Description
- Tube thoracostomy is performed to drain collections of fluid or air in the pleural space. If the collection is compressing the lung, removal can result in re-expansion and improved V/Q matching. If the air collection is under pressure (e.g., tension pneumothorax), removal can be life saving.
- Tube thoracostomy was initially introduced in the early 1870s; however, there is evidence that Hippocrates (circa 400 BC) initially considered drainage of the pleural compartment.
- The pleural space is a potential space between the parietal pleura on the inside of the chest wall and the visceral pleura that lines the outside of the lungs (pleura are thin layers of tissue). The space contains a small amount of serous fluid to "lubricate" movement.
- The pleural space's negative pressure bestows function. Because parietal pleura adheres to the inside of the stiff chest wall space, the negative pressure in the pleural space serves to "draw" or "pull" the visceral pleura (along with the adherent lung tissue) outward. This prevents lung collapse.
- Fluid and air collections in the pleural space are pathologic; they prevent adequate lung expansion (ventilation/perfusion mismatch) and create tension (positive pressure capable of shifting the mediastinum).
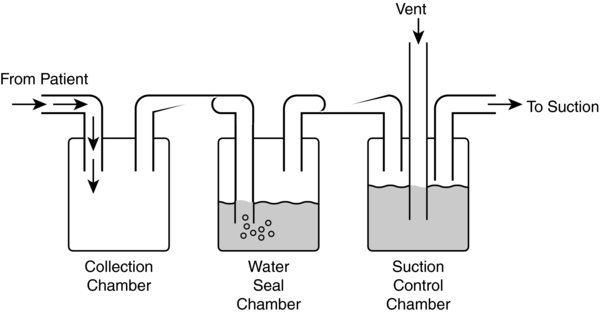
- The chest tube (a.k.a. tube thoracostomy), provides a conduit for the removal of air and fluid collections from the pleural space. By attaching to a drainage system (typically comprised of 3 chamber compartments), "one-way" flow out of the pleural space can be established.
- The system works by combining the following physiologic principles: positive pressure within the thoracic cavity facilitates extrusion of air and fluid; gravity facilitates drainage of fluid; air rises in a fluid column; suction facilitates flow of air and fluid out of the pleural cavity.
- Positive pressure. During spontaneous ventilation (SV), thoracic cavity pressure is positive on exhalation and negative during inhalation (downward movement of diaphragm and outward expansion of rib cage). Therefore, air and fluid are extruded out of the pleural cavity when the patient exhales. During positive pressure ventilation, thoracic cavity pressure is positive during inhalation, but negative/reduced during exhalation. Therefore, air and fluid are extruded out of the pleural cavity during inhalation.
- Chest tubes. Clear plastic of varying internal diameter (8F, 12F, 16F, 20F, 24F, 28F, 32F, 36F) that is inserted into the patient's pleural cavity and connects to the drainage system. The portion within the pleural cavity contains multiple orifices that improve drainage. Smaller diameter tubes may be placed via the Seldinger technique; however, they are more prone to clotting from blood or fluid and therefore may be more appropriate for air collections. Additionally, a radiopaque line facilitates visualization on chest radiography.
- Drainage system (collection chamber, water seal chamber, suction control chamber)
- Collection chamber. Connects to the chest tube; air and fluid empty directly into this chamber via gravity, suction, and positive pressure within the chest wall. The chambers are calibrated, allowing for fluid measurement. Fluid remains here and does not enter the other chambers, or flow back into the pleural space as long as the gravitational gradient is maintained. Because air rises in a fluid column, the chambers are set up such that air enters at the bottom of a fluid-filled chamber and can only move upward (creates one-way flow).
- Water seal chamber. Middle chamber; partially filled with water. Air from the collection chamber enters the bottom of this chamber and bubbles upward. Reentry of air cannot occur (air cannot move down a fluid column) and one-way flow is established. This is critical, because air would otherwise be able to reenter the pleural cavity.
- Air leak: Describes bubbling in the water seal chamber which indicates that air is present in the pleural space.
- Air leak meter: Allows for a qualitative measurement of the air leak (not quantitative; increased or decreased)
- Calibrated manometer: Allows measurement of the negative pressure in the pleural cavity. As intrapleural pressures become negative, the water level rises. Once negative pleural pressures are re-established, "Tidaling" occurs. Tidaling describes the rising and falling water level that corresponds with negative and positive pressures in the pleural cavity, respectively (SV: Rises with inhalation, falls with exhalation).
- High negativity float valve and relief chamber: Safety features that safeguard ill-effects of high negative pressures that may occur with coughing, chest tube stripping, or disconnected suction.
- Suction control chamber. The most distal chamber and connects the suction source to the water seal chamber. Serves to control the level of suction, thereby protecting the pleural cavity from excessive negative pressures. Water in this chamber serves as a barrier or buffer between the suction source and patient (allows for a more "gentle" suction and helps safeguard against the ill-effects of accidental excessive suction). Thus, the height of water in this chamber determines the amount of suction transmitted to the pleural cavity.
- Placement occurs with the patient supine, with the head slightly raised (30°). Expose the axilla by raising and abducting the arm, or placing the hand behind the head.
- Chest tube insertion point is performed between the 3rd and 5th intercostals space at the midaxillary line.
- A scalpel is used to make a superficial incision that follows the orientation of the ribs, followed by blunt dissection through subcutaneous tissue with a curved hemostat. Following identification of the parietal pleura (adheres to the inside of the ribs), the pleural tissue is punctured to enter the pleural space (rush of air or fluid occurs). The tract is dilated with the proceduralist's finger and adhesions are swept away. The chest tube is introduced with a hemostat in the direction of the air or fluid collection to a distance sufficient for all drainage holes to be within the chest. Once in situ, the chest tube is secured at the skin with a mattress suture, occlusively dressed, and connected in a sterile fashion to a drainage system. When smaller chest tubes are placed, a Seldinger technique may be used to guide the chest tube.
- Correct positioning is often confirmed with a chest radiograph following chest tube placement.
- Relative contraindications (or concerns) to chest tube placement include bleeding diatheses, infection over the chest tube insertion site, pulmonary bullae, or lung densely adherent to the chest wall throughout the hemithorax.
- Placement of a chest tube has a complication rate ranging from 3% to 16% and includes improper placement resulting in an inability to drain the desired air/fluid collection; diaphragm, pulmonary, splenic, hepatic, or gastric laceration; intercostal artery bleeding; unilateral pulmonary edema following rapid removal of a large pleural effusion or pneumothorax; thoracic empyema; and persistent air leak.
Physiology/Pathophysiology
- Indications for the placement of a chest tube include pneumothorax, hemothorax, chylothorax, empyema, and pleural effusions.
- Pneumothorax. Air collections can occur from a breach in the pleural tissue, either parietal or visceral. Causes include trauma, thoracic cavity surgery, pulmonary disease (chronic obstructive pulmonary disease [COPD], blebs/bullae, adult respiratory distress syndrome [ARDS], Marfan's syndrome, multiorgan dysfunction), complications of central line or peripheral nerve block placement, and bronchopleural fistulas. The effects can range from subclinical (where a small portion of the visceral pleura becomes detached from the parietal wall), to life-threatening (tension pneumothorax).
- Fluid collections can result from breaches in the pleural tissue or oncotic/osmotic pressure pathology. Causes include hemothorax (from surgical or traumatic injury), chylothorax (lymphatic blockade), and empyema, and pleural effusions (CHF, malignancy, cirrhosis, nephritic syndrome, lupus). The effects are due to impairment of lung expansion and vary depending on size and time of accumulation. Unless a breach in the pleural tissue occurs, they do not necessarily interfere with the negative pressure within the pleural space (thus, do not necessarily result in complete lung collapse or life-threatening tension scenarios).
- Pulsus paradoxus is an exaggeration of the normal variation of systolic BP during the inspiratory phase of respiration. Normally, during inhalation the systolic BP will fall <10 mm Hg. In certain disease states where there is an increased intrathoracic pressure, the systolic pressure will fall >10 mm Hg. These disease states include pneumo/hemothorax, pleural effusion, hemomediastinum, and COPD.
- Management practices regarding criteria and method of removal as well as monitoring with chest radiography are variable and depend on the clinician and institution.
- Intensive care unit (ICU) management: Management is centered on daily evaluation concerning the need to keep the chest tube in situ. Clinical picture, hemodynamic stability, pleural output, continued bleeding, bronchopleural fistula, and appearance on chest radiographs are factors that help management
- An air leak can occur if there is a leak in the tubing or if the openings along the lumen of the tube are outside of the chest wall. It can also occur if there is a bronchopleural fistula – one of the most feared complications of chest tube placement.
- Volume of chest tube drainage. Studies suggest <2 mL/kg/day or <200 mL/day (whichever is less) may be appropriate for chest tube removal.
- Removal may be done at end-inspiration or end-expiration. Studies have not shown a difference in the recurrence of pneumothorax.
- After resolution of air leak/drainage, removal on water seal may result in increased recurrence, hospital stay, and number of chest radiographs ordered (compared to placing the patient on suction for 24 hours, and then removing).
- Tube stripping. Conducted by some to prevent clotting (which can create a tension situation in the chest), however, has the potential to create large negative pressures or tissue injury to the lung.
- Chest radiography after removal is often performed; however, studies also demonstrate that clinical exam and judgment may be sufficient.
- Daily chest radiographs may not be indicated
- Management outside of ICU
- Water seal chamber evaluation prior to the procedure is crucial to intraoperative management. Look to see if there are bubbles – their presence indicates an air leak. If the bubbles coincide in time to the respiratory cycle, there may also be a bronchopleural fistula.
- Look for tidaling during the respiratory cycle, this respiratory swing indicates a patent system.
- A bubbling chest tube should not be clamped. This can lead to accumulation of air and formation of a tension pneumothorax.
- Unless there are extenuating clinical circumstances, keep the drainage system upright and below the patient so as to allow drainage of any fluid to gravity. Keep on water seal so as to prevent flow of air into the pleural space.
- Only attach to suction if there may be an accumulation of fluid/air in the pleural cavity.
- Be prepared to deal with malfunction and even dislodgement of the chest tube. This may necessitate replacement of the chest tube on an emergent basis.