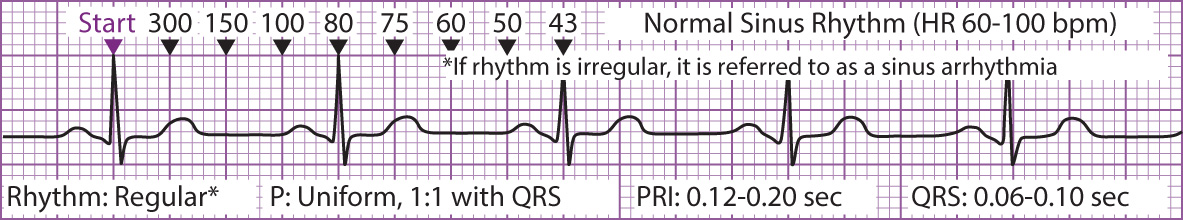
A cardiac dysrhythmia is any disturbance in the normal rhythm of the electrical excitation of the heart. It can be the result of a primary cardiac disorder, a response to a systemic condition, or the result of an electrolyte imbalance or a drug toxicity. The severity of a dysrhythmia, depending on its hemodynamic effect on the cardiac output, varies on the basis of the cause of the dysrhythmia and the myocardium's ability to adapt. An atrial dysrhythmia arises in the atria of the heart. If the dysrhythmia causes the patient to lose the “atrial kick” (the blood that is ejected into the ventricle during atrial systole), the patient may have more symptoms. The atrial kick provides approximately 35% of the total end-diastolic volume, which is an essential contribution to ventricular filling in individuals with heart disease. Atrial dysrhythmias that cause the loss of the atrial kick include atrial flutter and atrial fibrillation. Figure 1 illustrates types of atrial dysrhythmias in Lead II.
Sinus bradycardia (Figure 2), a heart rate less than 60 beats per minute, has a rhythm that is regular, with the electrical impulse originating in the sinoatrial (SA) node. There is a 1:1 ratio of P waves to QRS complexes, and the P wave and QRS complexes are of normal configuration. Sinus bradycardia is primarily caused by an excessive parasympathetic response. It can be a normal, asymptomatic occurrence in healthy individuals such as athletes or a desired medication effect with drugs such as digoxin and verapamil. Abnormal conditions such as ischemia, hypothermia, pain, anxiety, increased intracranial pressure, or myocardial infarction can also cause sinus bradycardia. Because of its effects on cardiac output, sinus bradycardia can cause symptoms of dizziness, fatigue, palpitations, chest pain, and congestive heart failure. Complications, depending on the type of dysrhythmia, include stroke, thromboembolism, heart failure, hypotension, syncope, and rarely, cardiac arrest.
Sinus tachycardia (Figure 3), a heart rate greater than 100 beats but rarely more than 150 beats per minute, is a regular rhythm whose electrical impulse originates in the SA node. There is a 1:1 ratio of P waves to QRS complexes, and the P wave and QRS complexes are of normal configuration. Sinus tachycardia is generally the result of increased stimulation of the sympathetic nervous system and the resulting release of catecholamines. It can also be a normal response to an increased demand for oxygenation, as in exercise or fever, or in response to a decreased cardiac output, as in congestive heart failure or shock syndromes. It can also occur in response to hypoxemia; electrolyte imbalance; acute fluid loss; stress; anxiety; intake of stimulants such as caffeine or nicotine, or anticholinergic medications.
Figure 1 Types of Atrial Dysrhythmias
 Figure 1 Types of Atrial Dysrhythmias
Figure 1 Types of Atrial Dysrhythmias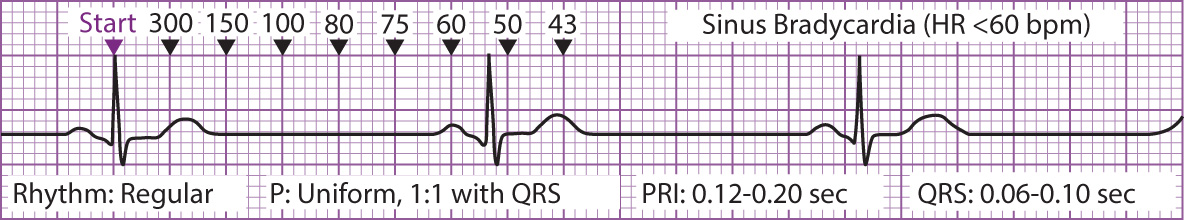 Figure 2 Sinus Bradycardia
Figure 2 Sinus Bradycardia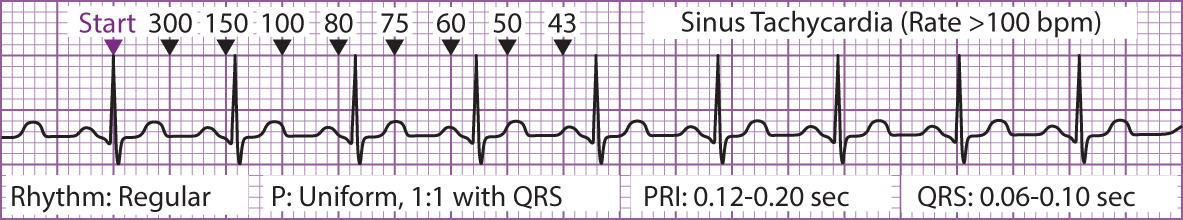 Figure 3 Sinus Tachycardia
Figure 3 Sinus TachycardiaSinus arrhythmia, defined as a variable rate of impulse discharge from the SA node, occurs when the rhythm is irregular and usually corresponds to the respiratory pattern. The rhythm increases with inspiration and slows with expiration. There is a 1:1 ratio of P waves to QRS complexes, and the P wave and QRS complex are of normal configuration. Sinus arrhythmia can be a normal variation in children. The vagal effect of some medications and of SA nodal disease and conditions that affect vagal tone can also be a cause.
Atrial flutter (Figure 4), defined as an abnormally fast, regular atrial rhythm that originates from an ectopic atrial focus, is usually in the range of 250 to 350 beats per minute. It is characterized by regular flutter or sawtooth-appearing waves. The QRS complex appears normal in configuration, and there is not a 1:1 ratio of the P to QRS complex because the ventricle cannot respond to the fast atrial rate. Atrial flutter is seldom seen in a healthy individual. Most frequently, atrial flutter is associated with ischemic myocardial disease, cardiomyopathy, acute myocardial infarction, and rheumatic heart disease. Other associated conditions include mitral valve disease, digitalis toxicity, hyperthyroidism, and chronic obstructive pulmonary disease. The patient is usually asymptomatic because of a controlled ventricular response.
Atrial fibrillation (Figure 5), a rapid and disorganized atrial dysrhythmia, occurs at atrial rates of 300 to 600 beats per minute. There are no clearly discernible P waves, but rather irregular fibrillatory waves. The QRS complex appears normal, but there is a variable, irregular ventricular response because of the atrioventricular (AV) node's ability to respond only partially to this rapid rate. Although atrial fibrillation can occur in healthy individuals, it is generally found in patients with underlying cardiovascular diseases such as ischemic heart disease, mitral valve disease, heart failure, and pericarditis. Other associated conditions include diabetes, hyperthyroidism, hypertension, valvular disease, and obesity.
Premature atrial contractions (PACs), cardiac contractions initiated in the atria, occur earlier than expected. The underlying rhythm is regular, with the early beat producing a slight irregularity. There is usually a 1:1 ratio of P wave to QRS complex unless the P wave is blocked because of the refractory period of the AV node. The P wave of the premature beat may exhibit a slightly different configuration because it does not originate in the SA node but from another area of the atrium. There may be a short “compensatory” pause after the ectopic (electrical stimulation of a cardiac contraction beginning at a point other than the SA node) beat. PACs can be a normal occurrence in all age groups or they can be the result of ischemic heart disease, rheumatic heart disease, stimulant ingestion, or digitalis toxicity.
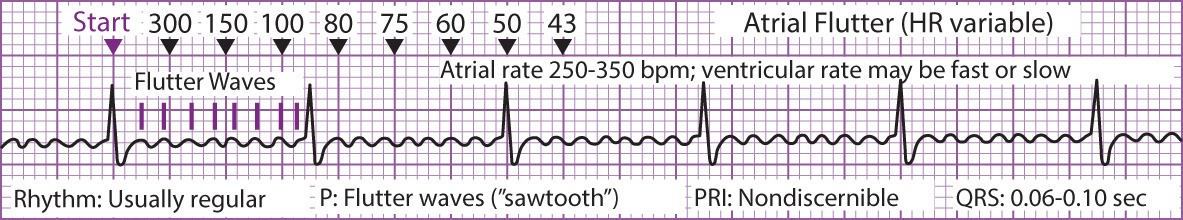 Figure 4 Atrial Flutter
Figure 4 Atrial Flutter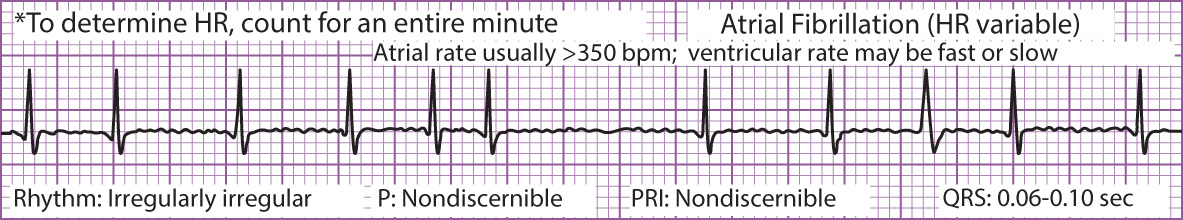 Figure 5 Atrial Fibrillation
Figure 5 Atrial FibrillationParoxysmal supraventricular tachycardia (PSVT), the sudden onset of a rapid atrial and ventricular rate of 150 to 240 beats per minute, occurs with a regular but aberrant P wave. The P waves are difficult to discern from the preceding T wave, but a P wave precedes each QRS. PSVT occurs when there is an intrinsic abnormality of the AV conduction or in conditions associated with stress, hypoxia, hypokalemia, hypertension, heart disease, or hyperthyroidism. It is also associated with digitalis toxicity, caffeine ingestion, and the use of central nervous system stimulants.