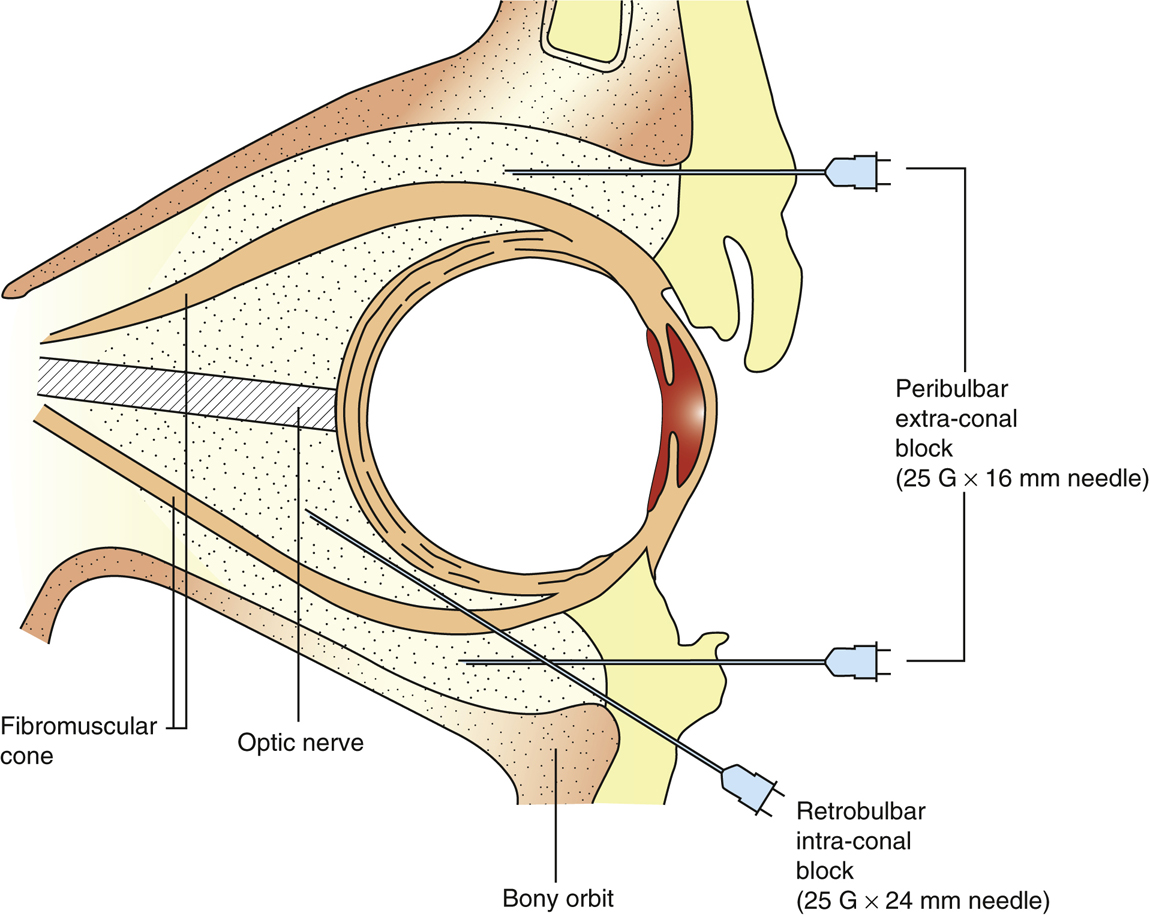
- Technique. Intraocular surgery requires adequate sensory and motor block of the eye and often the eyelids as well. Anesthesia of the eye is accomplished by injecting local anesthetic into the retrobulbar space, peribulbar space, or episcleral space, facilitating neural blockade of CNs II through VI.
- Retrobulbar block is achieved by injecting 4 to 6 mL of a 50:50 mixture of 1% lidocaine and 0.375% bupivacaine (with 5 units hyaluronidase) within the muscle cone formed by the four recti muscles and the two oblique muscles. With the eye in a neutral position, a 23- or 25-gauge blunt Atkinson 1 ¼-inch needle is inserted through the lower lid or conjunctiva at the level of the inferior orbital rim in the inferotemporal quadrant. The needle is first advanced slightly inferiorly and temporally approximately 1.5 cm; once past the equator of the eye, the needle is then directed superiorly and nasally toward the apex of the orbit to a depth of approximately 3.5 cm, while feeling for a “pop” as the needle penetrates through the muscle cone (Figure 30.1).
- Peribulbar block. No attempt is made to enter the muscle cone. A 25-gauge ¾-inch Atkinson needle is advanced along the inferior orbital floor to a depth of approximately 2.5 cm. Between 8 and 10 mL of local anesthetic is required, and hyaluronidase (3.75-15 U/mL) is frequently added to help facilitate spread through the muscle cone. Careful aspiration before injection is required for both blocks, followed by gentle massage or orbital compression to promote the spread of the anesthetic (although orbital compression should be avoided in patients with glaucoma). If desired, the facial nerve can also be blocked by infiltrating 2 to 4 mL of additional local anesthetic along the inferior and superior orbital rim to help prevent squinting. The retrobulbar block provides faster, more reliable anesthesia and akinesia but has a higher complication rate as compared with the peribulbar block (Figure 30.1).
- Episcleral block (sub-Tenon block). Local anesthetic is injected into the episcleral space via a needle or cannula. Needle entry is into the fornix at an angle tangential to the globe, between the conjunctival semilunaris fold and globe. Upon entry into the conjunctiva, the needle is shifted medially and advanced posteriorly until a “click” is felt. Local anesthetic is then injected, with volumes greater than 6 mL producing both globe analgesia and akinesia. Using the cannula technique, topicalization is performed and the bulbar conjunctiva lifted in the inferonasal quadrant with forceps. A small nick is made in the conjunctiva and Tenon capsule using blunt Westcott scissors, accessing the episcleral space. A specially designed blunt cannula is inserted, advanced into the episcleral space, and 3 to 4 mL of local anesthetic injected.
- Complications of regional anesthesia are infrequent but include direct optic nerve trauma, transient globe compression with increased IOP, retrobulbar hemorrhage, globe perforation, and stimulation of the OCR. Hyaluronidase is toxic to the eye if injected into the globe. Intravascular injection of local anesthetic may cause seizures or myocardial depression. Rarely, the local anesthetic may dissect proximally along the neural sheath of the optic nerve and a total spinal can occur; treatment is supportive.
- During the procedure, fresh air at a flow rate of 10 to 15 L/min is provided to the patient under the drapes using a large face mask. This helps to remove exhaled carbon dioxide and helps offset the sense of claustrophobia some patients may experience. Oxygen may be used if indicated, but the surgeon should be notified not to use electrocautery while oxygen is flowing. Capnography is frequently used since visual inspection of respiration may be difficult while patients are draped.
- General anesthesia
- Goals include (1) a smooth induction and maintenance of stable IOP, (2) avoidance and treatment of OCR, (3) maintenance of a motionless field with sufficient depth of anesthesia with or without NMB since the eye is highly innervated, (4) avoidance of postoperative nausea and vomiting (PONV), and (5) a smooth emergence.
- Smooth emergence and extubation are particularly desirable after ophthalmic surgery. This may be facilitated by thorough posterior pharyngeal suctioning while the patient is still deeply anesthetized, administration of an opioid to reduce the cough reflex, and IV lidocaine or dexmedetomidine before planned extubation. Deep extubation is also an option but does not guarantee a smooth emergence.
- Ketamine can cause blepharospasm, nystagmus, and vomiting. It may increase arterial pressure and IOP. For these reasons, ketamine usually is a poor choice for most ophthalmic surgeries.
- Ophthalmic procedures
- Open-eye injury. Penetrating eye trauma may be a surgical emergency or needs to be addressed within 24 hours of injury to minimize the risk of infection. It requires a carefully conducted anesthetic designed to prevent aspiration and favorably affect IOP. A sudden increase in IOP can result in extrusion of ocular contents and cause permanent vision loss. Trauma to the eye and orbit, long-duration and complex surgery, and a crying patient with a full stomach usually mandate general endotracheal anesthesia.
- Succinylcholine causes an increase in IOP of approximately 6 to 12 mm Hg for 10 minutes before returning to baseline. This has not been shown to be clinically significant and succinylcholine often is the drug of choice during a rapid sequence induction (RSI) in the eye surgery patient with a full stomach. Alternatively, 1.2 mg/kg of rocuronium can be used during an RSI.
- An adequate depth of anesthesia and degree of NMB must be ensured before laryngoscopy and intubation to minimize increases in IOP (which may rise to 40-50 mm Hg) secondary to straining, coughing, and bucking.
- In children, if an IV cannot be placed, an inhalation induction along with cricoid pressure may be necessary.
- Strabismus repair is a procedure to alter the lengths of the extraocular muscles.
- Surgical manipulation frequently elicits the oculocardiac reflex (see Section I.A.3).
- PONV is very common (40%-85% incidence in untreated patients). Strategies to reduce the incidence of PONV include minimizing opioids, multimodal analgesia, combination of antiemetics with different mechanisms of action (ondansetron, dexamethasone, haloperidol, etc.), gastric decompression using orogastric tube (OGT), ensuring adequate hydration, and possible total intravenous anesthetic (TIVA).
- Retinal surgery for detachment and vitreous hemorrhage often is performed on patients in extremes of age and/or with multiple comorbidities. Meticulous attention to airway management, fluid status, normothermia, and postoperative transport is crucial. Premature infants, especially those less than 60 weeks postconceptional age, are at risk for postoperative central apnea. They should demonstrate a 12-hour apnea-free interval before discharge. Patients with diabetes or sickle cell anemia also may require retinal surgery (see Chapter 7, Section I.G and Chapter 37, Section X.C).
- Regional anesthesia is suitable for short procedures (<3 hours) in cooperative patients, although unexpected movement during the delicate retinal repair may result in vision loss.
- An intravitreal gas bubble containing an inert, high-molecular-weight, low-diffusivity gas such as sodium hexafluoride (SF6), perfluoropropane (C3F8), octofluorocyclobutane (C4F8), or air, may be injected at the conclusion of surgery to reduce intravitreal bleeding. Nitrous oxide should be avoided in surgeries where an intravitreal gas bubble is injected as it will rapidly expand the bubble and increase IOP. Because these gas bubbles remain for various periods of time, administration of nitrous oxide should be avoided for 5 days after an air injection, 10 days after SF6 injection, and 60 days after C3F8 injection. Owing to pressure changes associated with air travel, patients should be instructed to avoid air travel for 3 to 4 weeks after intravitreal gas injection.
- Open-eye injury. Penetrating eye trauma may be a surgical emergency or needs to be addressed within 24 hours of injury to minimize the risk of infection. It requires a carefully conducted anesthetic designed to prevent aspiration and favorably affect IOP. A sudden increase in IOP can result in extrusion of ocular contents and cause permanent vision loss. Trauma to the eye and orbit, long-duration and complex surgery, and a crying patient with a full stomach usually mandate general endotracheal anesthesia.