- BLS refers to the core competency live-saving skill set of CPR, activation of the emergency response system, and expedient use of an automated external defibrillator (AED). BLS certification is offered to the public and is required for healthcare providers with variations in management suggestions based on level of training and comfort.
Any person found unresponsive or with absent or gasping/agonal breath sounds should be suspected to be in cardiac arrest (IIa/C-LD). Pulse checks by a healthcare provider in this setting should last at most 10 seconds (II/C). If the person cannot be aroused, the AHA guidelines for CPR and emergency cardiac care stress immediate activation of the emergency response system for out-of-hospital arrests and initiation of chest compressions to provide Circulation prior to Airway management and Breathing, or C-A-B. This was changed from A-B-C in 2010 to emphasize the initial focus on restoring circulation based on survival studies.
The C-A-B sequence emphasizes circulation first to minimize delays in chest compressions associated with establishing a patent airway. Beginning with chest compressions may also increase likelihood that bystanders will perform CPR on persons who have suffered from SCA as lay persons may find airway management challenging and hesitate to initiate CPR. In fact, the guidelines changed in 2017 to emphasize that untrained lay rescuers may provide compression only CPR (I/C-LD), and dispatchers should offer compression-only CPR instructions (I/C-LD). Lay persons trained in CPR should still add rescue breaths when trained or able.
For lone rescuers, the public is taught the “phone first/phone fast” rule. For adults, children aged 8 years and older, and all children known to be at high risk for arrhythmias, the emergency medical system (911; EMS) should be activated (phone first) before attempts at resuscitation by a lone rescuer. An initial resuscitation attempt followed by the activation of EMS (“phone fast”) is indicated for children less than 8 years old and for all ages in cases of submersion or near drowning, arrest secondary to trauma, and drug overdose. Owing to the increased rate of unresponsiveness secondary to opioid overdose, family members are recommended to have naloxone available to administer in coordination with alerting EMS.
- Circulation (chest compressions). It is estimated that chest compressions can provide up to one-third of the normal cardiac output. To ensure sufficient circulation, especially coronary and cerebral flow, compressions should occupy a minimum 60% of the arrest event time (IIb/C-LD) with a target of 80% and minimal pauses between shocks (I/C-LD). The patient should be on a firm surface, preferably a backboard when possible, and flat with their head at the level of the thorax. This is especially true in an OR where the soft surgical table padding/gel absorbs energy from compressions, which can decrease their effectiveness. For a prone, intubated patient in the OR who cannot be quickly turned supine for CPR, one member can place a clenched fist between the subxiphoid area and the OR table with compressions over the corresponding region of the back (IIb/C).
Proper positioning involves placing the heel of your hand in the center of the patient’s chest at the intermammary line with the heel of the other hand on top of the first so that the hands are overlapped and parallel (IIa/B). Shoulders can be positioned directly over the patient and elbows locked. The chest should depress to a minimum 2 inches in adults (I/C-LD) and at least one-third of the anterior-posterior chest diameter for pediatric patients (roughly 2 inches in children, 1.5 inches in infants) (IIa/C-LD). For children, single responders can use the heel of one or both hands (IIb/C). In infants, single responders should use a two-finger technique, whereas the two-thumb encircling hands technique is used with multiple responders (IIb/C).
The chest compression rate should be at least 100/min, and allow for complete chest recoil by targeting equal compression and relaxation times (IIb/C). While rate and depth tend to err on the lower side, compressions quality can also suffer from being too deep or too fast, thus upper bounds of 2.4 inches for depth and 120 for rate were introduced. Given this notably small range of 2 to 2.4 inches (5-6 cm), compression feedback devices that optimize performance should be used when available (IIb/B-R).
The target compression-ventilation ratio is 30:2 for single responders with two breaths being delivered over less than 10 seconds (IIa/C-LD). With two or more people, the 30:2 ratio is preserved, and providers should switch every 2 minutes (five cycles) in less than 5 seconds (IIa/B). In children, the compression-ventilation ratio is 15:2 when there are two rescuers to reflect the more respiratory driven arrest incidence. If an advanced airway such as an endotracheal tube (ETT) or laryngeal mask airway (LMA) is in place during two-rescuer CPR, ventilations should be given at a rate of 10 breaths/min simultaneously with compressions without pauses.
Another described maneuver is the precordial “thump” whereby the rescuer slams the underside of their fist to the mid-sternum to depolarize the heart. This maneuver can be considered for monitored patients with unstable or pulseless VT if a defibrillator is not immediately available (IIb/C), although this method of triggering depolarization with swift mechanical impulses should not be used to “pace” the heart.
- Airway and breathing. Although recent guideline changes have focused on circulation (all the way to compression-only CPR), maintaining a patent airway with adequate ventilation and oxygenation remains critical (I/C). It becomes more vital as arrest time increases owing to exhaustion of alveolar oxygen reserve and accumulation of carbon dioxide. Spontaneous ventilation is evaluated by observation and auscultation and aided by repositioning, most commonly through a head tilt-chin lift technique (IIa/B). If a cervical spine injury is suspected based on the scene or nature of injury, a jaw thrust without head extension should be attempted (IIb/C), although if unsuccessful at establishing airway patency, a head tilt should still be used (I/C). If ventilation remains impossible after these maneuvers and an advanced airway is not available, efforts to clear the airway of a suspected foreign body should be attempted. In primary foreign body obstruction, abdominal thrusts (Heimlich maneuver) should be attempted (IIb/B) and chest thrusts considered when unsuccessful (IIb/B). This differs for infants for whom back blows are delivered in succession with chest compressions for foreign body obstruction.
When an adult has spontaneous circulation by palpable pulses but ineffective breathing alone, rescue breaths should be provided 10 to 12 times per minute or every 5 to 6 seconds (IIb/C). Breaths should be delivered over 1 second with enough volume for visible chest rise, roughly 500 to 600 mL in adults (IIa/C). Rescue breaths during cardiac arrest should be similarly provided over 1 second with visible chest rise. In the absence of an advanced airway, compressions are briefly paused for breaths at the 30:2 ratio whether there are one or more providers. With an advanced airway in place, breaths should be given every 6 seconds (10/min) concurrent with compressions as mentioned above.
Hyperventilation (III/B) in any setting from excess respiratory rate or tidal volume should be avoided as it can cause gastric insufflation provoking aspiration and, more importantly, it can increase intrathoracic pressure, impair venous return, and lower cardiac output, which ultimately worsens outcomes.
- Defibrillation in BLS refers to the use of AEDs, which should be retrieved as part of the initial activation of the emergency response system. Timely defibrillation and CPR are major determinants of a successful resuscitation. Defibrillation is the definitive management for pulseless VT and VF (I/A). When an arrest is witnessed and an AED is within reach, the defibrillator should be used as soon as possible (IIa/C-LD). For unwitnessed arrests, CPR should be initiated while the AED is being retrieved (IIa/B-R).
Public access defibrillation programs have enabled public safety professionals (eg, fire personnel, police, security guards, and airline attendants) to employ readily accessible AEDs. The devices themselves are small and lightweight and use adhesive electrode pads for both sensing and delivering shocks. Visual and voice prompts are provided to assist the operators with the goal of making it usable by an untrained bystander. After analysis of the frequency, amplitude, and slope of the ECG signal, the AED advises either “shock indicated” or “no shock indicated.” The AED is manually triggered and does not automatically defibrillate the patient as an automatic shock could injure someone touching the patient. AEDs are now also equipped with pediatric pad-cable systems that attenuate the adult dose to a smaller dose appropriate for children. The dose attenuators should be used in children less than 8 years of age and less than 25 kg in weight. For infants, manual defibrillation is recommended, but if unavailable, an AED with or without an attenuator can be used. There are efforts to make AED analysis more sophisticated such as incorporating artifact filtering so that compressions can be continued during rhythm analysis. At this point, these technologies are not reliable enough to promote (IIb/C-EO).
- Reassessment. Although it is tempting to see if the defibrillation worked by checking for a pulse immediately after a shock, the heart still needs time to establish sufficient forward flow and compressions should be resumed immediately after shock delivery (IIb/C-LD) with a rhythm check after five cycles of CPR (2 minutes). For healthcare providers, if there is evidence of a perfusing rhythm, the pulse can be checked to determine if there is ROSC. If a nonshockable rhythm or no pulse is detected, CPR should be resumed with rhythm checks after every five cycles as before.
- Circulation (chest compressions). It is estimated that chest compressions can provide up to one-third of the normal cardiac output. To ensure sufficient circulation, especially coronary and cerebral flow, compressions should occupy a minimum 60% of the arrest event time (IIb/C-LD) with a target of 80% and minimal pauses between shocks (I/C-LD). The patient should be on a firm surface, preferably a backboard when possible, and flat with their head at the level of the thorax. This is especially true in an OR where the soft surgical table padding/gel absorbs energy from compressions, which can decrease their effectiveness. For a prone, intubated patient in the OR who cannot be quickly turned supine for CPR, one member can place a clenched fist between the subxiphoid area and the OR table with compressions over the corresponding region of the back (IIb/C).
- ACLS describes the definitive, medically exhaustive treatment for cardiac arrest taught exclusively to health professionals. It builds upon BLS skills and can be provided in the field by paramedics or in a hospital setting. As OR and intensive care unit (ICU) providers, anesthesiologists should keep themselves up to date with their certification and with changes to management protocols, which are amended yearly. Interventions described in ACLS include advanced airway management, manual defibrillation, synchronized cardioversion, pharmacologic management, and decisions toward more invasive mechanical circulatory support or withdrawal of care.
- Advanced airway. Swift control of the airway optimizes oxygenation and the removal of carbon dioxide during resuscitation. Options are bag-mask ventilation or an advanced airway such as an ETT or LMA (IIb/B-R). The goal is to secure the airway via endotracheal intubation, which should be performed by the most experienced provider, often a trained anesthesiologist. Insertion of an oropharyngeal or nasopharyngeal airway can improve ventilation in an obstructed airway before intubation (IIa/C). Although cricoid pressure is sometimes used during bag-mask ventilation to decrease gastric insufflation, routine use is discouraged (III/B) as it tends to be performed incorrectly or in a manner that impairs ventilation.
Endotracheal intubation during an in-hospital arrest can be difficult given confined space, poor patient positioning, suboptimal visualization, and interference from chest compressions. Waveform capnography, which is often a component of modern defibrillators, is the most reliable method to confirm correct placement (I/C-LD), although a color-changing in-line CO2 detector is frequently the most readily available. The ETT may be used to deliver certain lipophilic drugs like naloxone, atropine, vasopressin, epinephrine, or lidocaine (NAVEL, now known as LEAN with removal of vasopressin) if intravenous (IV) access has not been established. Higher doses of these drugs are needed (2-3 times as much) owing to lower peak blood concentrations and should be diluted in 10 mL of sterile saline.
- Defibrillation. Pulseless VT and VF are shockable dysrhythmias associated with cardiac arrest (see Figure 39.1). As the duration of SCA increases, cardiac ischemia worsens, and it becomes more difficult to achieve ROSC. Rapid defibrillation is critical in this situation before the rhythm degenerates into PEA or asystole. It is the responsibility of the person operating the defibrillator to ensure that members of the resuscitation team are not in contact with the patient during defibrillation.
Figure 39-1 Algorithm for pulseless arrest.

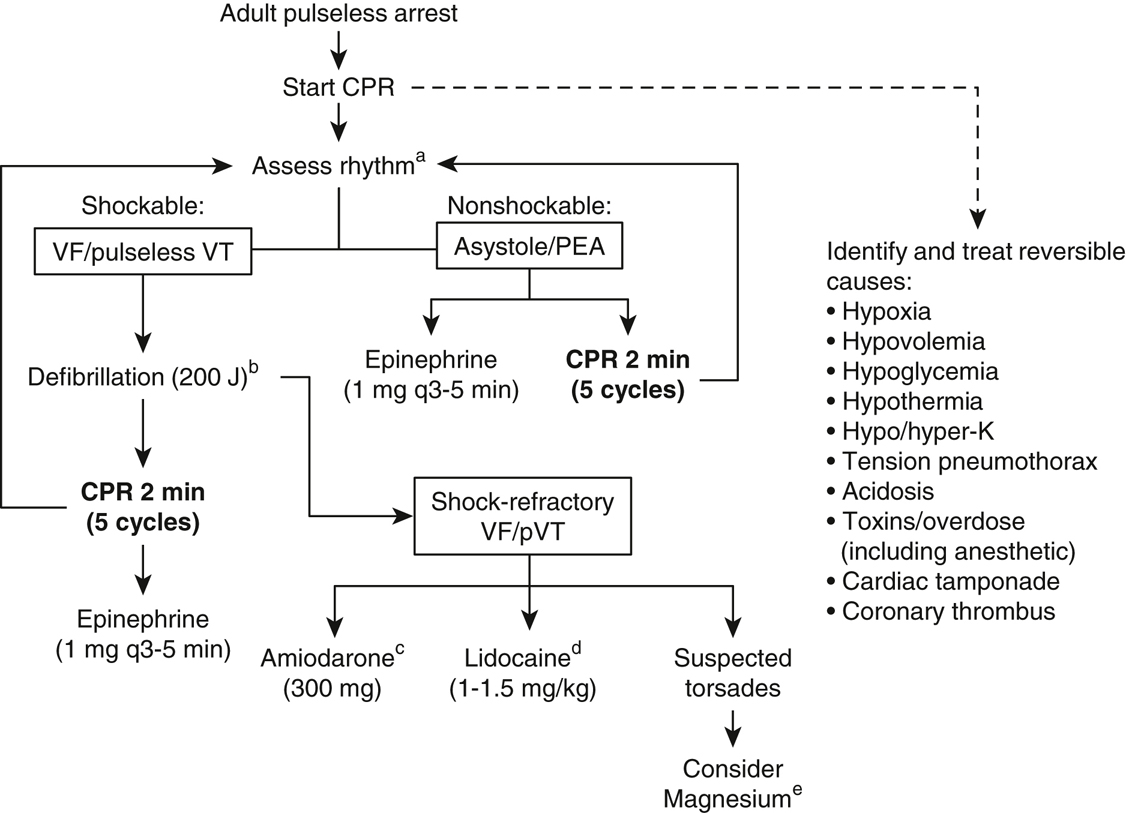
VF, ventricular fibrillation; VT, ventricular tachycardia. aWhen rhythm is unclear and could be VF, treat as shockable rhythm. bBiphasic. One cycle of CPR should follow any successful defibrillation. cAmiodarone bolus should be administered in 20 to 30 mL saline or D5W. This is followed by an infusion of 1 mg/min for 6 hours and then 0.5 mg/min thereafter. An additional dose of 150 mg IV can be readministered for recurrence of VF or VT. dLidocaine can be bolused again at a dose of 0.5 to 0.75 mg/kg. eMagnesium sulfate 1 to 2 g can be considered for torsades (long-QT-associated polymorphic VT) but trials have not demonstrated an advantage. Vasopressin is no longer used in the ACLS protocol as its use had no added benefit relative to or in combination with epinephrine.
Defibrillators deliver energy in a biphasic pulse that alternates current flow. The optimal dose to terminate VF is 150 to 200 J and is indicated on the front of the defibrillator. In children, an initial dose of 2 to 4 J/kg is advised (IIa/C-LD). The pediatric dose can be increased with successive shocks but should not exceed 10 J/kg or the maximum adult dose (IIb/C-LD). The large adult pads/paddles (8-13 cm) are recommended in children above 1 year of age and at least 10 kg in weight. Infant pads/paddles (4.5 cm) are used in children less than 10 kg in weight. Pads are preferred to paddles, as they can aid in rhythm detection and pacing. The defibrillator should be charged while compressions continue, and once ready to discharge, the provider calls “clear” to alert everyone to remove their hands from the patient and the shock is delivered, and compressions are resumed.
Cardioversion using synchronized biphasic shocks are used for unstable tachyarrhythmias with pulses (rates generally >150 bpm) such as paroxysmal supraventricular tachycardia (PSVT), atrial fibrillation, re-entrant arrhythmias, or unstable VT. The recommended initial energy dose for synchronized cardioversion of atrial fibrillation is 120 to 200 J (IIa/A). Dosing can be increased in a stepwise fashion if the initial shock is ineffective. Hemodynamically stable VT can be cardioverted using 100 J as the starting point (IIb/C). The initial dose for cardioversion in children is 0.5 to 1 J/kg followed by subsequent doses of 2 J/kg. See Figure 39.3 for management of tachyarrhythmias in adults.
- Pacing. High-grade heart block with profound bradycardia is one etiology of cardiac arrest. Temporary pacing should be used when the bradyarrhythmia does not improve with medication (primarily atropine) and there are signs of instability (eg, altered mental status, severe hypotension) (IIa/B). Transcutaneous pacing is the easiest method to increase the ventricular rate but may require high currents for consistent capture, which can be very uncomfortable for awake patients. Transesophageal atrial pacing is efficacious for sinus bradycardia with maintained atrioventricular (AV) conduction and is useful intraoperatively for bradycardia-related hypotension in otherwise stable patients. Transvenous pacing via a temporary wire into the right heart is a third option to increase heart rate while CPR continues. Special pacing pulmonary artery catheters are capable of AV pacing. See Figure 39.2 for management of symptomatic bradycardia.
Figure 39-2 Algorithm for bradycardia.

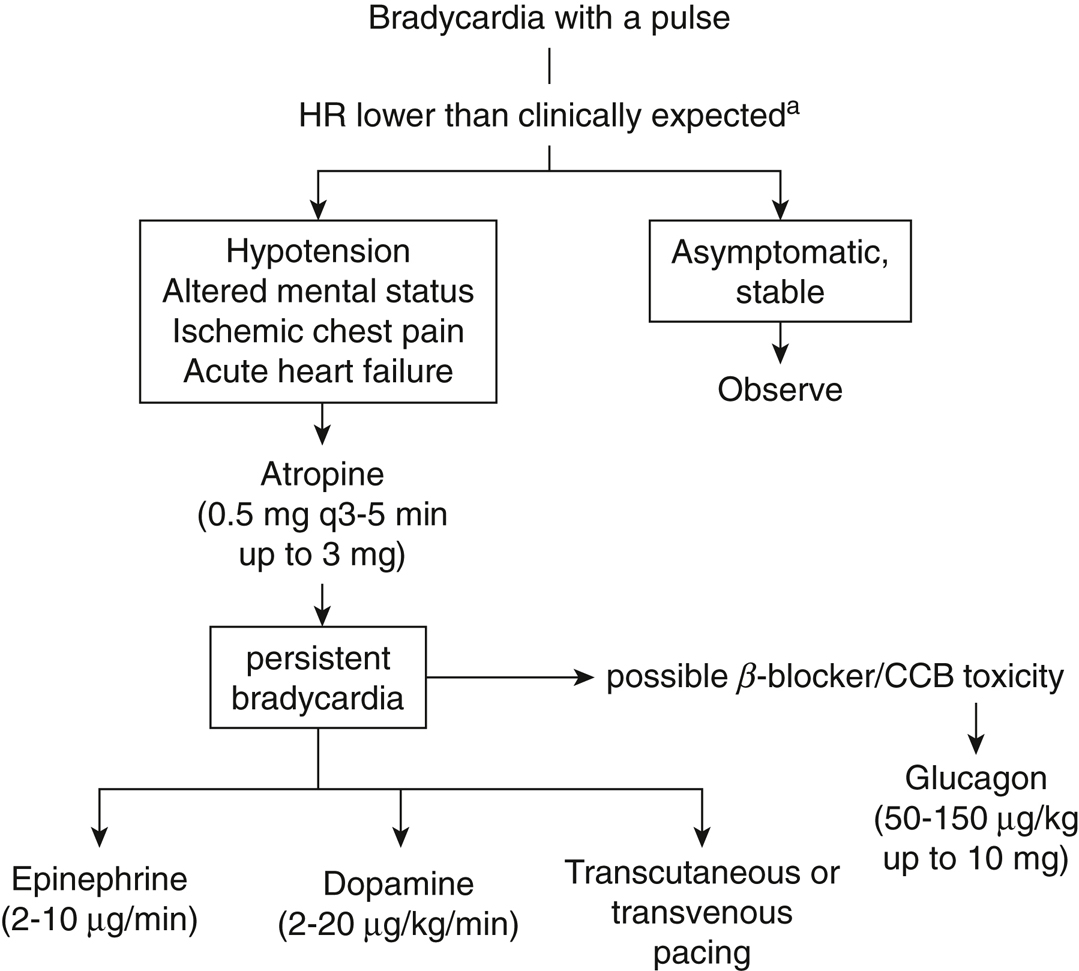
HR, heart rate; bpm, beats per minute; CCB, calcium channel blocker. aNormal heart rate goal may be <60 bpm for patients receiving therapeutic nodal agents (eg, β-blocker). When IV access or medications are not immediately available, can jump to transcutaneous pacing.
- Vascular access is imperative for successful resuscitation, but establishment of venous access should not delay chest compressions or defibrillation when appropriate. The most desirable route is into central circulation, which should be prioritized when possible (IIb/C). The insertion site (internal jugular, external jugular, subclavian, or femoral vein) is predicated on the anatomy of the patient, experience of the physician, and what is least disruptive to resuscitation. Peripheral IV catheters in antecubital veins are adequate when an appropriate volume is used to flush medications toward the central circulation (~20-mL bolus). If peripheral vascular access is not easily established, intraosseous (IO) cannulation should be attempted (IIa/C). IO access can be done in less than a minute in children. All drugs and fluids can be given through an IO route until good IV access is found.
Another form of vascular access to strongly consider is an arterial line, which is beneficial for sending arterial blood gases to aid in management and for evaluating compression quality (via pulsatile flow visualization) and return of spontaneous circulation.
- Drugs. The drugs described below are used in ACLS protocols for the treatment of hemodynamic instability, myocardial ischemia/infarction, and arrhythmias. The doses of drugs used for PALS are in parentheses following the adult doses. Drugs should be provided centrally whenever possible given the slow circulation times during CPR but can be given peripherally (IV or IO) or via ETT (LEAN medications as described previously).
- Adenosine is an endogenous purine nucleoside with a half-life of 5 seconds. Adenosine slows or blocks anterograde AV node conduction and interrupts AV node reentry pathways to convert a stable PSVT to sinus rhythm. It can also slow the heart rate enough to identify an underlying rhythm that may be difficult to differentiate at elevated heart rates such as atrial fibrillation or atrial flutter. Adenosine can also be considered in the treatment of stable, regular, wide complex monomorphic VT. The initial dose is always a 6-mg rapid IV bolus immediately followed by a 20-mL saline flush (I/B). A brief asystole ensues, followed by P waves, flutter waves, or fibrillation waves that are initially without ventricular responses. The PSVT is sometimes converted to sinus rhythm by the initial dose, but a second injection of 12 mg may be required to terminate the PSVT if there is no effect of the first dose after 1 to 2 minutes. These doses are based on peripheral IV administration. If given via central access, the first and second doses are 3 and 6 mg, respectively.
Recurrent PSVT, AF, and atrial flutter will require longer-acting nodal agents for definitive treatment. The required dose of adenosine may need to be increased in the presence of methylxanthines like theophylline owing to competitive inhibition and decreased if dipyridamole has been administered owing to potentiation via blockage of nucleoside transport (although such adjustments are usually made for infusions during stress tests to induce vasodilation and not in ACLS protocols) (PALS: 0.1 mg/kg; repeat dose 0.2 mg/kg; maximum dose 12 mg). Adenosine should not be used for irregularly irregular rhythms or pre-excitation syndromes like Wolff-Parkinson-White (WPW) as exclusive accessory tract conduction can precipitate VF (III/C).
- Amiodarone is the most versatile drug in ACLS algorithms. It has the properties of all four classes of antiarrhythmics: lengthening of the action potential, sodium channel blockade at high frequencies of stimulation, noncompetitive antisynaptic actions, and negative chronotropism. Because of its high efficacy and low incidence of proarrhythmic effects, it is the preferred antiarrhythmic for patients with severely impaired cardiac function. For shock-refractory pulseless VT/VF, 300 mg diluted in 20 to 30 mL of saline or 5% dextrose in water (D5W) is administered as a bolus. To treat stable dysrhythmias (eg, hemodynamically stable AF, VT), 150 mg is administered over 10 minutes, followed by an infusion of 1 mg/min for 6 hours, and then 0.5 mg/min. The maximum daily dose is 2 g. Immediate side effects can be bradycardia and hypotension (PALS: loading dose 5 mg/kg; maximum dose 15 mg/kg/d). Amiodarone is indicated in the following situations:
- Atropine is an anticholinergic used as the first-line agent for hemodynamically significant bradycardia (IIa/B) or AV block occurring at the nodal level. It increases the rate of sinus node discharge and enhances AV node conduction by its vagolytic activity. It is not effective for Mobitz type II heart block, for complete heart block, or in transplanted hearts missing vagal innervation. It is also not indicated for asystole or PEA (IIb/B) but should be considered for treatment of profound bradycardia that may appear as asystole but with a preserved pulse. The dose of atropine for bradycardia or AV block is 0.5 mg repeated every 3 to 5 minutes to a total dose of 3 mg (PALS: 0.02 mg/kg; minimum dose, 0.1 mg; maximum single dose, 0.5 mg in child, maximum total dose for adolescent 3 mg).
- β-Adrenergic antagonists (eg, atenolol, metoprolol, esmolol, propranolol) have established utility for patients with unstable angina or myocardial infarction. Their competitive inhibition of adrenergic receptors reduces heart rate, AV node conduction, blood pressure, and the effects of catecholamines. This action serves to reduce the rate of recurrent ischemia, nonfatal reinfarction, and postinfarction VF. In contrast to calcium channel blockers, β-blockers are not direct negative inotropes.
β-blockers are useful for the acute treatment of stable PSVT, AF, atrial flutter (I), and ectopic atrial tachycardia (IIb). Initial and subsequent IV doses, if tolerated, are atenolol, 5 mg over 5 minutes, repeated once at 10 minutes; metoprolol, three doses of 5 mg every 5 minutes; propranolol, 0.1 mg/kg divided into three doses given every 2 to 3 minutes; esmolol, 0.5 mg/kg over 1 minute followed by an infusion starting at 50 µg/min and titrated as needed up to 200 µg/min. Contraindications include second- or third-degree heart block, hypotension, and severe congestive heart failure. When a β-blocker might trigger bronchospasm in a patient with chronic lung disease, metoprolol with selective β1 blockade at therapeutic doses may be preferred.
- Calcium is indicated during cardiac arrest only when hyperkalemia, hypermagnesemia, hypocalcemia, or toxicity from calcium channel blockers is suspected. Calcium chloride can be given as a dose of 8 to 16 mg/kg IV (usually 0.5-1g) and repeated as necessary (PALS: calcium chloride 10%: 20 mg/kg = 0.2 mL/kg). Although calcium plays a role in myocardial contraction, studies have not shown any benefit with routine use in cardiac arrest (III/B).
- Calcium channel blockers (nondihydropyridine) such as verapamil and diltiazem depress AV nodal conduction and increase refractory time. These are used to treat hemodynamically stable, narrow complex PSVT unresponsive to vagal maneuvers or adenosine (IIa/B). The initial verapamil dose is 2.5 to 5.0 mg IV, with subsequent doses of 5 to 10 mg IV administered every 15 to 30 minutes. Diltiazem is given as an initial bolus of 15 to 20 mg over 2 minutes. An additional dose of 20 to 25 mg and an infusion of 5 to 15 mg/h can be administered if needed. Their vasodilator and negative inotrope properties can cause hypotension, exacerbation of congestive heart failure, bradycardia, and enhancement of accessory conduction in patients with WPW syndrome. The hypotension can often be reversed with calcium chloride, 0.5 to 1.0 g IV. They are contraindicated for wide complex tachyarrhythmias (III/B).
- Dopamine has dopaminergic (1-5 µg/kg/min), β-adrenergic (5-10 µg/kg/min), and α-adrenergic (>10 µg/kg/min) activity. Although those listed are “traditional” ranges for dose-dependent receptor agonism, the pharmacodynamics are not reliable (eg, tachycardia may occur with the lowest doses). Dopamine should be started at a low dose and titrated to the desired effect such as increased urine output, increased heart rate/inotropy, increased blood pressure or when undesired side effects limit further increases. It is the second-line agent to atropine for symptomatic bradyarrhythmias (IIa/B), alongside epinephrine and transcutaneous pacing. Infusions can range from 5 to 20 µg/kg/min.
- Epinephrine continues to be the mainstay of pharmacologic therapy for all forms of cardiac arrest (I/B-R) given its demonstrated survival benefits. Its α-adrenergic vasoconstriction of noncerebral and noncoronary vascular beds produces compensatory shunting of blood toward the brain and heart. Its β1 and β2 agonism stimulates the heart and relaxes the bronchial tree. In normal circulation, its half-life is a few minutes. The recommended dose in SCA is 1 mg IV repeated every 3 to 5 minutes (IIa,C-LD). Epinephrine is second line to atropine for symptomatic bradycardia with a target dose range of 2 to 10 µg/min (IIb/B). It is the first-line agent, however, for bradycardia associated with neuraxial anesthesia (PALS: bradycardia with a pulse but poor perfusion, 0.01 mg/kg; pulseless arrest, 0.01 mg/kg).
The optimal dose timing around defibrillation is not clear, but it is reasonable to give after the initial defibrillating shock fails (IIb/C-LD). In shock-refractory rhythms, epinephrine is combined with antiarrhythmics, including amiodarone or lidocaine. It is also commonly used in the OR in smaller, escalating doses for managing anaphylaxis and hypotension.
Studies have trialed high-dose epinephrine as high as 0.2 mg/kg but have not shown any advantage, and such doses are discouraged (III/B-R). High doses can contribute to myocardial dysfunction or even precipitate a stress cardiomyopathy.
- Isoproterenol is a β1 and β2-adrenergic agent. It is another second-line drug used to treat hemodynamically significant bradycardia unresponsive to atropine and dobutamine in the event that a temporarily pacemaker is not available. It is not stocked in code carts. Its β2 activity can cause hypotension. Isoproterenol is administered by IV infusion at 2 to 10 µg/min, titrated to achieve the desired heart rate.
- Lidocaine acts on voltage-gated sodium channels and functions as both a local anesthetic and a class Ib antiarrhythmic. In the 2018 ACLS guidelines, lidocaine was added alongside amiodarone for VF/pVT unresponsive to defibrillation, especially for witnessed arrests (IIb/B-R). It may be useful for the control (not prophylaxis) of ventricular ectopy during an acute myocardial infarction. The initial dose is 1 to 1.5 mg/kg IV and may be repeated as a 0.5- to 0.75-mg/kg bolus every 3 to 5 minutes to a total dose of 3 mg/kg followed by a continuous infusion at 2 to 4 mg/min. The lidocaine dose should be decreased for patients with reduced cardiac output, hepatic dysfunction, or advanced age (PALS: 1 mg/kg; infusion, 20-50 μg/kg/min).
- Magnesium is a divalent cation with a myriad of regulatory roles such as being a cofactor in enzyme reactions including that of the Na+, K+-ATPase, decreasing nerve and muscle conduction, relaxing bronchial smooth muscle, acting as a vasodilator, and even effecting N-methyl-D-aspartate antagonism through competition at calcium-binding sites. That said, magnesium is not recommended for general use in cardiac arrest (III/C-LD) except in specific circumstances such as for preventing recurrent long QT associated polymorphic VT (torsades de pointes) (IIb/C-LD). The dose for emergent administration is 1 to 2 g in 10 mL D5W over 1 to 2 minutes. Hypotension and bradycardia are side effects of rapid administration (PALS: 25-50 mg/kg; maximum dose, 2 g).
- Oxygen (100%) should be administered to all survivors of cardiac arrest by bag-valve-mask or advanced airway and to hemodynamically stable, breathing patients by unpressurized face mask. For neonates and infants not in cardiac arrest, high FIO2 can be deleterious and is carefully titrated to preductal SpO2.
- Procainamide is a class Ia antiarrhythmic that can be used to convert atrial fibrillation/atrial flutter to sinus rhythm and control the ventricular response to supraventricular tachycardia secondary to accessory pathways and is useful during cardioversion of wide complex tachycardias of unknown origin. It has essentially been replaced by amiodarone. The loading dose is a continuous infusion of 20 to 30 mg/min that is terminated when the arrhythmia is suppressed, hypotension occurs, the QRS complex is widened by 50% of its original size, or a total dose of 17 mg/kg is reached. When the arrhythmia is suppressed, a maintenance infusion of 1 to 4 mg/min should be initiated, with a reduced dose considered in the presence of renal dysfunction. An ECG should be examined for QRS widening at least daily (PALS: 15 mg/kg over 30-60 minutes).
- Sodium bicarbonate administration is detrimental in most cardiac arrests (III/B) because it creates a paradoxical intracellular acidosis. It can be considered when the standard ACLS protocol has failed in the presence of severe preexisting metabolic acidosis and for the treatment of hyperkalemia or tricyclic antidepressant overdose. The initial dose of bicarbonate is 1 mEq/kg IV, with subsequent doses of 0.5 mEq/kg given every 10 minutes (as guided by arterial blood pH and partial pressure of carbon dioxide [PaCO2]) (PALS: 1 mEq/kg).
- Sotalol, a type III antiarrhythmic and nonselective β-blocker can be considered alongside amiodarone and procainamide and is primarily used for atrial fibrillation/flutter and stable monomorphic VT (IIb/B). A dose of 1.5 mg/kg is given over 5 minutes for hemodynamically stable arrhythmias. Like procainamide, it should be avoided in patients with prolonged QT as it can precipitate torsade (III/B). Other side effects include bradycardia and hypotension.
- Vasopressin, a hormone from the neurohypophysis, has pressor (V1) and antidiuretic (V2) activities. Endogenous levels of vasopressin are increased in patients undergoing CPR who eventually have ROSC. It is more effective than epinephrine in maintaining the coronary perfusion pressure, has a longer half-life of 10 to 20 minutes, and was conventionally substituted for either the first or second dose of epinephrine in the treatment of pulseless arrest at doses of 40 units IV. Although vasopressin may still be considered as a substitute or in combination with epinephrine (IIb/C-LD), it has not been shown to offer any clear advantage and is no longer part of the ACLS protocol (PALS: 0.4-1 U/kg bolus with a maximum dose of 40 units for cardiac arrest and 0.0002-0.002 U/kg/min for catecholamine-resistant hypotension).
- Adenosine is an endogenous purine nucleoside with a half-life of 5 seconds. Adenosine slows or blocks anterograde AV node conduction and interrupts AV node reentry pathways to convert a stable PSVT to sinus rhythm. It can also slow the heart rate enough to identify an underlying rhythm that may be difficult to differentiate at elevated heart rates such as atrial fibrillation or atrial flutter. Adenosine can also be considered in the treatment of stable, regular, wide complex monomorphic VT. The initial dose is always a 6-mg rapid IV bolus immediately followed by a 20-mL saline flush (I/B). A brief asystole ensues, followed by P waves, flutter waves, or fibrillation waves that are initially without ventricular responses. The PSVT is sometimes converted to sinus rhythm by the initial dose, but a second injection of 12 mg may be required to terminate the PSVT if there is no effect of the first dose after 1 to 2 minutes. These doses are based on peripheral IV administration. If given via central access, the first and second doses are 3 and 6 mg, respectively.
- Specific ACLS protocols are shown in Figures 39.1-39.3.
- Pulseless arrest (Figure 39.1).
Figure 39-3 Algorithm for tachycardia with pulse.

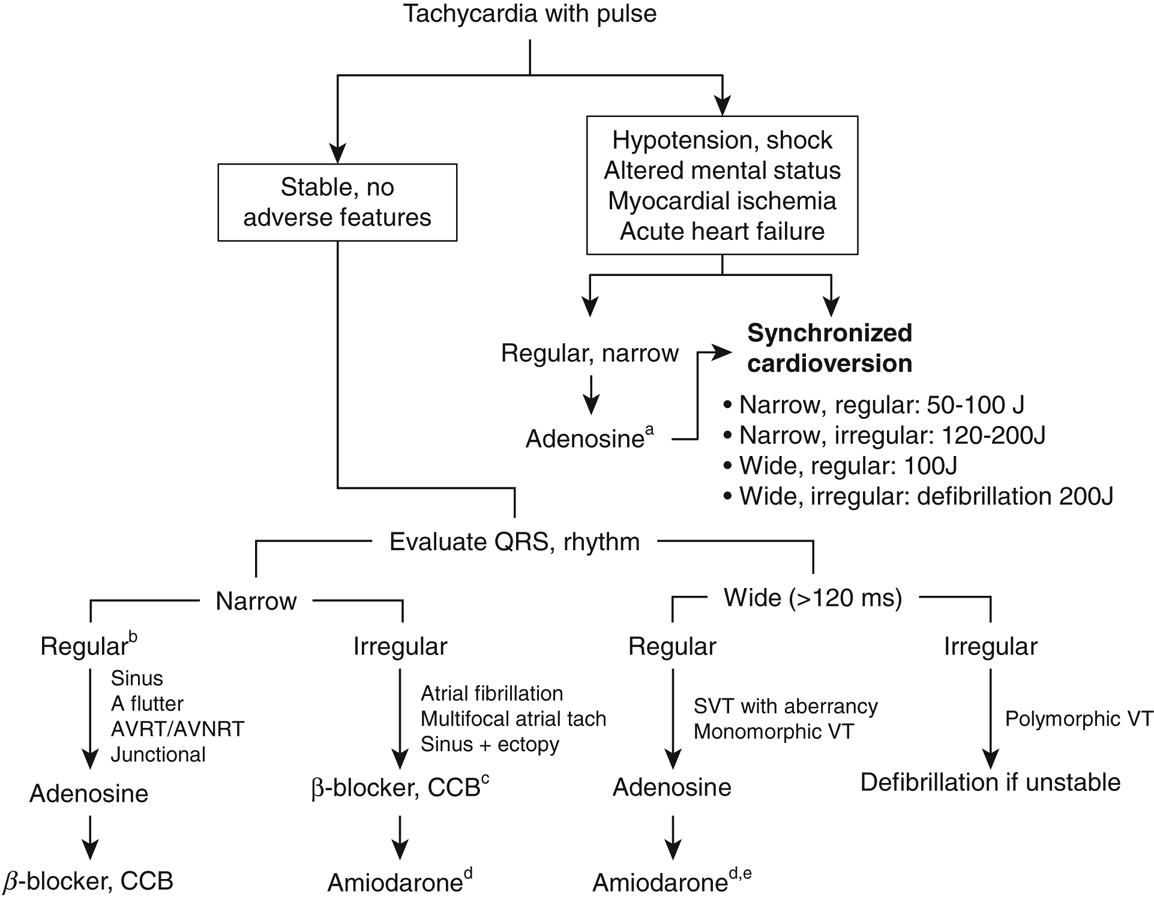
If there are signs of instability with hemodynamic compromise, the treatment of choice is immediate cardioversion. A useful estimate for peak heart rate is 220 – Age. When stable, EKG analysis and appropriate pharmacologic interventions should be attempted. aAdenosine should not be prioritized over cardioversion with unstable patients. It is given as a 6-mg IV push with a potential second dose of 12 mg (avoid with history or evidence of WPW). bConsider vagal stimulation before adenosine for stable, regular, narrow tachyarrhythmias. cGenerally metoprolol, esmolol infusion, or diltiazem push. dAmiodarone given as 150 mg IV over 10 minutes followed by an infusion of 1 mg/min. eAlternatives to amiodarone for regular, wide complex include procainamide or sotalol.
- Bradycardia with pulse (Figure 39.2).
- Tachycardia with pulse (Figure 39.3).
- Pulseless arrest (Figure 39.1).
- Open-chest direct cardiac compression is an intervention used at institutions with appropriate resources to manage penetrating chest trauma, abdominal trauma with cardiac arrest, pericardial tamponade, hypothermia, or pulmonary embolism. Direct cardiac compressions also are indicated for individuals with anatomic deformities of the chest that prevent adequate closed-chest compression (IIb/C).
- ECMO is a portable form of advanced mechanical cardiopulmonary support through invasive cannulation of large vessels. Recently, it has been referred to as extracorporeal cardiopulmonary resuscitation (eCPR). There are two forms of eCPR, venovenous (VV) and venoarterial (VA). Both provide respiratory support through external gas exchange, whereas VA provides additional circulatory (hemodynamic) support. eCPR is indicated when traditional CPR has failed, but it has many contraindications including, but not limited to, unwitnessed arrest, >30 minutes of traditional CPR without ROSC, severe bleeding, and the inability to tolerate systemic anticoagulation.
Although eCPR can achieve normal cardiac output in situations where ROSC is not attainable through traditional CPR, it is not recommended as a routine intervention and should be reserved for patients who would likely recover (I/C-EO). Institutions that offer ECMO services should have a separate emergency consult team that screens, selects, and cannulates patients.
- Termination of CPR. There are no absolute guidelines based on outcome studies to determine when to stop an unsuccessful resuscitation, but there is a very low probability of survival after 30 minutes. One objective measure is the failure to attain an end-tidal CO2 of 10 mm Hg after 20 minutes of CPR (IIb/C-LD). It is at the discretion of the physician in charge to determine when the failure of the cardiovascular system to respond to adequately applied BLS and ACLS indicates that the patient has died. There should be meticulous documentation of the resuscitation, including the reasons for terminating the effort.
- Advanced directives, such as “Do Not Resuscitate” (DNR), places the anesthesiologist in a key position with respect to intraoperative and postoperative care. It is often incorrectly assumed that a DNR order is suspended in the perioperative period. Each institution’s written guidelines should be reviewed. In advance of a procedure, physicians and the patient with the DNR status or the patient’s healthcare proxy should clarify any resuscitative measures that would be compatible with the patient’s wishes. For example, the use of a pressor to control hypotension following induction of general anesthesia might be permitted while defibrillation and CPR for spontaneous VF might be prohibited. When asked to perform an emergent intubation outside of the OR, the anesthesiologist should ask about the patient’s code status and is ethically and legally bound to a known decision to limit treatment.
- Advanced airway. Swift control of the airway optimizes oxygenation and the removal of carbon dioxide during resuscitation. Options are bag-mask ventilation or an advanced airway such as an ETT or LMA (IIb/B-R). The goal is to secure the airway via endotracheal intubation, which should be performed by the most experienced provider, often a trained anesthesiologist. Insertion of an oropharyngeal or nasopharyngeal airway can improve ventilation in an obstructed airway before intubation (IIa/C). Although cricoid pressure is sometimes used during bag-mask ventilation to decrease gastric insufflation, routine use is discouraged (III/B) as it tends to be performed incorrectly or in a manner that impairs ventilation.