The neonatal period refers to the time from when a child is born and adjusting from intrauterine environment/physiology through the first month of life. About 10% of newborns require brief resuscitation at birth such as assistance with respiration, whereas 1% require more extensive interventions. At least one person who is skilled in the resuscitation of newborns should be present at every delivery. Rapid assessment of term gestation, respiration/crying, and good muscle tone (“yes” to all three predicts good outcome) helps identify babies who may require ongoing resuscitation from those who can stay with the mother. Resuscitation is often needed during an emergent cesarean section for fetal distress. In the event that the anesthesiologist is the only provider available to treat the newborn, the neonatal warmer should be brought to the head of the OR table to facilitate the treatment and monitoring of both the mother and child until a second provider (pediatrician) arrives (Figure 39.7).
Figure 39-7 Algorithm for newborn resuscitation.
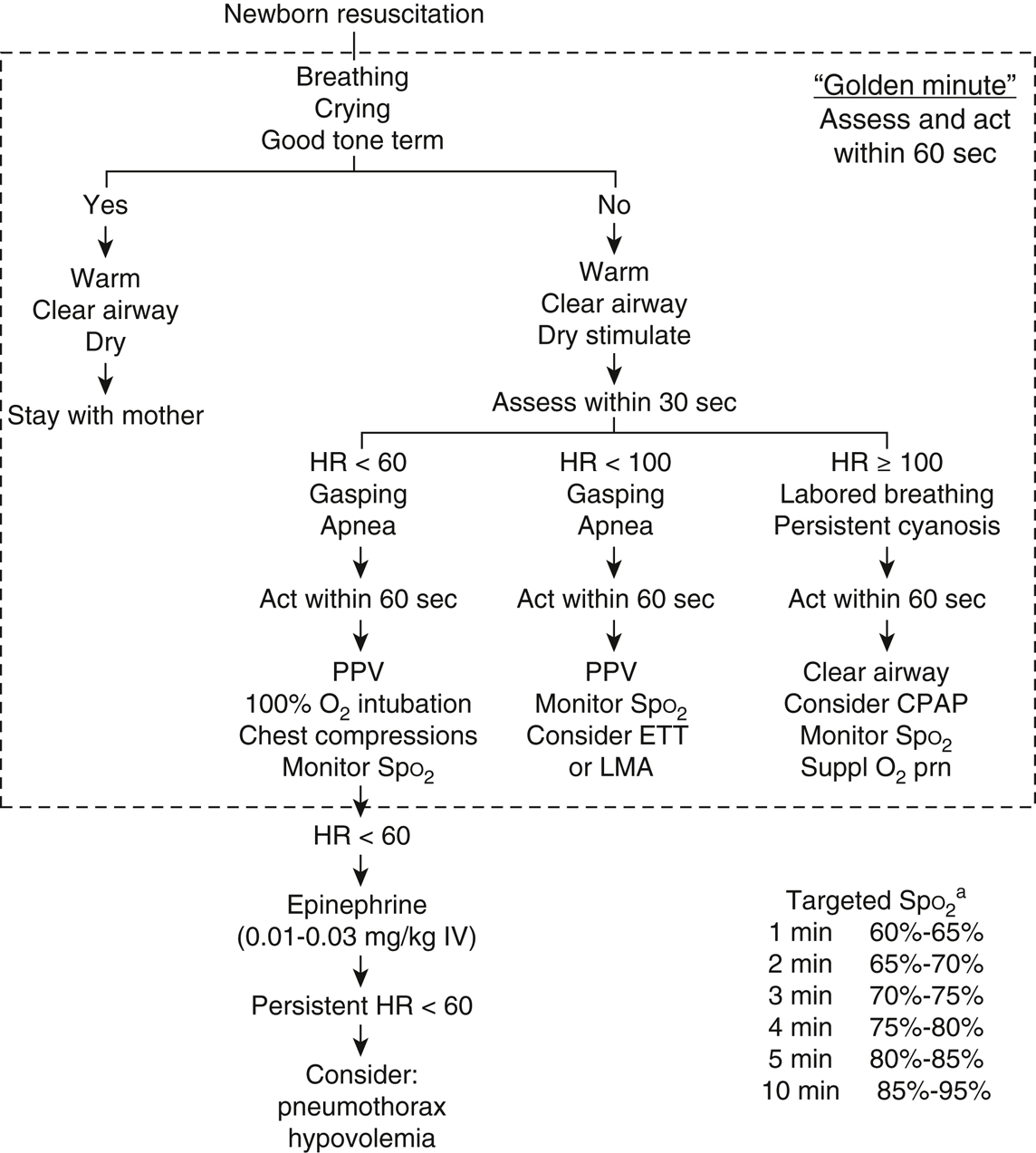
HR, heart rate; PPV, positive pressure ventilation. aTarget SpO2 refers to preductal saturation (eg, right arm) as opposed to postductal (eg, feet). For access can place IV/IO but can consider umbilical venous catheter (UVC) placement as well.
- Assessment. Immediate neonatal resuscitation is crucial, since profound hypoxemia can occur rapidly and may lead to persistence of the fetal circulation and resulting right-to-left shunting, which will exacerbate the hypoxemia. A neonate who requires resuscitation will likely have a significant right-to-left shunt.
The Apgar score is an objective assessment of the physiologic well-being of the child as it relates to heart rate, respiration, tone, reflexes, and color and is taken at 1 and 5 minutes after birth.
- An Apgar score of 0 to 2 mandates immediate CPR. Neonates with scores of 3 to 4 will need bag-mask ventilation and may require more extensive resuscitation. Supplemental oxygen and stimulation are normally sufficient for newborns with Apgar scores of 5 to 7. Respiratory activity should be evaluated by watching chest excursions and by auscultation. The heart rate is assessed by auscultation or by palpation of the umbilical pulse.
- If rapid assessment at birth regarding term gestation, crying/breathing, and good muscle tone is “yes,” then in most cases what is required is drying the baby and providing warmth (mother/wrapping). If the answer is “no,” the following four categories should be followed in sequence.
- Resuscitation. The first 60 seconds is referred to as the “Golden Minute” and is the time allotted for the initial steps and evaluation to decide if the baby requires ventilation. The decision to progress depends on the simultaneous assessment of two vital characteristics: appropriate respiration and heart rate. Once ventilation is required owing to inappropriate respiration or heart rate, ongoing assessment is based on three vital characteristics: heart rate, respiration, and oxygenation (pulse oximetry is used to avoid hyperoxia, and hence color is not recommended). An increase in heart rate with each intervention is the most valuable and sensitive indicator to a successful response.
- Initial steps. The cold-intolerant neonate should be dried thoroughly after birth and warmth provided by placing the baby under a radiant heat source. Temperature on admission to a neonatal ICU is a strong mortality predictor (I/B-NR) and should be maintained between 36.5 °C and 37.5 °C (I/C-LD). Risks of hypothermia include intraventricular hemorrhage, hypoglycemia, or delayed recognition of sepsis. Hyperthermia should also be avoided (III/C-EO). In the OR, a thermal mattress or warmed gases can be used in addition to the radiant warmer (IIb/B-R). It is unclear if there are risks with rapid rewarming (>0.5 °C/h) for newborns (IIb, C-LD).
Placement in the lateral Trendelenburg position with the head in a “sniffing” position helps to open the airway and allow secretions to drain. Routine suctioning of the oro/nasopharyngeal area is not recommended (meconium-stained or clear amniotic fluid) and should be reserved for babies with clear airway obstruction or who need positive-pressure ventilation (IIB/C). Suctioning the nasopharynx can induce bradycardia, reduce cerebral blow flow, and worsen pulmonary compliance. When necessary, clear the airway with a bulb syringe or suction catheter and use supplementary oxygen or bag-mask ventilation as needed. Drying and suctioning, however, usually provide adequate respiratory stimulation. Infants with meconium-stained amniotic fluid (vigorous or nonvigorous) are no longer routinely intubated for tracheal suctioning unless there are other reasons for intubation such as severe airway obstruction, slow heart rate or compromised breathing (IIb/C-LD).
Pulse oximetry is recommended during resuscitation to avoid hyperoxia, which has proved to be detrimental. Pulse oximetry (SpO2) and heart rate are reliably measured 90 seconds after birth with a neonatal probe. Preductal values (right upper limb) are higher than postductal. Oximetry should be used in conjunction with and not replace clinical assessment of heart rate.
- Ventilation. Positive-pressure ventilation is initiated if the baby is apneic/gasping and if the heart rate is less than 100 beats/min with shorter or longer inspiratory times. The initial peak inspiratory pressure required for chest movement and increase in heart rate is variable. If airway pressure is monitored, an initial peak pressure of 20 cm of water may be required in preterm babies and higher pressures of 30 to 40 cm of water may be required in term babies (IIb/C). If airway pressures are not monitored, the minimal pressure required for heart rate response (increase) and chest rise should be used. In a preterm baby, excessive chest expansion could create lung injury. Assisted ventilation should be delivered at 40 to 60 breaths/min for a goal heart rate of above 100 (IIb/C).
PEEP at 5 cmH2O has been shown to be beneficial and should be used if proper equipment is available for its delivery (IIb/B-R). Continuous positive airway pressure is recommended for preterm babies breathing spontaneously with difficulty, thus avoiding intubation (IIb/B-R). Endotracheal intubation is indicated in prolonged or ineffective bag-mask ventilation, during chest compression, and in special circumstances like a diaphragmatic hernia. Exhaled CO2 monitoring should be used for confirmation of correct ETT placement including in very-low-birth weight neonates (IIa/B). An LMA can be considered as an alternative to an ETT (IIb/B-R) and is suggested for infants greater than 34 weeks gestation when ETT placement is unsuccessful (I/C-EO), although their efficacy during chest compressions is unclear.
Based on studies comparing air (21% O2) and 100% oxygen for newborn resuscitation, air has been shown to have a higher survival rate and similar neurocognitive outcomes. Therefore, in term and late-preterm newborns air is most reasonable (IIa/B-R) and 100% O2 should be avoided (III/B-R). From there, the FIO2 can be titrated to achieve the targeted range of preductal oxygen saturation (target SpO2 table in Figure 39.7). If blended oxygen is unavailable, resuscitation should be started with air and if there is no improvement in 90 seconds, 100% oxygen should be used.
- Chest compressions are indicated if the heart rate is less than 60 beats/min in spite of adequate ventilation with oxygen for 30 seconds. They should be delivered on the lower third of the sternum, and the chest should be compressed approximately one-third of its anterior-posterior depth (IIb/C-LD). Compressions and ventilations should be alternated and delivered while alternating at a 3:1 ratio, with 90 compressions and 30 breaths for approximately 120 events/min (IIa/C-LD). This 3:1 ratio reflects the predominant cardiopulmonary collapse secondary to poor gas exchange in infants, although if the arrest has a clear cardiac origin, a higher ratio such as 15:2 can be used (IIb/C-EO). There are two techniques, two thumb encircling hands and the two-finger with second hand on the back. The two thumb encircling hands is recommended as it generates higher pressures and is less exhausting to the provider (IIb/C-LD).
Frequent interruption of compressions should be avoided. Periodic assessment of ventilation, heart rate, and oxygenation should be done, and compressions are stopped when the spontaneous heart rate is greater than 60 beats/min. Whenever chest compressions are provided, 100% O2 is suggested (IIa/C-EO) but reduced as soon as possible (I/C-LD). CPR is continued until the heart rate is greater than 60 (IIb/C).
- Delivery of resuscitation drugs and fluids. Resuscitation drugs should be administered when the heart rate remains below 60 beats/min despite adequate ventilation with 100% oxygen and chest compressions. The umbilical vein, the largest and thinnest of the three umbilical vessels, provides the best vascular access for resuscitation of the newborn. It is cannulated with a 3.5- to 5.0-French umbilical catheter after the umbilical cord stump has been prepped with an antiseptic and trimmed. Sterile umbilical tape placed at the base of the cord will prevent bleeding. The catheter should be placed below the skin level with blood aspirated freely, and care must be taken not to permit air into the system. If vascular access is unavailable, the ETT or IO access can be used to administer drugs.
- Medications and volume expansion
- Epinephrine. The β-adrenergic effect of epinephrine increases the intrinsic heart rate during neonatal resuscitation. Epinephrine should be used for asystole and for heart rates less than 60 despite adequate oxygenation and chest compressions. The dose of 0.01 to 0.03 mg/kg per dose of a 1:10,000 solution is recommended intravenously (IIb/C). Higher IV doses are not recommended. If the drug is given via the endotracheal route, a dose of 0.05 to 0.1 mg/kg of 1:10,000 (0.1 mg/mL) should be considered.
- Naloxone is a specific opiate antagonist used for neonatal respiratory depression secondary to narcotics administered to the mother. The initial dose is 0.1 mg/kg. Naloxone is not recommended as part of the initial resuscitative efforts in newborns. Depressed respiration due to narcotics should be treated with assisted ventilation. Studies have shown misuse of naloxone in newborn and association of seizures following administration.
- Sodium bicarbonate is not recommended for newborn resuscitation unless specifically considered during prolonged arrests in an attempt to relieve depression of myocardial function and reduced action of catecholamines induced by marked acidemia. Intraventricular hemorrhage in premature infants has been associated with the osmotic load occurring with bicarbonate administration. A neonatal preparation of sodium bicarbonate (4.2% or 0.5 mEq/mL) should be used to prevent this from occurring. The initial dose is 1 mEq/kg IV given over 2 minutes. Subsequent doses of 0.5 mEq/kg may be given every 10 minutes and should be guided by arterial blood pH and PaCO2.
- Atropine, calcium, and glucose are not recommended for use in neonatal resuscitation unless specifically indicated.
- Fluids. Hypovolemia should be considered in the setting of peripartum hemorrhage, hypotension, weak pulses, and persistent pallor, despite adequate oxygenation and chest compressions. The fluid of choice for volume expansion in the delivery room is an isotonic crystalloid or blood (IIb/C). The volume infused should be 10 mL/kg and repeated as necessary. The administration of volume expanders too rapidly to premature infants has been associated with intraventricular hemorrhage (IIa/C).
- Post-resuscitation care. After resuscitation, the baby should be in an environment where continuous monitoring and anticipatory care are provided. Maintenance of normothermia and normoglycemia is important in preventing any further injury to the brain. Therapeutic hypothermia should be offered to near-term babies with evolving moderate to severe hypoxic-ischemic encephalopathy. It should be conducted and initiated under clearly defined protocols in centers with facilities and capabilities of a multidisciplinary team.
- Guidelines for withholding and discontinuing resuscitation
- It is considered reasonable to withhold resuscitative efforts when the conditions are known to be associated with high mortality and poor outcome especially with parental consent.
- The following guidelines should be interpreted according to current regional outcomes.
- Gestation (<23 weeks), birth weight (<400 g), and congenital anomalies (anencephaly, trisomy 13) associated with high mortality (IIb/C). Resuscitation is not generally indicated.
- High rate of survival and acceptable morbidity. Resuscitation is usually indicated. Includes gestational age >25 weeks and most congenital malformations (IIb/C).
- In conditions with an uncertain prognosis, borderline survival, high morbidity, and anticipated large burden to child, parental desires concerning initiation of resuscitation should be supported (IIb/C).
- Initial steps. The cold-intolerant neonate should be dried thoroughly after birth and warmth provided by placing the baby under a radiant heat source. Temperature on admission to a neonatal ICU is a strong mortality predictor (I/B-NR) and should be maintained between 36.5 °C and 37.5 °C (I/C-LD). Risks of hypothermia include intraventricular hemorrhage, hypoglycemia, or delayed recognition of sepsis. Hyperthermia should also be avoided (III/C-EO). In the OR, a thermal mattress or warmed gases can be used in addition to the radiant warmer (IIb/B-R). It is unclear if there are risks with rapid rewarming (>0.5 °C/h) for newborns (IIb, C-LD).
- Discontinuation of resuscitation is appropriate if no heart beat is detectable after 10 minutes of efficient resuscitation. The decision to continue after 10 minutes is influenced by presumed etiology of arrest, gestational age, potential reversibility of the situation, and parents’ request.