- Needles used for nerve blockade
Needle gauge should be the smallest possible for patient comfort. A 22-gauge needle is used most commonly. Short-beveled needles (45°) have become standard for peripheral nerve blocks. Insulated needles used in nerve stimulator-guided techniques have a small conductive area at the needle tip allowing for more accurate nerve stimulation at lower amplitudes of current. Ideal needle length varies by block. Upper- and lower-extremity blocks are best performed with a 50- to 150-mm needle depending on nerve depth. Echogenic needles designed for use in ultrasound-guided techniques have modifications such as special coating, scoring of the needle’s surface, and reflector placement to enhance reflection of ultrasound waves and improve needle visualization.
- Connecting a large-volume (20-mL) syringe to the block needle with sterile extension tubing ensures stable needle position during aspiration and injection.
- A variety of continuous catheter kits and infusion pumps for continuous nerve blockade are commercially available.
- Nerve stimulators (Figure 21.1) designed for RA can deliver a current of 0.1 to 10.0 mA at a frequency of 0.5 to 4 Hz with a stimulus duration of 0.05 to 1.0 ms.
Figure 21-1 Nerve stimulator attached to the regional block needle.
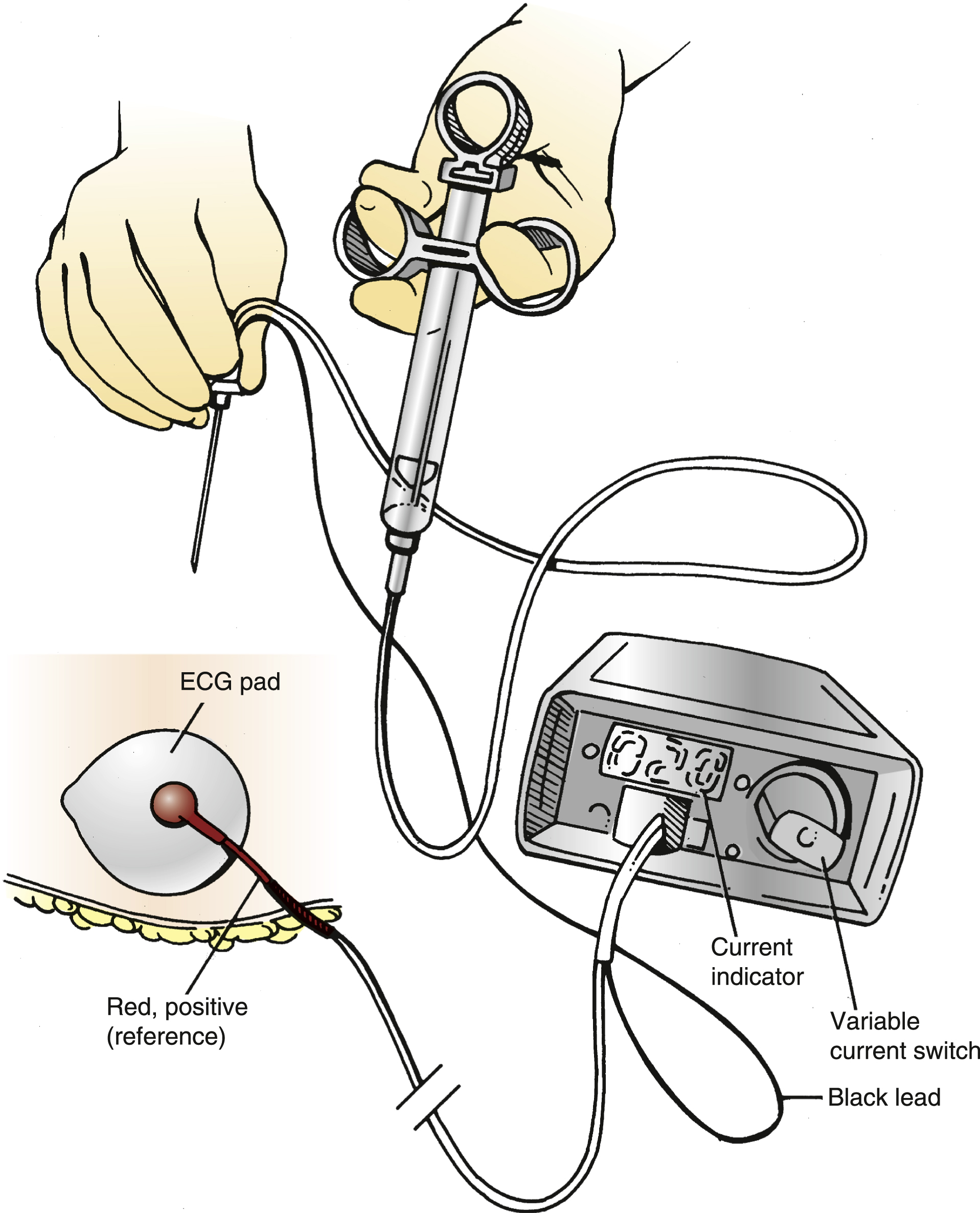
The negative (black) lead is attached to the exploring needle, whereas the positive (red) is connected to a reference electrocardiogram pad used as a “ground.”
(Reprinted with permission from Mulroy MF, BernardsCM, McDonaldSB, et al. A Practical Approach to Regional Anesthesia. 4th ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2009.)
- Ultrasound machines that are portable and utilize transducers of various shapes, sizes, and frequencies facilitate imaging of relevant anatomy and serve as an alternative/adjuvant to nerve stimulator approaches. Sterile transducer covers and gel allow for real-time imaging within a sterile field.
- Selection of LA for a block depends upon the desired speed of onset and duration (see Chapter 19).
- Resuscitation drugs should be immediately accessible for any provider performing RA. Medications include lipid emulsion with dosing guidelines and resuscitation medications including, but not limited to, epinephrine. Emergency equipment should include oxygen supply, airway management devices, suction, and defibrillators.
- To provide for the safe and effective practice of RA, a designated and centralized regional anesthesia bay with equipment and nurses who are familiar and experienced with RA techniques is recommended (Figure 21.2).
Figure 21-2 Regional anesthesia bay and team.
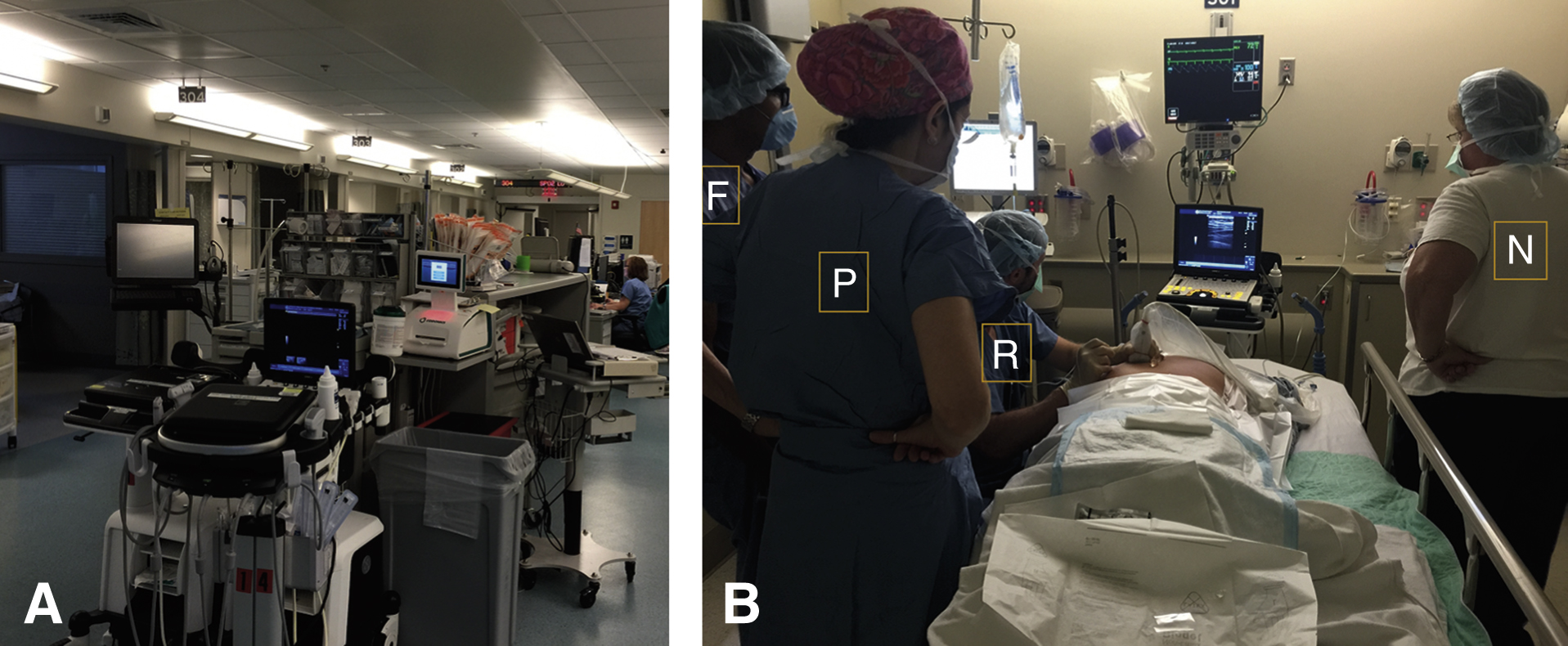
A, A well-maintained and equipped regional anesthesia bay is essential to the safe practice of regional anesthesia techniques.
B, A “block nurse” (N) who is familiar with regional anesthesia techniques is an important member of the team (physician [P], fellow [F], and resident [R]).