- Basic life support. The need for CPR in the pediatric age group is rare after the neonatal period. Pediatric cardiac arrests usually result from hypoxemia linked to respiratory failure or airway obstruction. Initial efforts should be directed toward the establishment of a secure airway and adequate ventilation. The pediatric guidelines apply to infants between the ages of about 1 month and 1 year and to children more than 1 year of age. For newborns, see the next section. The definition of “children” for healthcare providers is patients between the ages of 1 year and the start of puberty; for the lay public, a child is defined as aged 1 to 8 years.
In contrast to the guideline of “phone first” for adult CPR, one should “phone fast” for infants and children. That is, the lone rescuer should perform five cycles (about 2 minutes) of CPR before phoning 911. The “phone fast” rule also applies to resuscitation from drowning, traumatic arrest, or drug overdose. Exceptions include witnessed and sudden arrests (eg, an athlete who collapses on the playing field) or situations in which a child is known to be at high risk for a sudden arrhythmia. Modifications to the rate and magnitude of compressions and ventilations, as well as to the hand positions for compressions are necessary because of anatomic and physiologic differences (Table 39.2). Differences between pediatric and adult resuscitation techniques are detailed below.
Table 39-2 Adult and Pediatric Cardiopulmonary Resuscitation
Airway and breathing. Maneuvers to establish an airway are the same as in the adult, with a few caveats. For children less than 1 year of age, abdominal thrusts are not used in the setting of airway foreign body obstruction since the gastrointestinal tract can be damaged easily. Hyperextension of an infant’s neck for the head tilt-chin lift may lead to airway obstruction because of the small diameter and ease of compression of the immature airway. Submental compression while performing the chin lift can also lead to airway obstruction by pushing the tongue into the pharynx. Ventilations should be given slowly and with low airway pressures to avoid gastric distention and should be of sufficient volume to cause visible chest rise and fall.
- Circulation. The brachial or femoral artery is used for pulse assessment in infants (<1 year old) because the carotid artery is difficult to palpate. Upon determination that a pulse is absent, chest compressions should be initiated. Chest compressions in infants are delivered using two fingertips applied to the sternum or by encircling the chest with both hands and using the thumbs to depress the sternum one fingerbreadth below the intermammary line (IIb/C). In older children, the correct hand position is determined as for adults, but with only one hand depressing the sternum. The chest should be compressed at least one-third of the anterior-posterior depth, roughly 1.5 in (4 cm) in infants and 2 in (5 cm) in children (IIa/C-LD). The compression-ventilation ratio is 30:2 for one-rescuer CPR of infants and children and 15:2 when two rescuers are available. If an advanced airway is in place during two-person CPR, there is no need to synchronize breaths between compressions. Ventilations should be given at a rate of approximately 10 breaths/min, and chest compressions should be given at a rate of 100 to 120/min without pauses for ventilation.
Pediatric advanced life support (PALS). Most pediatric cardiac arrests present as asystole and bradycardia, rather than ventricular arrhythmias, as they primarily occur secondary to respiratory failure or shock. In infants less than 1 year old, respiratory and idiopathic (sudden infant death syndrome) etiologies predominate. Anatomic and physiologic differences from the adult require weight-based defibrillator settings and drug dosing.
- Intubation. Low-pressure high-volume cuffed ETT have mostly replaced uncuffed ones as the ETT of choice in children. Achieving an appropriate airway seal with an uncuffed ETT often requires multiple intubation attempts, which may predispose a child to iatrogenic airway edema. Whether using an uncuffed or cuffed ETT, a correctly sized tube should have an air leak at a driving pressure between 15 and 30 cm of water. For a cuffed ETT, this leak should be tested with the cuff deflated. Once the appropriately sized cuffed ETT has been selected, the cuff can be inflated and maintained at a pressure (as measured with a manometer) between 20 and 30 cm of water.
The internal diameter (ID) of an ETT required in children less than 1 year of age is 3.5 mm uncuffed or 3 mm cuffed and 1 to 2 years of age, the size is 4 mm uncuffed or 3.5 mm cuffed. The formula for the size of ETT (ID in millimeters) in children above 2 years of age is as follows: age in years/4 + 4 for uncuffed tubes and age in years/4 + 3.5 for cuffed tubes. Appropriate oral ETT depth (centimeters at teeth) can be calculated by the formulas: inner diameter × 3 for infants and neonates and age (in years)/2 + 12 for children >1 year. Correct ETT positioning should be confirmed with capnography, auscultation, and radiographic confirmation when available. If an intubated patient’s condition deteriorates, the provider must rule out displacement or obstruction of the ETT, pneumothorax, or equipment failure (mnemonic DOPE).
- Defibrillation. Defibrillator pads/paddles used for infants are 4.5 cm in diameter, and those used for older children (>8 years, <25 kg) are 8 cm in diameter (adult size). In an emergency and if no pediatric sizes are available, adult pads on the chest and back will suffice. The energy level is 2 J/kg for the initial biphasic shock and 4 J/kg or the lowest level that was previously successful for any subsequent shocks (IIa/C-LD). Hypoxemia, acidosis, or hypothermia should be considered as treatable causes of an arrest if the defibrillation attempts are unsuccessful. For synchronized cardioversion, the starting energy is 0.5 to 1 J/kg, which can be increased up to 2 J/kg (IIb/C). The configuration for pediatric pads/paddles varies among defibrillators.
- IV access. During resuscitation, peripheral IV access is preferred over central venous access as central IV line placement may require an interruption in chest compressions. If central IV access is in place, it is the preferred route for delivery of drugs and fluids. All drugs by peripheral route should be flushed with saline to ensure delivery to the central circulation. IO access can be used in all age groups if needed.
- Medications. Many of the drugs described in the adult ACLS section apply to PALS, with doses adjusted to the child’s weight. Weight estimations can be obtained using body length tape with precalculated weights (Broselow tape) or formulas like the European pediatric life support formula [(age in years + 4) × 2 kg].
- Specific PALS algorithms are shown in Figures 39.4-39.6.
- Pediatric cardiac arrest (Figure 39.4).
Figure 39-4 Algorithm for pediatric cardiac arrest.

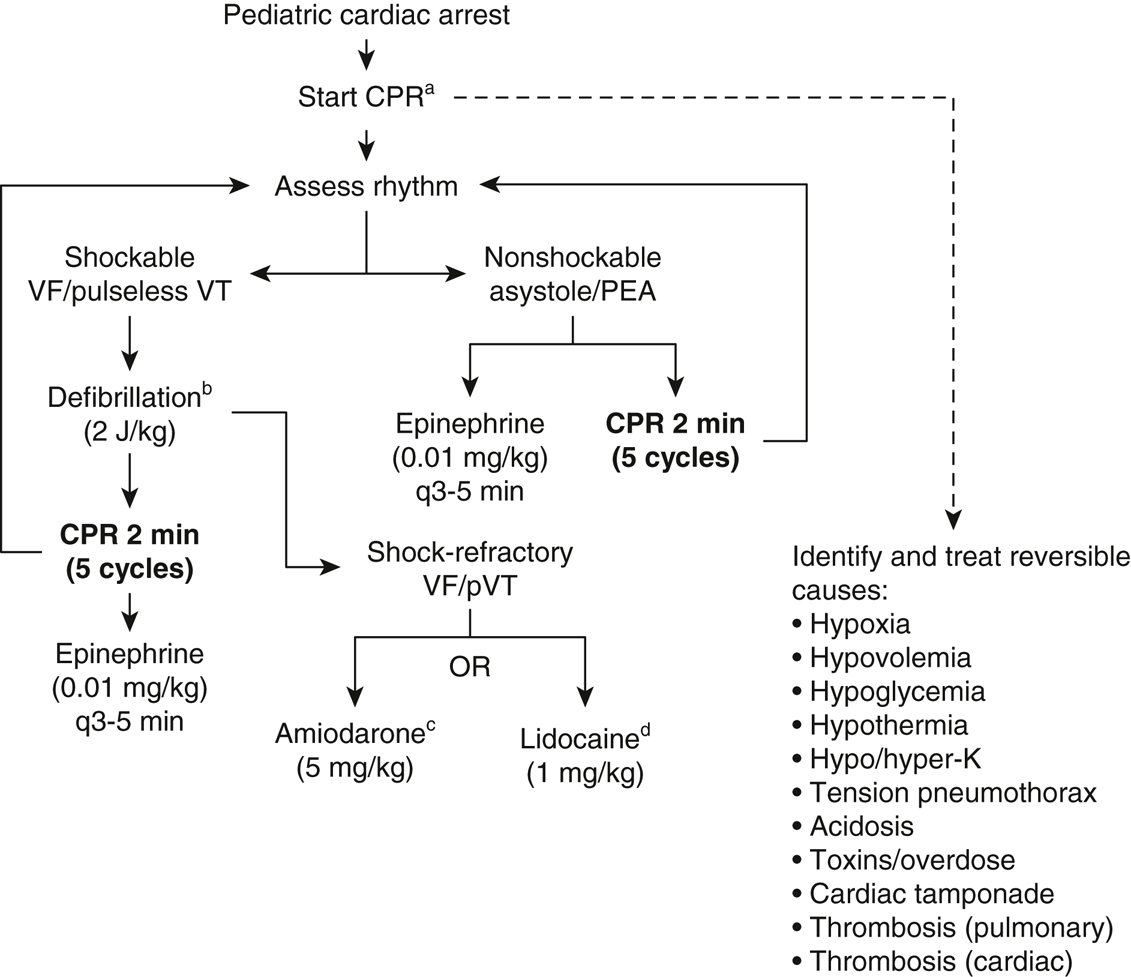
CPR, cardiopulmonary resuscitation; VF, ventricular fibrillation; VT, ventricular tachycardia. aProvide oxygen, establish intravenous or intraosseous access. bFirst shock, 2 J/kg; second shock, 4 J/kg; subsequent shocks ≥4 up to 10 J/kg or adult dose (200 J). cMay repeat up to two times for VF or refractory VT. dLidocaine can be used alternatively to amiodarone and following the bolus a maintenance of 20 to 50 µg/kg/min infusion may be used.
Figure 39-5 Algorithm for pediatric bradycardia.

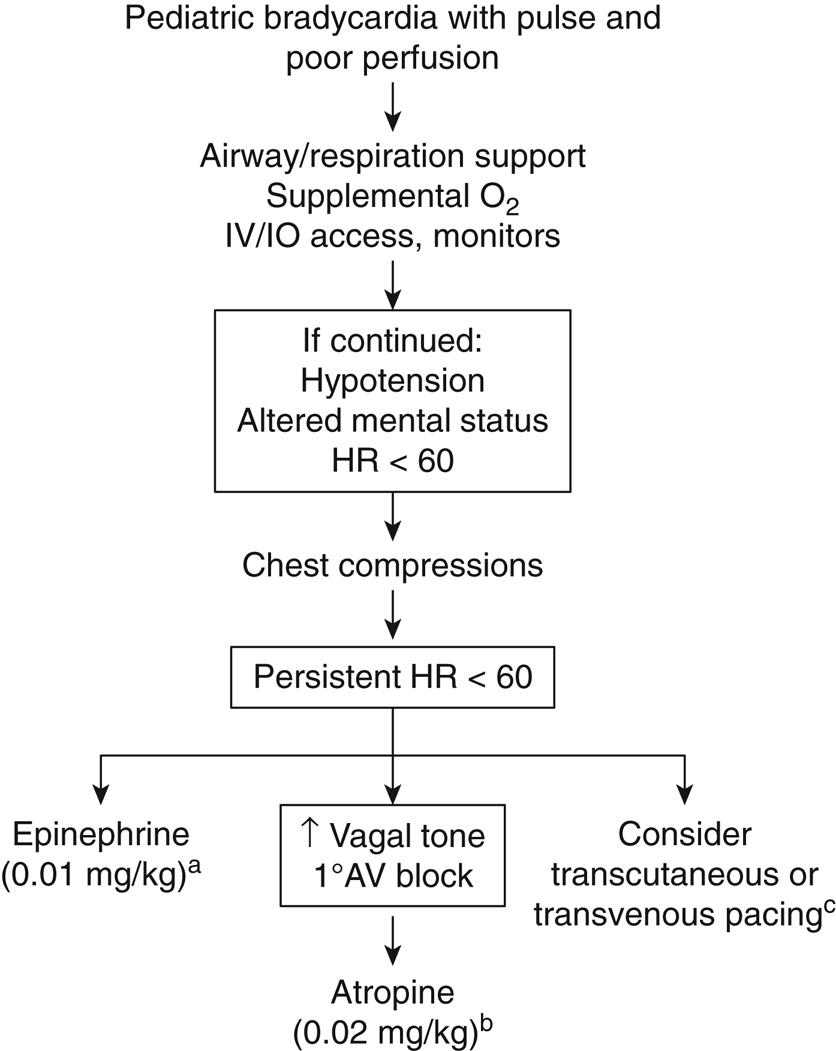
HR, heart rate; AV, atrioventricular. aMay repeat every 3 to 5 minutes. If vascular access is not available, may give 0.1 mg/kg via endotracheal tube. bMay repeat once. Minimum atropine dose is 0.1 mg; maximum 0.5 mg. If vascular access is not available, may give 0.04 to 0.06 mg/kg atropine via ETT. cTranscutaneous pacing is effective for bradycardia secondary to complete heart block or sinus dysfunction associated with a congenital heart disease but is not useful for asystole or hypoxic bradycardia. If pulse is lost, proceed to pulseless arrest PALS algorithm (Figure 39.4).
Figure 39-6 Algorithm for pediatric tachycardia with pulse and poor perfusion.

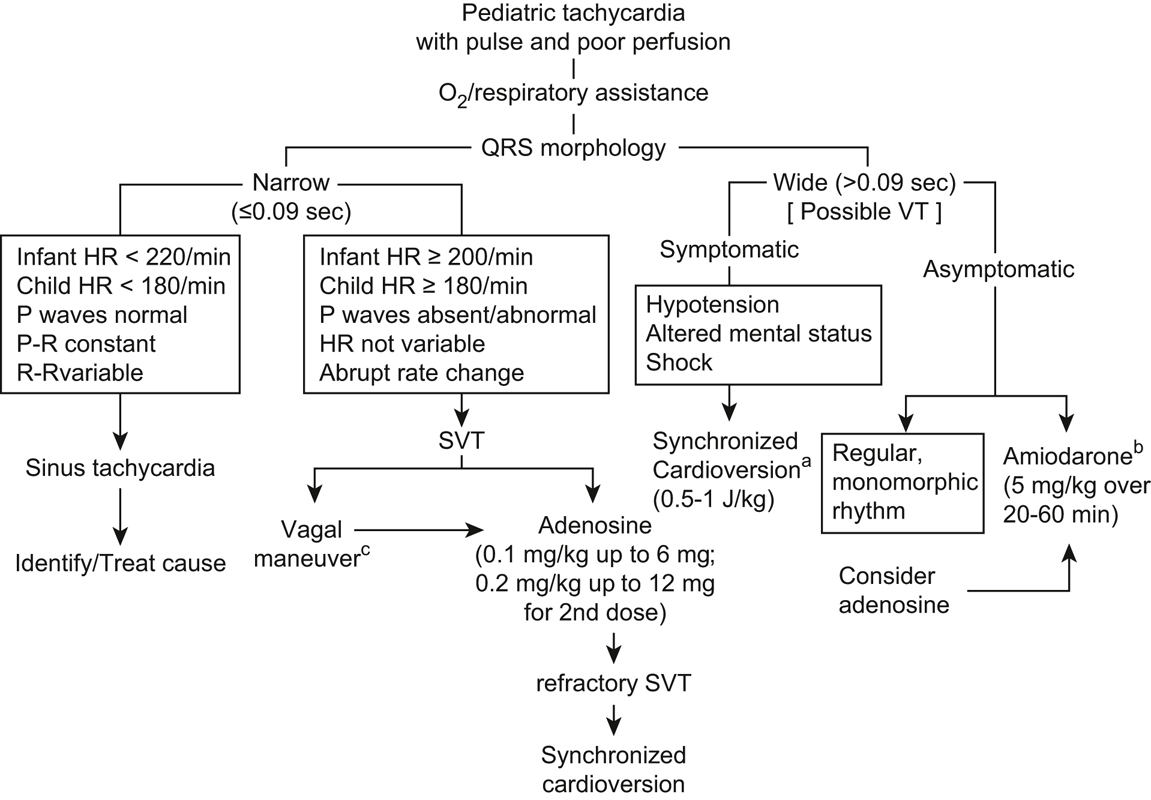
HR, heart rate; SVT, supraventricular tachycardia; VT, ventricular tachycardia. aIf not effective, increase to 2 J/kg. bAlternative to amiodarone is procainamide, 15 mg/kg over 30 to 60 minutes, but should not be given together and given with caution as can precipitate torsades. cVagal stimulation should be attempted unless hemodynamically unstable or if it would delay medical or electrical cardioversion. Can be performed with ice applied to the face of infants/young children or carotid massage/Valsalva in older children.
- Pediatric bradycardia with pulse (Figure 39.5).
- Pediatric tachycardia with pulse (Figure 39.6).
- Pediatric cardiac arrest (Figure 39.4).
- Family presence. Family presence during pediatric resuscitation is common in most institutions. Studies have shown that this is beneficial to family members, and parents should be offered the opportunity to observe the resuscitative efforts (I/B). One person should be assigned to stay with the family to explain the ongoing efforts, answer questions, and provide comfort and support. Parents can be requested to leave if they are disruptive (IIa/C). The resuscitation team should be aware of the presence of a family member.
- Intubation. Low-pressure high-volume cuffed ETT have mostly replaced uncuffed ones as the ETT of choice in children. Achieving an appropriate airway seal with an uncuffed ETT often requires multiple intubation attempts, which may predispose a child to iatrogenic airway edema. Whether using an uncuffed or cuffed ETT, a correctly sized tube should have an air leak at a driving pressure between 15 and 30 cm of water. For a cuffed ETT, this leak should be tested with the cuff deflated. Once the appropriately sized cuffed ETT has been selected, the cuff can be inflated and maintained at a pressure (as measured with a manometer) between 20 and 30 cm of water.