The most important clues to a clinically significant bleeding disorder in an otherwise healthy patient may be obtained from a thorough history. In particular, a personal or family history of anemia requiring iron replacement or blood products may suggest a bleeding diathesis. Prior excessive surgical bleeding, gingival bleeding, easy bruising, epistaxis, or menorrhagia should raise concern. Many laboratory tests are available to assess the coagulation system. However, the clinician must remember that coagulation depends on a complex interplay of platelets and coagulation factors that may not be fully captured by any single test.
- Activated partial thromboplastin time (aPTT or PTT) is measured by adding particulate matter such as silica or kaolin to a blood sample to activate the coagulation system. Normal values for the PTT are 22 to 34 seconds but vary according to the reagent and instruments used by the specific laboratory. The PTT assesses factors in the intrinsic (XI, XII, VIII, IX, and contact factors) and the common (II, V, X, and fibrinogen) coagulation pathways. The test is sensitive to decreased amounts of coagulation factors, and the value is elevated in patients on heparin therapy. The PTT will also be abnormally elevated in patients with hemophilia or a circulating anticoagulant (eg, lupus anticoagulant or antibodies to factor VIII). The clinician should remember that an abnormal PTT does not necessarily correlate with clinical bleeding severity. Therefore, aggressive correction of an abnormal PTT in surgical patients is not universally indicated unless the patient is actively bleeding.
- PT is measured by adding tissue factor (thromboplastin) to a blood sample to activate coagulation. It serves as a measure of factors of the extrinsic (VII and tissue factor) and common (see above) coagulation pathways. Although both PT and PTT are affected by levels of factors V and X, prothrombin, and fibrinogen, the PT is specifically sensitive to deficiencies of factor VII. The PT is also normal in deficiencies of intrinsic pathway factors VIII, IX, XI, XII, prekallikrein, and high-molecular-weight kininogen. Normal values fall between 10 and 15 seconds, although the international normalized ratio (INR) (see below) is more commonly reported given the variability of PT results between laboratories.
- The INR represents a means of standardizing PT values to allow reliable comparison among different laboratories. It is defined as the ratio of the patient’s PT to the control PT value that would be obtained if international reference reagents had been used to perform the test. Oral warfarin anticoagulation therapy may therefore be guided by a target INR value that is independent of the laboratory variability of the PT. For example, an INR of 2.0 to 3.0 is recommended for prophylaxis against thromboembolism in atrial fibrillation. Higher INR values may be targeted in specific populations at increased risk for thromboembolic phenomena (eg, patients with mechanical mitral valves).
- Activated clotting time (ACT) is a modified whole blood clotting time in which diatomaceous earth (celite) or clay (kaolin) is added to a blood sample to activate the intrinsic pathway. The ACT is the time until clot formation. A normal ACT is 90 to 130 seconds depending on the instrument used. Compared with the PTT, the ACT is a relatively easy and expedient test to perform and is useful in monitoring heparin therapy rapidly in the operating room (see Chapter 24). However, because the ACT is relatively insensitive to lower levels of heparin anticoagulation, it is typically reserved for settings that require higher doses of heparin, particularly cardiopulmonary bypass and extracorporeal membrane oxygenation.
- Platelet counts can be measured to determine the risk of excessive bleeding due to platelet depletion. Commonly accepted normal values range between 150,000 and 450,000/mm3, and a clinical threshold for perioperative platelet transfusion is often less than 50,000/mm3. However, platelet counts do not provide a qualitative metric of platelet function and thus may not reliably reflect the risk of bleeding in certain populations.
- Platelet function tests range from simple assessments of bleeding time to sophisticated optical aggregometry techniques. In circumstances involving elements of platelet dysfunction, including uremia and the use of antiplatelet agents, point-of-care tests of platelet activation and aggregation—such as that generated by the platelet function analyzer 100 (PFA-100) device—may provide insight into bleeding risk. However, these tests remain largely unvalidated for routine perioperative use. Thromboelastography may also allow for rapid assessment of platelet function.
- Fibrinogen is the precursor protein that is activated to form fibrin and then cross-linked to strengthen clots. Assaying fibrinogen levels can be helpful when coagulopathy is present or suspected. Although the diagnostic specificity of the fibrinogen level is low, it can be helpful to guide further transfusion support (ie, the administration of fresh frozen plasma [FFP] or cryoprecipitate).
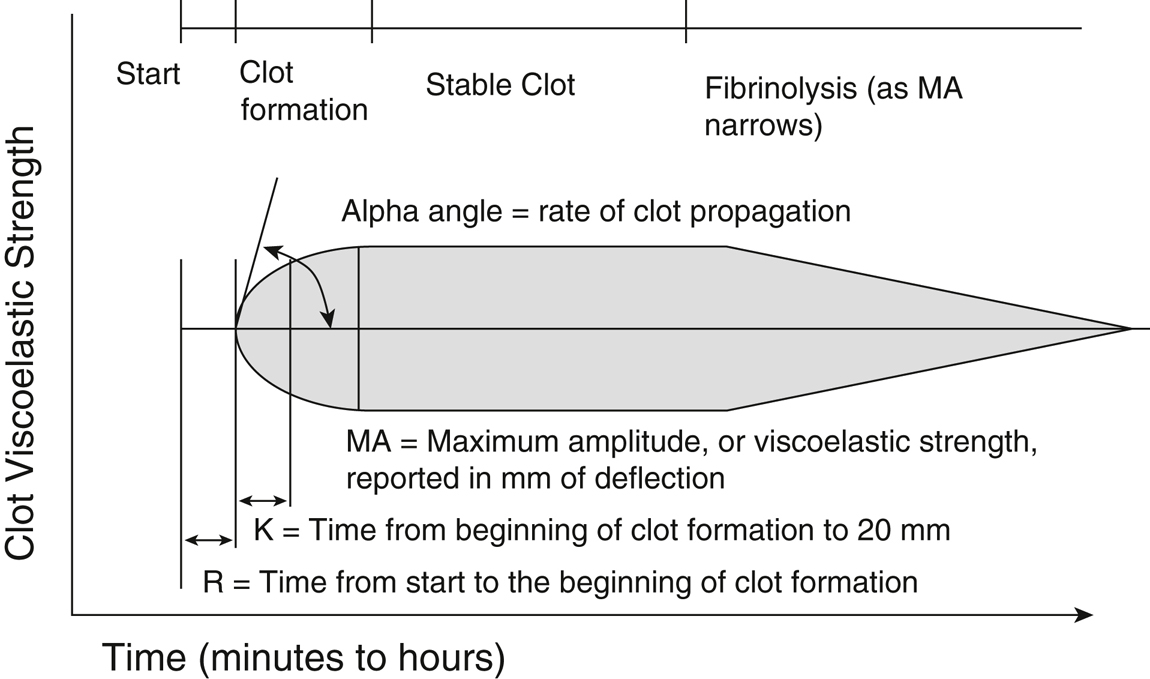
- Thromboelastography (TEG) is available in some centers for clinical use, often as a point-of-care test. TEG is performed by placing a small aliquot of blood into a heated oscillating cup, into which a pin on a torsion wire is suspended. Clot formation in the oscillating cup generates torque on the pin, and the torque is measured and converted to an electrical signal. The signal is then recorded by a computer, creating a characteristic trace (Figure 36.1) that may be analyzed for abnormalities of clot formation. By measuring clot formation and viscoelastic clot strength, TEG provides information about the adequacy of clotting factors, fibrin levels, and platelets. In general, R time represents the activity of coagulation factors, the alpha angle and K time represent acceleration of fibrin formation, maximum amplitude represents platelet function, and percent lysis in 30 minutes (LY30) represents the rate of fibrinolysis. Thromboelastometry (TEM, previously ROTEM) uses similar technology with similarly measured parameters.