Author:
Michael D. Cabana, MD, MPH
| Table 1. | Developmental Milestones from Birth to 5 Years | |||
| Age (mo) | Adaptive/Fine Motor | Language | Gross Motor | Personal–Social |
|---|---|---|---|---|
| 1 | Grasp reflex (hands fisted) | Facial response to sounds | Lifts head in prone position | Stares at face |
| 2 | Follows object with eyes past midline | Coos (vowel sounds) | Lifts head in prone position to 45 degrees | Smiles in response to others |
| 4 | Smiles spontaneously | |||
| 6 | Palmar grasp of objects | Babbles (consonant sounds) | ||
| 9 | Pincer grasp | Says “mama,” “dada” nonspecifically, comprehends “no” | Pulls to stand | |
| 12 | Helps turn pages of book | Points to indicate wants | ||
| 15 | Scribbles | Walks independently | ||
| 18 | Turns pages of book | Walks up steps | Feeds self with spoon | |
| 24 | Solves single-piece puzzles | |||
| 30 | Imitates horizontal and vertical lines | Names all body parts | Rides tricycle using pedals | |
| 36 | ||||
| 42 | Copies cross | Understands “cold,” “tired,” ”hungry” | Stands on 1 foot for 2–3 s | Engages in associative play |
| 48 | Hops on 1 foot | |||
| 54 | Understands opposites | Broad-jumps 24 inches | ||
| 60 | Asks meaning of words | Skips (alternating feet) | Ties shoes | |
Figure 1. The normally refractive eye, common refractive errors, and their corrections.
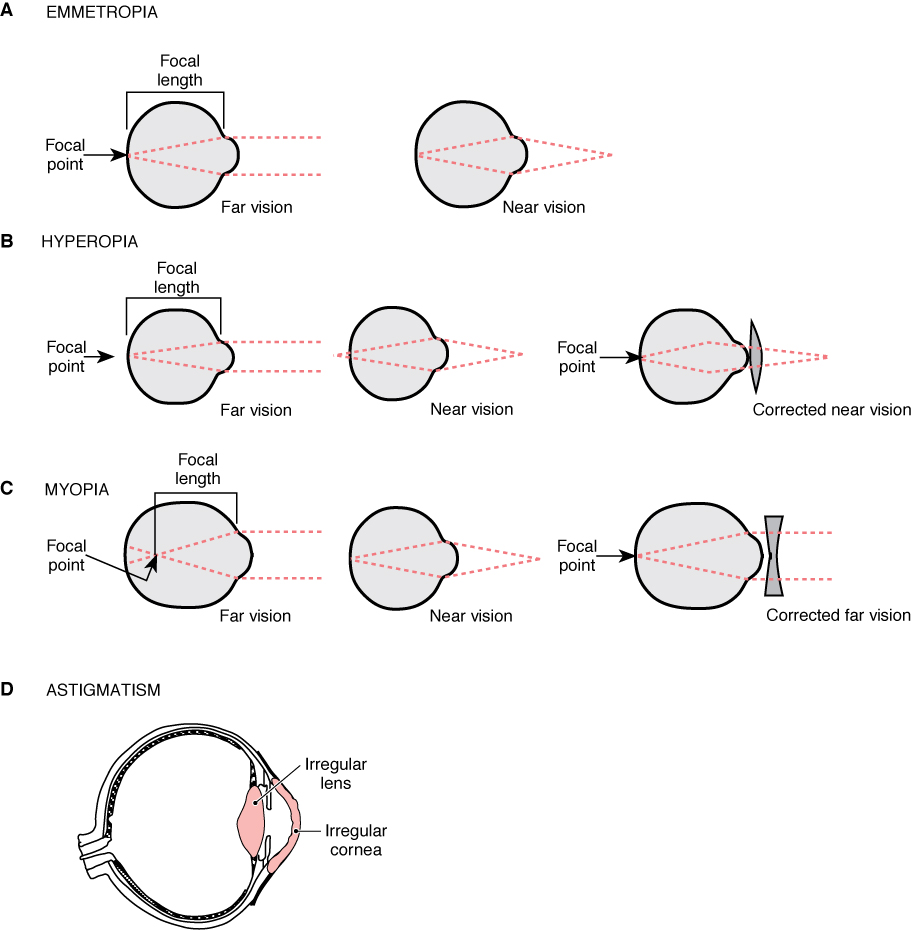 Figure 1.
Figure 1.(From BhatnagarSC .Neuroscience for the Study of Communicative Disorders. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.)
Figure 2. The Universal Numbering System.
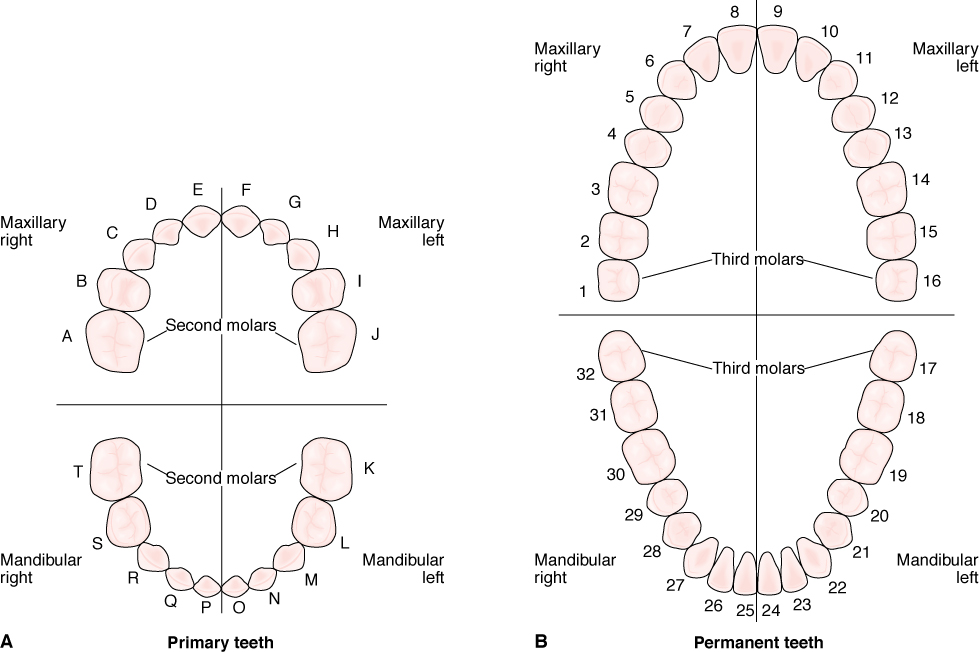 Figure 2.
Figure 2.(From Lippincott Williams & Wilkins. Lippincott Williams & Wilkins’ Comprehensive Dental Assisting. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.)
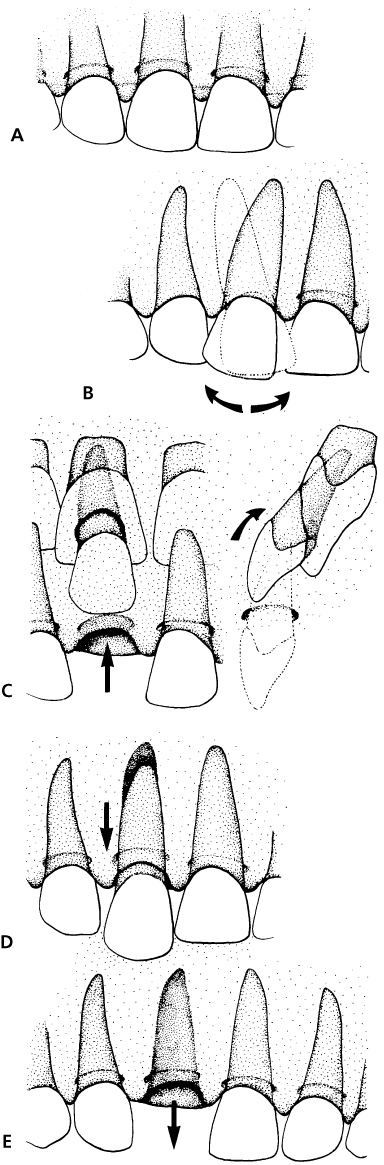
The various types of trauma to the periodontal structures: concussion/subluxation (A), lateral luxation (B), intrusion (if primary tooth is intruded, note location of developing permanent tooth bud) (C), extrusion (D), and avulsion (E). Refer emergencies B through E to the dental staff as soon as possible.
(From FleisherGR , LudwigS , HenretigFM , et al, eds. Textbook of Pediatric Emergency Medicine. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
| Table 2. | Clinical Signs of Dehydration in Children | ||
| Parameter | Mild | Moderate | Severe |
|---|---|---|---|
| Activity | Normal | Lethargic | Lethargic to comatose |
| Color | Pale | Gray | Mottled |
| Urine output | Decreased (<2–3 mL/kg/h) | Oliguric (<1 mL/kg/h) | Anuric |
| Fontanelle | Flat | Depressed | Sunken |
| Mucous membranes | Dry | Very dry | Cracked |
| Skin turgor | Slightly decreased | Markedly decreased | Tenting |
| Pulse | Normal to increased | Increased | Grossly tachycardic |
| Blood pressure | Normal | Normal | Decreased |
| Weight loss | 5% | 10% | 15% |
Hypernatremic dehydration may be accompanied by moderate clinical signs.
Reprinted with permission from RogersMC . Shock. In: RogersMC , HelfaerMA , eds. Handbook of Pediatric Intensive Care. 2nd ed. Baltimore: Williams Wilkins; 1994:140.
| Table 3. | Characteristics of the Three Stages of Parapneumonic Pleural Effusions | ||
| Exudative Stage | Fibrinolytic Stage | Organizing Stage (Empyema) | |
|---|---|---|---|
| Appearance | Nonpurulent, not turbid | Nonpurulent, not turbid | Purulent, turbid |
| Fluid consistency | Free-flowing | Loculated | Organized |
| Gram stain and culture results | Negative | Transitional | Positive (before antibiotic treatment) |
| Glucose | >100 mg/dL | <50 mg/dL | <50 mg/dL |
| Protein | <3 g/dL | >3 g/dL | >3 g/dL |
| pH | >7.30 | <7.30 | <7.30 |
| WBCs | Few | PMNs | PMNs |
PMNs, polymorphonuclear neutrophils; WBCs, white blood cells.
| Table 4. | Pleural Fluid Diagnostic Studies | |
| Study | Transudate | Exudate |
|---|---|---|
| Biochemical | ||
| Pleural LDH | <200 IU | ≥200 IU |
| Pleural fluid/serum LDH ratioa | <0.6 | ≥0.6 |
| Pleural fluid/serum protein ratioa | <0.5 | ≥0.5 |
| Specific gravity | <1.016 | ≥1.016 |
| Protein level | <3.0 g/dL | ≥3.0 g/dL |
| Other studies | ||
| Glucose | Usually >40 mg/dL | Typically <40 mg/dL |
| Amylase | May be elevated in some neoplasms, GI trauma, or surgery | |
| Rheumatoid factor, LE prep, ANA | Are occasionally helpful if collagen vascular disorders are within the differential | |
| Hematologic | ||
| WBC count | Although high counts (>100/mm3) are suggestive of an exudate, the results are quite variable. | |
| WBC differential | May actually provide more useful information | |
| Lymphocyte count | May be elevated in neoplasms, tuberculosis, and some fungal infections | |
| Segmented neutrophils | May be elevated in bacterial infections, connective tissue disease, pancreatitis, or pulmonary infarction | |
| Eosinophil count | May be elevated in bacterial infections, neoplasms, and connective tissue diseases | |
| RBC count | If >100,000/mm3, is suggestive of trauma, neoplasms, or pulmonary infarction | |
| Cytology and chromosomal studies | May show evidence of malignant cells or chromosomal abnormalities | |
| Microbiology | ||
| Gram stain | ||
| Fluid culture for aerobes and anaerobes | ||
| Acid-fast stain (if tuberculosis is in the differential) | ||
| Fungal culture | ||
| Viral culture | ||
| Counterimmune electrophoresis may aid in the detection of a bacterial infection. | ||
aThese tests are more reliable in differentiating transudate from exudate than specific gravity or protein level.
LDH, lactate dehydrogenase; LE prep, lupus erythematosus cell preparation; ANA, antinuclear antibody; WBC, white blood cell; RBC, red blood cells.
| Table 5. | Glasgow Coma Scale | ||
| Eyes open | Best motor response | ||
| Spontaneously | 4 | Obey commands | 6 |
| To speech | 3 | Localize pain | 5 |
| To pain | 2 | Withdrawal | 4 |
| None | 1 | Flexion to pain | 3 |
| Best verbal response | Extension to pain | 2 | |
| Oriented | 5 | None | 1 |
| Confused | 4 | ||
| Inappropriate | 3 | ||
| Incomprehensible | 2 | ||
| None | 1 | ||
Adapted from FleisherG , LudwigS , eds. Textbook of Pediatric Emergency Medicine. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 1993:272.
| Table 6. | Glasgow Coma Scale for Adults and Children and Modified Score for Infants | ||
| Glasgow Coma Score (Adults/Older Children) | Modified Glasgow Coma Score (Infants) | ||
|---|---|---|---|
| Eye opening | Spontaneous | 4 | Spontaneous |
| To verbal stimuli | 3 | To speech | |
| To pain | 2 | To pain | |
| None | 1 | None | |
| Best verbal response | Oriented | 5 | Coos and babbles |
| Confused speech | 4 | Irritable, cries | |
| Inappropriate words | 3 | Cries to pain | |
| Nonspecific sounds | 2 | Moans to pain | |
| None | 1 | None | |
| Best motor response | Follows commands | 6 | Normal spontaneous movements |
| Localizes pain | 5 | Withdraws to touch | |
| Withdraws to pain | 4 | Withdraws to pain | |
| Flexes to pain | 3 | Abnormal flexion | |
| Extends to pain | 2 | Abnormal extension | |
| None | 1 | None | |
| Table 7. | Key Characteristics of Vaginal Discharges | |||||
| Presenting Symptoms | Discharge | Nonmenstrual pH | Amine/Whiff Test | Vaginal Smear | Treatment | |
|---|---|---|---|---|---|---|
| Nonspecific vaginitis | Foul-smelling discharge | Scant to copious | Variable | Negative | Leukocytes | Improve perineal hygiene. |
| Itching | Brown to green in color | Bacteria and other debris | ||||
| Physiologic leukorrhea | None | Variable | <4.5 | Negative | Normal epithelial cells | None |
| Scant to moderate | Lactobacilli predominate | |||||
| Clear to white | ||||||
| Bacterial vaginosis | Foul-smelling discharge | Gray-white | >4.7 | Positive | ||
| Candidiasis | White, “curd-like” | <4.5 | Negative | Fungal hyphae and buds | ||
| Trichomonal vaginitis | 5.0–6.0 | Occasionally present | Motile flagellated organisms | Metronidazole | ||
| Foreign body | Foul-smelling discharge | Variable (usually >4.7) | Occasionally present | |||
| Contact vulvovaginitis | Variable (usually <4.5) | Negative | ||||
| Table 8. | Epidemiologic Aspects of Food Poisoning | ||
| Organism | Pathogenesis | Source | Prevention |
|---|---|---|---|
| Salmonella | Infection | Meats, poultry, eggs, dairy products | Proper cooking and food handling, pasteurization |
| Staphylococcus | Preformed enterotoxin | Meats, poultry, potato salad, cream-filled pastry, cheese, sausage | Careful food handling, rapid refrigeration |
| Clostridium perfringens | Enterotoxin | Meats, poultry | Avoid delay in serving foods; avoid cooling and rewarming foods. |
| Clostridium botulinum | Preformed neurotoxin | Honey, home-canned foods, uncooked foods | Proper refrigeration (see text) |
| Vibrio parahaemolyticus | Infection enterotoxin | Sea fish, seawater, shellfish | Proper refrigeration |
| Bacillus cereus | |||
| Diarrheal type | Sporulation enterotoxin | Many prepared foods | Proper refrigeration |
| Vomiting type | Preformed toxin | Cooked or fried rice, vegetables, meats, cereal, puddings | Proper refrigeration of cooked rice and other foods |
| Enterohemorrhagic including STEC 0157-H7 | Cytotoxins | Milk, beef | Thorough cooking of beef, consumption of pasteurized milk products |
| Enterotoxigenic Escherichia coli (traveler’s diarrhea) | Enterotoxin | Food or water | Travelers should drink only bottled or canned beverages and water, and avoid ice, raw produce including salads, and peeled fruit. Cooked foods should be eaten hot. |
| Table 9. | Clinical Aspects of Food Poisoning | ||
| Organism | Incubation | Symptoms | Duration |
|---|---|---|---|
| Bacillus cereus | Vomiting ± diarrhea; fever uncommon | 8–24 h | |
| Brucella | Several days to months; usually >30 d | Weakness, fever, headache chills, arthralgia, weight loss; splenomegaly | |
| Campylobacter | 2–10 d; usually 2–5 d | Diarrhea (often bloody), abdominal pain, fever | |
| Clostridium botulinum | 2 h to 8 d; usually 12–48 h | Poor feeding, weak cry, constipation, diplopia, blurred vision, respiratory weakness; symmetric descending paralysis | |
| Clostridium perfringens | 6–24 h | Diarrhea, abdominal cramps, vomiting and fever uncommon | <24 h |
| Escherichia coli | → | → | |
| E. coli 0157:H7 | 1–10 d; usually 3–4 d | Diarrhea (often bloody), abdominal cramps, little or no fever can cause HUS | 5–10 d |
| ETEC | 6–48 h | Diarrhea, abdominal cramps, nausea, fever, and vomiting; uncommon | 5–10 d |
| Listeria monocytogenes | 2–6 wk | Meningitis, neonatal sepsis, fever | Variable |
| Nontyphoidal Salmonella | 6–72 h | Diarrhea often with fever and abdominal cramps | <7 d |
| Salmonella typhi | 3–60 d; usually 7–14 d | Fever, anorexia, malaise, headache, myalgias ± diarrhea or constipation | 3–4 wk |
| Shigella | 12 h to 6 d; usually 2–4 d | Diarrhea (often bloody), frequently fever, abdominal cramps | 1 d to 1 mo |
| Staphylococcus aureus | 30 min to 8 h; usually 2–4 h | Vomiting, diarrhea | <24 h |
| Vibrio | 4–30 h | Diarrhea, cramps, nausea, vomiting | Self-limited |
| Yersinia enterocolitica | 1–10 d; usually 4–6 d | Diarrhea, abdominal pain (often severe), mesenteric adenitis, pseudoappendicular syndrome | 1–3 wk |
ETEC, enterotoxigenic Escherichia coli; HUS, hemolytic uremic syndrome.
| Table 10. | U.S. Food and Drug Administration Pharmaceutical Pregnancy Categories |
| Pregnancy Category A | Adequate and well-controlled human studies have failed to demonstrate a risk to the fetus in the first trimester of pregnancy (and there is no evidence of risk in later trimesters). |
| Pregnancy Category B | Animal reproduction studies have failed to demonstrate a risk to the fetus, and there are no adequate and well-controlled studies in pregnant women OR animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in any trimester. |
| Pregnancy Category C | Animal reproduction studies have shown an adverse effect on the fetus, and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. |
| Pregnancy Category D | There is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. |
| Pregnancy Category X | Studies in animals or humans have demonstrated fetal abnormalities and/or there is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience, and the risks involved in use of the drug in pregnant women clearly outweigh potential benefits. |
| Table 11. | Assessment of Etiology of Rickets Based on Laboratory Results | |||||||
| Ca | Phos | Alk phos | iPTH | 25-(OH)D | 1,25-(OH)2D | Urine Ca/Cr | TRP | |
|---|---|---|---|---|---|---|---|---|
| Nutritional/insufficient sunlight | N or ↓ | ↓ | ↑ | ↑ | ↓ | ↑ | ↓ | ↑ |
| Malabsorption | N or ↓ | ↓ | ↑ | ↑ | ↓ | ↑ | ↓ | ↑ |
| Renal tubular defects | N or ↓ | ↓ | ↑ | ↑ | N | ↑ | ↑ | N or ↓ |
| Altered vitamin D metabolism | N or ↓ | ↓ | ↑ | ↑ | ↓ | ↑ | ↓ | ↑ |
| Genetic forms of rickets | ||||||||
| X-linked, AD, and AR hypophosphatemic rickets | N | ↓ | ↑ | N or ↑ | N | N or ↑ | N or ↓ | ↓ |
| 1a-hydroxylase deficiency | ↓ | ↓ | ↑ | ↑ | N | ↓ | ↓ | ↑ |
| Vitamin D receptor mutations (vitamin D resistance) | ↓ | ↓ | ↑ | ↑ | N | ↑ | ↓ | ↑ |
| Hereditary hypophosphatemic rickets with hypercalciuria | N or ↓ | ↓ | ↑ | ↑ | N | ↑ | ↑ | ↓ |
| Hypophosphatasia | N or ↑ | N or ↑ | ↓ | N or ↓ | N | N or ↓ | N or ↑ | N |
Ca, calcium; phos, phosphorus; alk phos, alkaline phosphatase; iPTH, intact parathyroid hormone; 25-(OH)-D, 25-hydroxy vitamin D; 1,25-(OH)2-D, 1,25-dihydroxy vitamin D; Ca/Cr, calcium/creatinine ratio; TRP, tubular reabsorption of phosphorus ([1 − (U phos × P Cr/U Cr × S Phos)] × 100, normal 85–95%); AD, autosomal dominant; AR, autosomal recessive; N, normal.
| Table 12. | Dietary Reference Intake for Calcium and Vitamin D | |||||
| Calcium | Vitamin D | |||||
|---|---|---|---|---|---|---|
| Age | Estimated Average Requirement (mg/d) | Recommended Dietary Allowance (mg/d) | Upper Level Intake (mg/d) | Estimated Average Requirement (IU/d) | Recommended Dietary Allowance (IU/d) | Upper Level Intake (IU/d) |
| 0–6 mo | 200 | 200 | 1,000 | 400 | 400 | 1,000 |
| 6–12 mo | 260 | 260 | 1,500 | 400 | 400 | 1,500 |
| 1–3 y | 500 | 700 | 2,500 | 400 | 600 | 2,500 |
| 4–8 y | 800 | 1,000 | 2,500 | 400 | 600 | 3,000 |
| 9–18 y | 1,100 | 1,300 | 3,000 | 400 | 600 | 4,000 |
| 19–30 y | 800 | 1,000 | 2,500 | 400 | 600 | 4,000 |
Adapted from RossAC , AbramsSA , AloiaJF , et al. Dietary reference intakes for calcium and vitamin D . http://www.iom.edu/~/media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20Calcium%202010%20Report%20Brief.pdf. Accessed March 1, 2015.
| Table 13. | Clinical and Biochemical Features of Congenital Adrenal Hyperplasia | |||
| Sexual Ambiguity | Additional Clinical Manifestations | Predominant Steroids | ||
|---|---|---|---|---|
| Enzyme Defect | Female | Male | ||
| Desmolase | − | + | Salt wasting | — |
| 3β-hydroxysteroid dehydrogenase | + | + | Salt wasting | 17-OH-pregnenolone, DHEA |
| 21-hydroxylase | + | − | Salt wasting | 17-OH-progestone, androstenedione |
| 11-hydroxylase | + | − | Hypertension | 11-deoxycortisol |
| 17-hydroxylase | − | + | Hypertension | DOC, corticosterone |
Figure 4. Nomogram for estimating severity of acute poisoning.
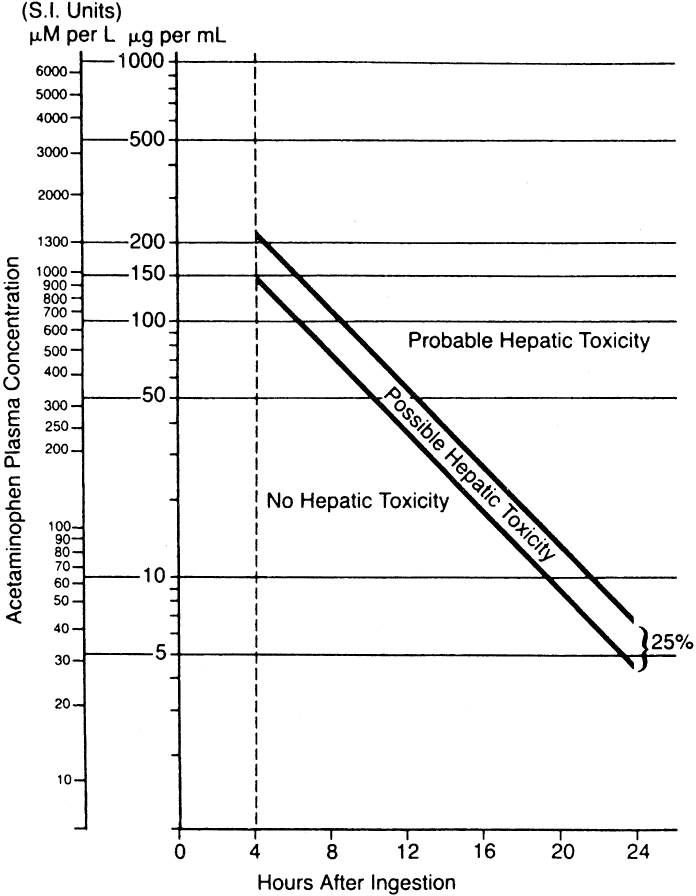 Figure 4.
Figure 4.(Reprinted with permission from RumackBH , MatthewH . Acetaminophen poisoning and toxicity . Pediatrics. 1975;55(6):871–876.)
Figure 5. National Heart, Lung, and Blood Institute, National Institutes of Health.
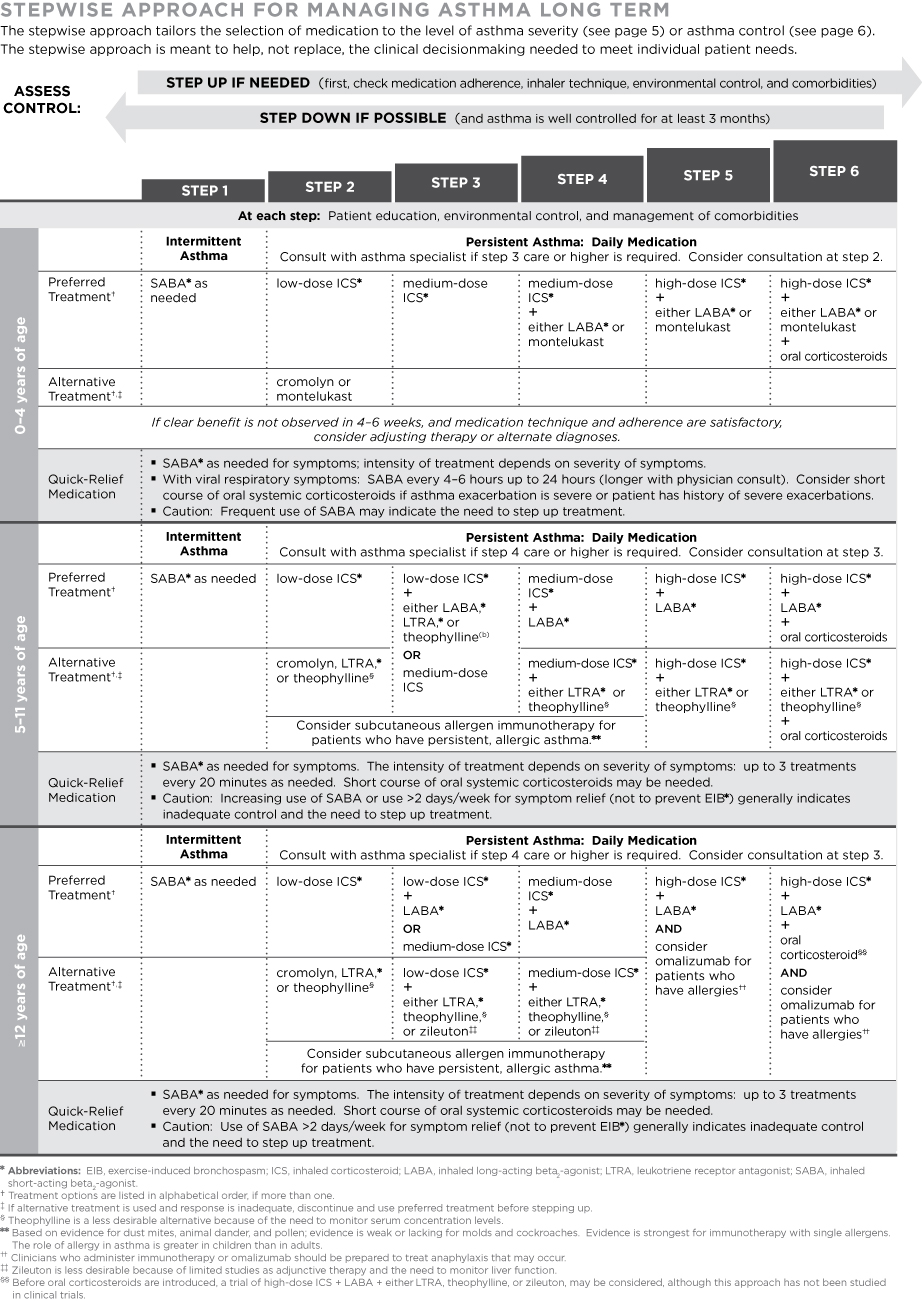 Figure 5.
Figure 5.Asthma care quick reference : http://www.nhlbi.nih.gov/files/docs/guidelines/asthma_qrg.pdf. Accessed March 1, 2015.
| Table 14. | Estimated Comparative Daily Dosages: Inhaled Corticosteroids for Long-Term Asthma Control | ||||||||
| 0–4 years of age | 5–11 years of age | ≤12 years of age | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Daily Dose | Low | Meduim* | High* | Low | Meduim* | High* | Low | Meduim* | High* |
| MEDICATION | |||||||||
| Beclomethasone MDI† | N/A | N/A | N/A | 80–160 mcg | >160–320 mcg | >320 mcg | 80–240 mcg | >240–480 mcg | >480 mcg |
| 40 mcg/puff | 1–2 puffs 2×/day | 3–4 puffs 2×/day | 1–3 puffs 2×/day | 4–6 puffs 2×/day | |||||
| 80 mcg/puff | 1 puff 2×/day | 2 puffs 2×/day | ≥3 puffs 2×/day | 1 puff am, 2 puffs pm | 2–3 puffs 2×/day | ≥4 puffs 2×/day | |||
| Budesonide DPI† | N/A | N/A | N/A | 180–360 mcg | >360–720 mcg | >720 mcg | 180–540 mcg | >540–1,080 mcg | >1,080 mcg |
| 90 mcg/inhalation | 1–2 inhs† 2×/day | 3–4 inhs† 2×/day | 1–3 inhs† 2×/day | ||||||
| 180 mcg/inhalation | 2 inhs† 2×/day | ≥3 inhs† 2×/day | 1 inh† am, 2 inhs† pm | 2–3 inhs† 2×/day | ≥4 inhs† 2×/day | ||||
| Budesonide Nebules | 0.25–0.5 mg | >0.5–1.0 mg | >1.0 mg | 0.5 mg | 1.0 mg | 2.0 mg | N/A | N/A | N/A |
| 0.25 mg | 1–2 nebs†/day | 1 neb† 2×/day | |||||||
| 0.25 mg | 1 neb†/day | 2 nebs†/day | 3 nebs†/day | 1 neb†/day | 1 neb† 2×/day | ||||
| 1.0 mg | 1 neb†/day | 2 nebs†/day | 1 neb†/day | 1 neb†2×/day | |||||
| Ciclesonide MDI† | N/A | N/A | N/A | 80–160 mcg | >160–320 mcg | >320 mcg | 160–320 mcg | >320–640 mcg | >640 mcg |
| 80 mcg/puff | 1–2 puffs/day | 1 puff am, 2 puffs pm–2 puffs 2×/day | ≥3 puffs 23/day | 1–2 puffs 2×/day | 3–4 puffs 2×/day | ||||
| 160 mcg/puff | 1 puff/day | 1 puff 2×/day | ≥2 puffs 2×/day | 2 puffs 2×/day | ≥3 puffs 2×/day | ||||
| Flunisolide MDI† | N/A | N/A | N/A | 160 mcg | 320–480 mcg | ≥480 mcg | 320 mcg | >320–640 mcg | >640 mcg |
| 80 mcg/puff | 1 puff 2×/day | 2–3 puffs 2×/day | ≥4 puffs 2×/day | 2 puffs 2×/day | 3–4 puffs 2×/day | ≥5 puffs 2×/day | |||
| Fluticasone MDI† | 176 mcg | >176–352 mcg | >352 mcg | 88–176 mcg | >176–352 mcg | >352 mcg | 88–264 mcg | >264–440 mcg | >440 mcg |
| 44 mcg/puff | 2 puffs 2×/day | 3–4 puffs 2×/day | 1–2 puffs 2×/day | 3–4 puffs 2×/day | 1–3 puffs 2×/day | ||||
| 110 mcg/puff | 1 puff 2×/day | ≥2 puffs 2×/day | 1 puff 2×/day | ≥2 puffs 2×/day | 2 puffs 2×/day | 3 puffs 2×/day | |||
| 220 mcg/puff | 1 puff 2×/day | ≥2 puffs 2×/day | |||||||
| Fluticasone DPI† | N/A | N/A | N/A | 100–200 mcg | >200–400 mcg | >400 mcg | 100–300 mcg | >300–500 mcg | >500 mcg |
| 50 mcg/inhalation | 1–2 inhs† 2×/day | 3–4 inhs† 2×/day | 1–3 inhs† 2×/day | ||||||
| 100 mcg/inhalation | 1 inh† 2×/day | 2 inhs† 2×/day | >2 inhs† 2×/day | 2 inhs† 2×/day | ≥3 inhs† 2×/day | ||||
| 250 mcg/inhalation | 1 inh† 2×/day | 1 inh† 2×/day | ≥2 inhs† 2×/day | ||||||
| Mometasone DPI† | N/A | N/A | N/A | 110 mcg | 220–440 mcg | >440 mcg | 110–220 mcg | >220–440 mcg | >440 mcg |
| 110 mcg/inhalation | 1 inh†/day | 1–2 inhs† 2×/day | ≥3 inhs† 2×/day | 1–2 inhs† pm | 3–4 inhs† pm or2 inhs† 2×/day | ≥3 inhs† 2×/day | |||
| 220 mcg/inhalation | 1–2 inhs†/day | ≥3 inhs† dividedin 2 doses | 1 inh† pm | 1 inh† 2×/day or2 inhs† pm | ≥3 inhs† dividedin 2 doses | ||||
*It is preferable to use a higher mcg/puff or mcg/inhalation formulation to achive as low a number of puffs or inhalations as possible.
†Abbreviations: DPI, dry power inhaler (requires deep, fast inhalation); inh, inhalation; MDI, metered dose inhaler (releases a puff of medication); neb, nebule.
National Heart, Lung, and Blood Institute, National Institutes of Health. Asthma care quick reference : http://www.nhlbi.nih.gov/files/docs/guidelines/asthma_qrg.pdf. Accessed March 1, 2015.
| Table 15. | Relative Potencies of Topical Corticosteroids | ||
| Class | Drug | Dosage form(s) | Strength (%) |
|---|---|---|---|
| I. Very high potency | Augmented betamethasone dipropionate | Ointment | 0.05 |
| Clobetasol propionate | Cream, foam, ointment | 0.05 | |
| Diflorasone diacetate | Ointment | 0.05 | |
| Halobetasol propionate | Cream, ointment | 0.05 | |
| II. High potency | Amcinonide | Cream, lotion, ointment | 0.1 |
| Augmented betamethasone dipropionate | Cream | 0.05 | |
| Betamethasone dipropionate | Cream, foam, ointment, solution | 0.05 | |
| Desoximetasone | Cream, ointment | 0.25 | |
| Desoximetasone | Gel | 0.05 | |
| Diflorasone diacetate | Cream | 0.05 | |
| Fluocinonide | Cream, gel, ointment, solution | 0.05 | |
| Halcinonide | Cream, ointment | 0.1 | |
| Mometasone furoate | Ointment | 0.1 | |
| Triamcinolone acetonide | Cream, ointment | 0.5 | |
| III–IV. Medium potency | Betamethasone valerate | Cream, foam, lotion, ointment | 0.1 |
| Clocortolone pivalate | Cream | 0.1 | |
| Desoximetasone | Cream | 0.05 | |
| Fluocinolone acetonide | Cream, ointment | 0.025 | |
| Flurandrenolide | Cream, ointment | 0.05 | |
| Fluticasone propionate | Cream | 0.05 | |
| Fluticasone propionate | Ointment | 0.005 | |
| Mometasone furoate | Cream | 0.1 | |
| Triamcinolone acetonide | Cream, ointment | 0.1 | |
| V. Lower-medium potency | Hydrocortisone butyrate | Cream, ointment, solution | 0.1 |
| Hydrocortisone probutate | Cream | 0.1 | |
| Hydrocortisone valerate | Cream, ointment | 0.2 | |
| Prednicarbate | Cream | 0.1 | |
| VI. Low potency | Alclometasone dipropionate | Cream, ointment | 0.05 |
| Desonide | Cream, gel, foam, ointment | 0.05 | |
| Fluocinolone acetonide | Cream, solution | 0.01 | |
| VII. Lowest potency | Dexamethasone | Cream | 0.1 |
| Hydrocortisone | Cream, lotion, ointment, solution | 0.25, 0.5, 1 | |
| Hydrocortisone acetate | Cream, ointment | 0.5–1 | |
From PallerAS , ManciniAJ . Eczematous eruptions in childhood. In: PallerAS , ManciniAJ , eds. Hurwitz Clinical Pediatric Dermatology: A Textbook of Skin Disorders of Childhood and Adolescence. 4th ed. St. Louis, MO: Elsevier; 2011: 49, with permission from Elsevier.
Outline
