- Difficult airway. The 2013 revision of the American Society of Anesthesiologists (ASA) algorithm for managing difficult airways is shown in Figure 13.9. Familiarity with this algorithm is crucial for the anesthesiologist. Since its adoption in 1993, the number of death and brain death claims associated with airway-related events during induction of anesthesia has decreased significantly.
- The difficult airway can be divided into the recognized difficult airway and the unrecognized difficult airway; the latter presents the greater challenge for the anesthesiologist.
Figure 13-9 American Society of Anesthesiologists (ASA) difficult airway algorithm.

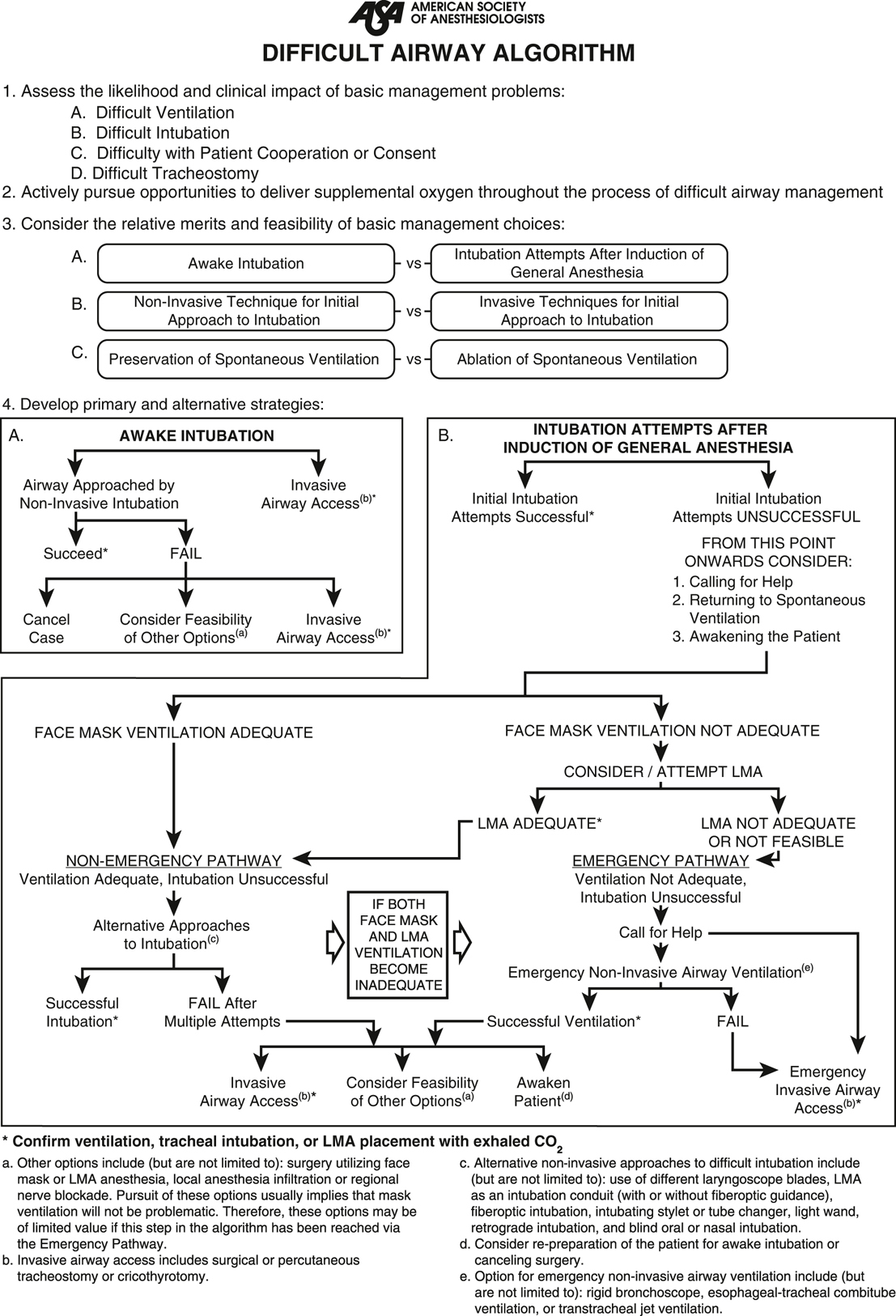
(Reprinted with permission from American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98(5):1269-1277. Copyright © 2003 American Society of Anesthesiologists, Inc.)
- The ASA defines a difficult airway as the situation in which an anesthesiologist experiences difficulty with mask ventilation, difficulty with tracheal intubation, or both. Another definition of a difficult airway is failure to intubate with conventional laryngoscopy after an optimal/best attempt. This optimal/best attempt is defined as an attempt with an experienced laryngoscopist, no significant resistive muscle tone, use of optimal sniffing position, use of external laryngeal manipulation, change of laryngoscope blade type a single time, and change of laryngoscope blade length a single time.
- The use of regional anesthesia as a way to avoid the known or anticipated difficult airway deserves special mention. Although the difficult airway algorithm suggests considering regional anesthesia, it must be kept in mind that the regional block can fail or the patient may require rapid conversion to a general anesthetic for other reasons. Regional anesthesia generally should not be elected for a patient with a known difficult airway if the surgery cannot be terminated rapidly (in case of failed or inadequate block) or access to the patient’s airway is compromised.
- Supraglottic airway devices (eg, LMA) are used to keep the upper airway open to allow oxygenation and ventilation and are a prominent airway option throughout the 2013 ASA difficult airway algorithm:
- Nonemergency
- An airway in patients who can be mask ventilated after general anesthesia is induced but cannot be intubated. It is also an alternative if awake intubation has failed (but only when general anesthesia and mask ventilation are not considered problematic).
- A conduit for intubation in patients who can be mask ventilated but cannot be intubated with conventional laryngoscopy.
- Emergency
- Nonemergency
- The difficult airway can be divided into the recognized difficult airway and the unrecognized difficult airway; the latter presents the greater challenge for the anesthesiologist.
- Emergency airway techniques
- Percutaneous needle cricothyroidotomy involves placing a 14-gauge IV catheter or 7.5-French introducer through the cricothyroid membrane into the trachea. Oxygen can be administered by connecting the breathing circuit to a 3-mm ID ETT adapter inserted directly into the IV catheter or to a 7.0-mm ID ETT adapter inserted into a 3-mL syringe barrel and connected to the IV catheter. Dedicated cricothyroidotomy catheters are preferred as the IV catheters have a very high rate of kinking and obstruction. Percutaneous needle cricothyroidotomy is a temporary maneuver until more stable airway access is achieved (tracheostomy or intubation). It is absolutely contraindicated in cases of complete upper airway obstruction because severe barotrauma may result.
- Oxygenation, but not ventilation, can be achieved by administering oxygen through the catheter at flow rates of 10 to 12 L/min.
- Some ventilation may be achieved by pressing the oxygen flush valve for 1 second and allowing for passive exhalation over 2 to 3 seconds.
- Once in place, the catheter must be carefully and firmly held in position to avoid dislodgment, which can be life threatening.
- Complications include barotrauma, pneumothorax, subcutaneous emphysema of the neck and anterior chest, loss of the airway, aspiration, and death.
- Rigid bronchoscopy by a surgeon or interventional pulmonologist may be necessary to support an airway partially obstructed by a foreign body, traumatic disruption, stenosis, or mediastinal mass. General anesthesia is usually required. A range of bronchoscope sizes (including pediatric sizes) should be available (see Chapter 27).
- Cricothyroidotomy is a rapid effective method for relieving severe upper airway obstruction. The cricothyroid membrane is an elastic tissue located between the inferior border of the thyroid cartilage and the superior border of the cricoid cartilage. With the neck extended, a small incision is made in this membrane in the midline. The handle of a scalpel or a Kelley forceps is used to separate the tissues, and a tube (eg, tracheostomy tube or ETT) is inserted. Alternatively, commercial kits are available, which allow cricothyroidotomy to be performed using Seldinger technique. An introducer needle is used to perforate the cricothyroid membrane and a guidewire is advanced through the needle. Next, a combined tissue dilator-airway catheter is advanced over the wire, the dilator is removed, and the airway catheter is left in the trachea.
- Tracheostomy may be performed under local anesthesia before the induction of general anesthesia for a patient with a particularly difficult airway.
- Technique. After careful dissection of vessels, nerves, and the thyroid isthmus, a tracheal incision is made, usually between the third and fourth cartilaginous rings. Percutaneous dilational tracheostomy, using commercially available techniques and a modified Seldinger technique, may also be performed.
- Complications include hemorrhage, false passage, and pneumothorax.
- Percutaneous needle cricothyroidotomy involves placing a 14-gauge IV catheter or 7.5-French introducer through the cricothyroid membrane into the trachea. Oxygen can be administered by connecting the breathing circuit to a 3-mm ID ETT adapter inserted directly into the IV catheter or to a 7.0-mm ID ETT adapter inserted into a 3-mL syringe barrel and connected to the IV catheter. Dedicated cricothyroidotomy catheters are preferred as the IV catheters have a very high rate of kinking and obstruction. Percutaneous needle cricothyroidotomy is a temporary maneuver until more stable airway access is achieved (tracheostomy or intubation). It is absolutely contraindicated in cases of complete upper airway obstruction because severe barotrauma may result.