Description
- The 12-lead EKG is a noninvasive test that provides information on the electrical function of the heart and aids in the diagnosis of pathophysiologic processes.
- Serves as a baseline for perioperative changes and as a screening tool to identify cardiac abnormalities.
- Continuous 3- or 5-lead EKG is an American Society of Anesthesiologists (ASA) standard monitor used for general anesthesia and monitored anesthesia care.
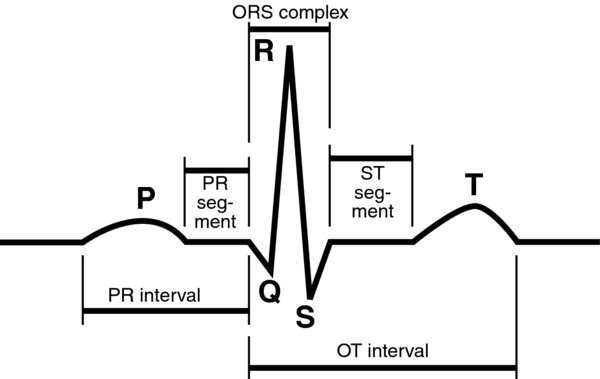
- P wave (80 ms): Denotes atrial depolarization. Myocardial depolarization is normally initiated by spontaneous sinoatrial (SA) node depolarization. The signal is quickly and efficiently conducted along a specialized conduction pathway. In the atria, this pathway is via interatrial tracts (anterior, middle, and posterior); they begin by depolarizing the right, followed by the left, atria. The conduction cells depolarize adjacent myocardial cells, which have a different histology.
- QRS (80–120 ms): Denotes the varying stages of ventricular depolarization. The Q wave is the initial negative deflection and results from septal depolarization. The R wave follows and is the first positive deflection. It results from depolarization of the larger, more muscular left ventricle; right ventricular depolarization is normally obscured. The S wave is the final negative deflection caused by lateral wall depolarization.
- T wave: Denotes ventricular repolarization. The beginning of the wave represents a period of absolute refractoriness, where a subsequent depolarization (no matter how strong) cannot initiate a aberrant rhythm. The latter portion of the wave is a time of relative refractoriness, where a strong enough depolarization can result in a runaway rhythm.
- PR interval (120–200 ms): Time from the start of atrial depolarization to atrioventricular (AV) nodal conduction to conduction through the His-Purkinje system.
- QRS width: Represents the time for ventricular depolarization
- J point: Describes the intersection between the QRS complex and ST segment. When the heart rate is increased, atrial repolarization may be observed at the very end of the QRS complex as J point depression.
- ST segment: Denotes the end of depolarization to the beginning of repolarization and is usually isoelectric
- QT interval (QTc <440 ms): Beginning of ventricular depolarization to the end of ventricular repolarization. Time for ventricular repolarization is heart rate dependent; thus, the QT is usually corrected for heart rate (QTc).
- Rate: Typically measured between sequential R waves; the RR interval (0.6–1.2 s) is useful due to its prominent wave that allows for easy detection. A rate <60 bpm is bradycardia; a rate >100 bpm is tachycardia.
- Rhythm: The location of regular P waves preceding each QRS suggests an atrial rhythm. The relationship between the P wave and QRS complex provides information about underlying conduction defects or dissociation.
- Axis: The average direction of the various complexes determines the axis. The normal QRS axis is between 0 and 100° in the frontal plane. Left or right axis deviation can suggest underlying pathophysiology.
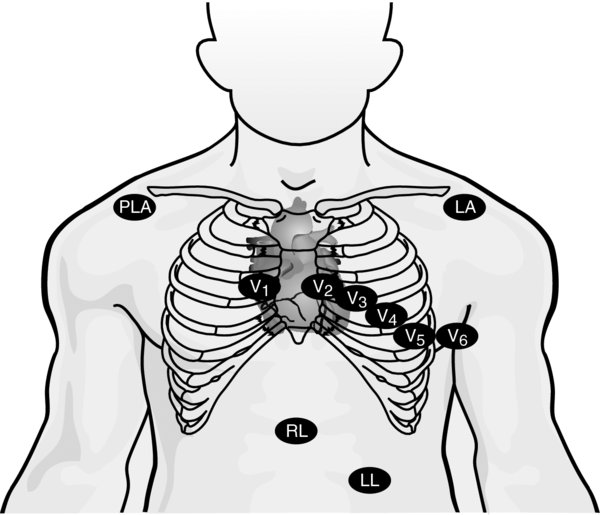
- A total of 12 leads allows for "visualizing" the electrical function from different angles through the heart. Considering the leads in different combinations can aid in clinical diagnosis.
- Standard limb leads (I, II, III): form the points of Einthoven's triangle, an equilateral triangle whose vertices lie at the left and right shoulders and the pubic region and whose center corresponds to the vector sum of all electric activity occurring in the heart at any given moment. This allows for the determination of the electrical axis.
- Augmented limb leads (aVR, aVL, aVF): Together with the standard limb leads, record the electrical activity along the frontal plane.
- Precordial leads (V1, V2, V3, V4, V5, V6): Record the electrical activity along the horizontal plane.
- Anterior leads (V3 and V4): Allow evaluation and assessment of the electrical function of the anterior wall of the heart. Usually supplied by the left anterior descending artery.
- Inferior leads (II, III, and aVF): Allow evaluation and assessment of the electrical function of the inferior heart muscle. The inferior wall is usually supplied by the right coronary artery.
Physiology/Pathophysiology
- ST segments: Ischemia or infarct may present as either elevation or depression of the ST segment. A routine preoperative EKG may appear normal if a patient is not experiencing active ischemic symptoms. Thus, a high index of suspicion must be maintained for patients at risk for coronary ischemia.
- Axis deviation: Common conditions associated with left axis deviation include left bundle branch block or left anterior hemiblock, inferior MI, or left ventricular hypertrophy. Common causes of a right axis deviation include right ventricular hypertrophy, chronic lung disease, right bundle branch block, or lead reversal.
- Bundle branch blocks: A prolonged QRS suggests either a right (RBBB) or a left bundle branch block (LBBB). They are described as either partial (QRS <120 ms) or complete (QRS >120 ms). Although a RBBB can represent pulmonary or right heart disease, it is more commonly benign. Alternatively, a LBBB is more likely to indicate underlying cardiac pathology (CAD, CMO, valvular disease). A new onset LBBB should prompt a thorough cardiac workup. The anterior or posterior fascicle of the left bundle may be blocked in isolation (termed hemiblock). A nonspecific intraventricular conduction delay describes a nonpathologic widening of the QRS complex that does not meet the criteria for either LBBB or RBBB.
- AV blocks: Impaired conduction between the atria and ventricles of the heart are described as first, second, and third degree. First-degree AV block is defined as a PR interval >0.2 s. Second-degree AV block may be Type 1 (Mobitz 1, Wenckebach), defined as progressive prolongation of the PR interval with eventual dropped QRS; or Type II (Mobitz 2), where the PR remains unchanged prior to the sudden failure of conduction of a P wave and a dropped ventricular beat. In third-degree AV block, there is no association between P waves and QRS complexes. While first-degree and Mobitz I AV block are generally benign conditions, Mobitz II (can progress to complete heart block) and third-degree AV blocks are indications for cardiac pacing.
- P waves: Abnormal P wave morphology may indicate an ectopic atrial rhythm, whereas a changing P wave morphology may suggest either a wandering atrial pacemaker or multifocal atrial tachycardia. An irregular rhythm with no clear P waves suggests atrial fibrillation. A regular "saw tooth" pattern may suggest atrial flutter.
- Arrhythmias: A narrow QRS suggests a supraventricular (above the ventricles) rhythm while a wide QRS suggests either a ventricular source or aberrant conduction of a supraventricular rhythm.
- QT prolongation: Prolonged QTc is a risk factor for developing ventricular arrhythmias (Torsades de Pointes) and is an independent risk factor for sudden cardiac death. QTc may be prolonged due to genetic causes (long QT syndrome), drugs (haloperidol, methadone), or diseases (hypothyroidism).
- Delta waves: Describes a slurred upstroke of the QRS complex and is found in patients with Wolff–Parkinson–White (WPW) syndrome. WPW is caused by the bypass of the AV node via an accessory pathway called the bundle of Kent. This accessory pathway does not have the rate-slowing property of the AV node, thus allowing for extremely fast heart rates and potential hemodynamic instability. The combination of cardiac arrhythmias and an accessory pathway may degenerate into ventricular fibrillation.
- R on T phenomenon: The beginning of the T wave is a time of absolute refractoriness; the latter portion of the wave is a time of relative refractoriness. An abnormal depolarization signal (aberrant pacemaker, PAC, PVC, cardioversion) cannot depolarize the entire ventricle during the absolute refractory period; however, it may potentially do so during the relative refractory period. This can result in degeneration into ventricular tachycardia or fibrillation.
- Artificial pacemaker: May be identified by tell-tale "pacer spikes" on EKG or telemetry. May be atrial, ventricular, or sequentially paced. QRS will appear widened if ventricularly paced.
- Medication toxicities:
- Digoxin: Characteristic downward sloping of the ST segment. May also see an increased PR and decreased QTc interval.
- Tricyclic antidepressants (TCAs): Characteristic rightward change in the frontal plane QRS vector. A large R wave in aVR is quite sensitive for TCA toxicity; may also see an increased QRS and QTc interval.
- Electrolyte abnormalities:
- Hypokalemia: EKG changes result from delayed ventricular repolarization. May include T wave flattening and/or inversion, ST segment depression, prominent U wave, increased P wave amplitude, and prolonged PR interval. Increased myocardial cell automaticity may predispose to atrial or ventricular arrhythmias.
- Hyperkalemia: EKG changes are due to delayed depolarization and hastened repolarization. Changes commonly progress in order from symmetrically peaked T waves
 widened QRS
widened QRS  prolonged PR interval
prolonged PR interval  loss of P wave
loss of P wave  loss of R wave
loss of R wave  ST depression
ST depression  EKG that resembles sine wave
EKG that resembles sine wave  ventricular fibrillation
ventricular fibrillation  asystole.
asystole. - Hypocalcemia: QTc prolongation and cardiac irritability leading to arrhythmias
- Hypercalcemia: Shortened ST segment and QTc interval
- Hypomagnesemia: PR and QT interval prolongation, cardiac irritability
- Hypermagnesemia: May see PR prolongation and QRS widening
- Intraoperative bovie, electrical interference, patient shivering, tremors, or movement may closely resemble an intraoperative arrhythmia. Close inspection may reveal the QRS "marching through" the interference; other times, it may be indistinguishable from a true arrhythmia. Close evaluation of other monitors (blood pressure, pulse oximetry or arterial plethysmograph, verification of palpable peripheral pulses) may provide clues in this circumstance.
- Malpositioning of leads may result in the appearance of ST changes. Thus, it is good practice to place leads in proper position if it does not interfere with the surgical field and to note baseline abnormalities in the EKG tracing.
- Body habitus: Large breasts or obesity may result in low-voltage EKG.
- Pulmonary artery catheters and central lines: for patients with LBBB, there is a risk of complete heart block with insertion. In this circumstance, it is prudent to have pacing capabilities readily available. Similarly, in patients with WPW, the pulmonary artery catheter or a wire for central line placement can induce a hemodynamically intolerable tachyarrhythmia.
- Extracorporeal shock wave lithotripsy: Older machines time shocks to be delivered during the R wave to prevent R on T phenomenon.
- Cardioversion: Machines synchronize the delivery of electrical discharge to the R wave to prevent R on T phenomenon.