- One lung ventilation (OLV) is achieved by isolating either the right or left lung in order to:
- Isolate ventilation in the case of a bronchopleural fistula or to protect the healthy lung from pus, blood, other fluids, or protein in the affected lung
- Facilitate surgery/exposure by collapsing one lung while the other lung sustains ventilation gas exchange during the procedure
- Lung isolation can be achieved by 3 basic methods (1,2,3) [B].
- Placing a right or left endobronchial double lumen tube (DLT)
- Placing a single lumen endotracheal tube in conjunction with a bronchial blocker (Arndt, Cohen, balloon-tipped luminal catheters) or utilizing a commercially available endotracheal tube with a built-in blocker (Univent) (4,5,6) [B]
- Placing a single lumen tube in the right or left main bronchus
- Lung isolation can also be done through a tracheostomy tube is most commonly done with a bronchial blocker (3) [B].
- Ventilation (V) perfusion (Q): The relationship between V Q determines gas exchange, with the ideal V/Q ratio being 1; however, there are physiologic regional differences.
- Alveolar lung units are said to “shunt” when V Q, whereas “dead space” results when V > Q.
- Lung base: V Q are highest in this “dependent area” when sting up. However, perfusion is proportionally greater than ventilation (V Q), creating a shunt.
- Mid-lung (Zone 2): V Q decrease at different proportions, resulting in ventilation perfusion matching (V = Q).
- Apices: V Q continue to decrease at different proportions, resulting in ventilation exceeding perfusion (V > Q) creating dead space.
- At any given time, shunting dead space occur in different areas without derangements in oxygenation or CO2 removal. Thus, V/Q matching must be understood on a spectrum based upon the number of units with mismatch, as well as the lung's ability to compensate (distal units able to upload O2 dispose of CO2, hypoxic pulmonary vasoconstriction [HPV], supplement O2).
- Bilateral ventilation with general anesthesia, different ventilatory modes, lateral position, an open chest
- Spontaneous ventilation: Anesthetic agents (volatile intravenous) decrease the functional residual capacity by impairing diaphragmatic intercostal muscle function. This results in cephalad movement of the abdominal contents decreased chest wall expansion. This increases the number of atelectatic alveolar units (V = 0).
- Lateral position: The upper lung (non-dependent) has increased compliance since the abdominal pressure is mostly exerted over the lower lung (dependent lower compliance). Perfusion remains gravity-dependent preferentially flows to the dependent lung.
- Positive pressure ventilation (PPV) muscle paralysis: Although PPV can improve V/Q matching by overcoming the abdominal pressure on the diaphragm, the non-dependent areas are preferentially ventilated while the dependent areas are preferentially perfused.
- Open chest: Exposing the non-dependent lung to atmospheric pressure increases its compliance PPV is preferentially diverted. However, perfusion remains gravity-dependent preferentially flows to the dependent lung.
- OLV: When ventilation only occurs to one side, any blood flow to the non-ventilated lung becomes shunt flow (V Q). This results in a large alveolar–arterial oxygen gradient decreased PaO2. Factors that aid with redistribution of pulmonary blood flow to the dependent lung help to maintain PaO2 in an acceptable range during surgery. Despite the effect on PaO2, it has much less effect on PaCO2. The ventilated lung is able to compensate by eliminating a higher amount of CO2 to compensate for OLV (provided that minute ventilation is maintained).
- Spontaneous ventilation: In addition to the non-dependent lung being shunted, cephalad movement of abdominal contents will also increase the number of atelectatic units in the dependent lung.
- PPV aids with offsetting the effect of the abdominal contents to the dependent, ventilated lung.
- Lateral position: Blood that flows to the non-dependent lung is shunted (there is no ventilation). Gravity shifts the blood flow towards the dependent ventilated lung. Maneuvers that “shift” blood flow to the non-dependent lung will therefore worsen shunting.
- Open chest: Exposure of the pleural cavity to atmospheric pressure on the surgical side will help initiate collapse of the non-ventilated lung, as well as further shift/defer perfusion to the dependent lung.
- HPV: A physiologic response by pulmonary capillary vessels to low oxygen tension in the alveoli. Vasoconstriction occurs, decreasing blood flow to the alveoli diverting blood to ventilated alveoli. By optimizing blood flow, the end result is a decrease in shunting.
- The lungs are contained in the chest cavity, which is formed by the rib cage, the diaphragm, chest muscles. Parietal pleura lines the inside of the rib cage.
- Each lung is surrounded by its own visceral pleura. The intrapleural space is a potential space that lies between the parietal visceral pleura has a negative pressure that “brings” together or “sucks” the two surfaces towards each other.
- The tracheobronchial tree starts with the trachea divides in a dichotomous fashion, ending in alveolar sacs.
- The trachea is about 11–13 cm long in an adult, starts at the cricoid cartilage, first divides/bifurcates at the level of T5 (carina) to form the right left main stem bronchus.
- The right bronchus is wider, diverges from the trachea at a 25° angle branches into the upper, middle, lower lobes. The right upper lobe branches at approximately 1–2.5 cm distal to the carina.
- The left bronchus diverges from the trachea at a 45° angle branches into an upper lower lobe. The left upper lobe diverges approximately 5 cm distal to the carina.
- Because of these differences, right left DLTs are slightly different in their endobronchial lumen design. Right DLTs have a side opening (Murphy's eye) close to the tip surrounded by the cuff so that it can be positioned at the right upper lobe origin to assure its ventilation; the cuff of a left DLT may inadvertently block the right main bronchus (2,7) [B].
- OLV is indicated:
- In massive hemorrhage or infection to isolate the lungs avoid spillage dissemination of infection
- To control distribution of ventilation; bronchopleural fistulas, surgical opening of conductive airway, tracheobronchial tree disruption, severe hypoxemia due to unilateral lung disease
- Exposure for surgical procedures: Aortic surgery, spine surgery, lung resection, esophageal surgery, single lung transplantation, thoracoscopy among others
- Pulmonary circulation has much less smooth muscle to control tone than systemic circulation; therefore, any increase in pulmonary arterial pressure (mitral stenosis, congestive heart failure, thromboembolism) can recruit dilate pulmonary vessels potentially interfere with HPV. Other mechanisms that have been traditionally attributed to interfere with HPV are direct vasodilating drugs (nitroglycerin, nitroprusside, etc.) volatile anesthetics.
- Prior to the initiation of OLV for surgical procedures, the patient's comorbidities should be assessed optimized to decrease morbidity (cardiac function, pulmonary hypertension, chronic obstructive pulmonary disease, coagulopathy).
- Initiation of OLV. Ventilation should be adjusted properly to minimize hypoxia.
- Start by ventilating both lungs with tidal volumes of 6–8 mL/breath, a normal I:E ratio, a rate of 8–10/min, 100% FIO2. The goal is to observe the peak plateau airway pressures.
- Upon instituting OLV, adjust the respiratory rate according to the PaCO2 without changing the tidal volume.
- If the peak plateau pressures do not increase by >5–8 mmHg, maintain the same tidal volume; otherwise, decrease tidal volume so that the airway pressure is maintained within the above-mentioned range.
- Increase the respiratory rate as needed to maintain normocarbia; keep in mind that this can indirectly increase airway pressures.
- Collapsing the non-dependent lung: Exposure of the pleural cavity to atmospheric pressure on the surgical side will initiate collapse of the lung.
- Accelerated by a higher FIO2 before lung isolation, clearing the airway of secretions, applying gentle suction to the non-ventilated lung
- Slowed or hampered by small airway diseases, secretions in the airway, tumor pressure on the airway, malpositioning of the DLT, pleural adhesion fibrosis
- Factors that aid with diverting blood flow maintaining a PaCO2 in an acceptable range during surgery:
- Passive: Gravity (lateral decubitus), pre-existing lung disease (mass), surgical manipulation interventions (ligation of vessels)
- Active (more effective): HPV
- Hypoxia:
- DLT malposition (major cause): Fiberoptic examination of the tube position is necessary in any patient with OLV hypoxia; confirm that the tube is not too deep (endolobar) or that the cuff is not herniating upwards into the carina (8) [B].
- Shunting: Interventions to decrease shunting depend upon the severity of hypoxia. If mild, consider starting with continuous positive airway pressure (CPAP) to the non-dependent lung followed by positive end expiratory pressure (PEEP) to the dependent lung (may “shunt” blood to the non-dependent lung worsen hypoxia). When acute or severe, temporary re-expansion of the non-dependent lung /or clamping of the pulmonary artery to the non-dependent lung (if surgical conditions permit).
- Secretions: Can cause localized hypoventilation, which can be improved by suctioning
- Decreased cardiac output: Can impair oxygen delivery to tissues. Increasing the CO may improve hypoxia by improving mixed venous O2.
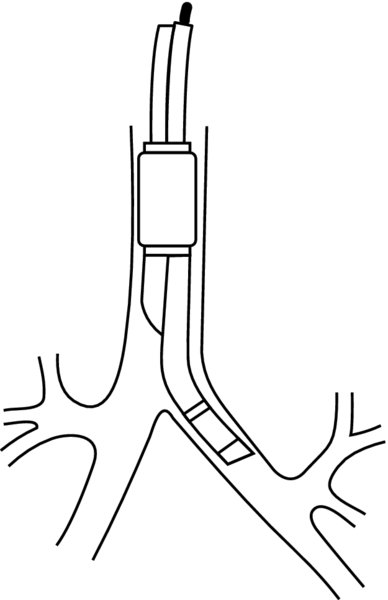
FIGURE 1. Left-sided double lumen tube.
The endobronchial lumen sits in between the carina left upper lobe. There is an increased margin for error while positioning, even for right sided lung surgeries procedures, a left DLT is commonly placed (with ventilation to the left lung/dependent lung through the endobronchial lumen).
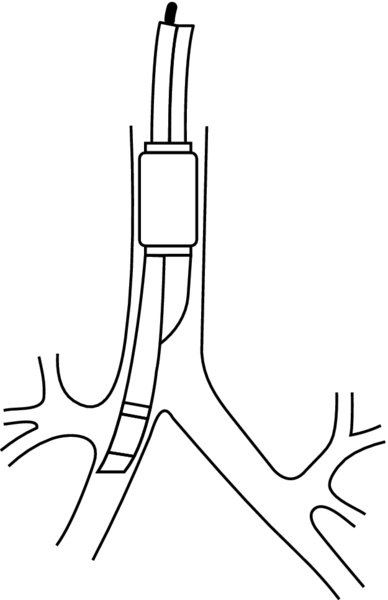
FIGURE 2. Right-sided double lumen tube.
The endobronchial lumen sits below the carina. However, because of the shorter distance between the carina right upper lobe takeoff, there is little margin for error while positioning. In order to avoid occlusion shunting of the right upper lobe, a Murphy's eye is embedded into the endobronchial cuff to allow ventilation. Ventilation also occurs through the endobronchial lumen.
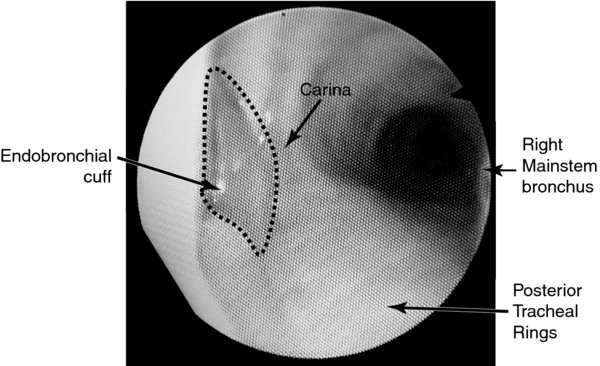
FIGURE 3. Fiberoptic view of a properly positioned left double lumen tube via the tracheal lumen.
The carina should be visualized along with the endobronchial cuff slightly above the bronchial lumen. The posterior tracheal rings can aid with identifying that the view is of the trachea, not endobronchial.