![]()
In this chapter, you’ll learn:
The historical roots of nursing and its emergence as a profession
Practice guidelines and the educational background required for nursing
Functions and roles of nurses in various care settings
The guiding principles behind nursing theories and patient care.
As we progress through the 21st century, the role of the nurse continues to expand. The increasing reliance on technology in nursing education and practice, the pressures of health care reform, and the continuing crisis of noninsured or underinsured persons have combined to make nursing practice more complex than ever.
The nursing profession has developed a reputation for successfully delivering high-quality, cost-effective care. In fact, a survey of public attitudes toward health care and nurses conducted in the United States revealed that the public admires nurses and that most people are willing to have an increasing portion of their care delivered by registered nurses.

Nursing’s origins lie in religious and military traditions that demanded unquestioning obedience to authority. Florence Nightingale challenged these traditions by emphasizing critical thinking, attention to patients’ individual needs, and respect for patients’ rights.
Nightingale proposed that schools of nursing be independent of hospitals and that they provide nursing education but not patient care. She demanded that her schools accept only qualified candidates and that the students learn to teach as well as provide care.
The first schools of nursing based on Nightingale’s model opened in the United States in 1873 and in Canada in 1874. Her ideas were soon discarded, however, when nursing schools realized that they couldn’t survive without the hospitals’ financial support. At the same time, hospitals recognized that nursing students were a major source of cheap, disciplined labor. They began to hire student nurses instead of more experienced—and more expensive—graduate nurses.
This situation changed after World War II, when major scientific discoveries and technological advancements altered the nature of hospital care. Increasingly, the care of hospitalized patients required experienced, skilled nurses. The development of intensive and coronary care units gave rise to the concept of the advanced clinician: a nurse qualified to give specialized care and the forerunner of today’s clinical nurse specialist.
After the war, nursing responded to greater public interest in health promotion and disease prevention by creating another new role: the nurse practitioner. Using advanced knowledge and skills, the nurse practitioner helps promote health and helps prevent illness while caring for the minor health concerns of patients.
Another crucial change in nursing stemmed from a midcentury shift in attitudes about education for women. The practice of extending full educational opportunities to women has significantly altered the role that nurses play in today’s health care system. Armed with a strong educational base, nurses have the confidence necessary to question, analyze, and argue for family-centered health care—and to secure a major role for nursing in delivering that care.

Florence Nightingale believed that a nurse’s goal should be “to put the patient in the best condition for nature to act upon him.” Definitions of nursing have changed over time, but nursing has retained a common focus: providing humanistic and holistic care to each patient.
The American Nurses Association’s (ANA) definition of nursing shares this focus: “The practice of nursing by a registered nurse is defined as the process of diagnosing human responses to actual or potential health problems; providing supportive and restorative care, health counseling and teaching, case finding and referral; collaborating the implementation of the total health care regimen; and executing the medical regimen under the direction of a licensed physician or dentist.”
Most people use the term “nursing professionals” to describe a group of people who practice nursing. However, not everyone agrees that nursing has the full autonomy that it needs to distinguish itself as a profession rather than an occupation.

Nursing already has achieved some degree of autonomy. It exercises control over its education and practice. It has achieved legal recognition through licensure. Every state and Canadian province now has a nurse practice act, which requires nurses to pass state board examinations in order to practice and regulates the scope of their practice. Nursing also has a code of ethics, which is regularly updated to reflect current ethical issues.
The key to professional nursing autonomy, however, is to function independently of any other profession or external force. For many nurses, this remains a goal to be achieved. As employees of large, sometimes inflexible organizations, nurses seldom enjoy full latitude in deciding on patient care within the defined scope of nursing practice. However, by striving for individual excellence, each nurse can help this emerging profession become a full-fledged profession.
The ANA has identified two categories of nursing practice—professional and associate—and established educational requirements for each. According to the ANA’s guidelines, the minimum requirement for beginning professional nurses is a baccalaureate degree in nursing (BSN), whereas the minimum requirement for beginning associate nurses is an associate’s degree in nursing (ADN).
Besides pursuing a BSN at a 4-year college or university or an ADN at a junior or community college, today’s undergraduate student nurses have a third option: hospital-operated diploma programs. However, regardless of which option she chooses, a graduate of any of these three programs is eligible to sit for the same registered nurse (RN) licensing examination.
After the nurse receives her baccalaureate degree, she may choose to advance her education at the graduate level. She can choose from a number of graduate fields, including nursing. She can choose a Master of Arts (MA) in nursing, Master in Nursing (MN), or Master of Science in Nursing (MSN). A master’s degree qualifies a nurse to serve as a nurse educator, clinical nurse specialist, nursing administrator, or nurse practitioner.
Doctoral education in nursing is expanding. Most doctoral programs in nursing lead to a Doctor of Philosophy (PhD) degree or a doctorate in nursing practice (DNP).
A nurse with a doctorate might assume a leadership position in a practice setting or as an educator of beginning nurses and those seeking advanced clinical and educational preparation, including research in nursing.
The way you practice your profession of nursing should be guided by two sets of care documents: standards of nursing care and nurse practice acts. The standards of nursing care are administered by the ANA, and the nurse practice acts are administered by individual states or provinces.
Standards of care set minimum criteria for your proficiency on the job, enabling you and others to judge the quality of care you and your nursing colleagues provide. They help to ensure high-quality care and, in the legal arena, they serve as criteria to help determine whether adequate care was provided to a patient. States may refer to standards in their nurse practice acts. Unless included in a nurse practice act, professional standards aren’t laws; they’re guidelines for sound nursing practice.
Some nurses regard standards of nursing care as pie-in-the-sky ideals that have little bearing on the reality of working life. This opinion is a dangerous misconception. You’re expected to meet standards of nursing care for every nursing task you perform.

The ANA standards include two lists:
Standards of professional performance, which include guidelines for quality of care, performance appraisal, education, collegiality, ethics, collaboration, research, resource utilization, and leadership
Standards of practice, which outline professional responsibilities in assessment, diagnosis, outcome identification, planning, implementation, and evaluation.
The standards below are adapted from standards of nursing practice published by the American Nurses Association (ANA). The ANA developed the standards (last revised in 2010) to provide registered nurses with guidelines for determining quality nursing care. The courts as well as hospitals, nurses, and patients may refer to these standards. The standards of nursing practice are divided into the standards of practice, which define care provided to patients, and the standards of professional performance, which explain the level of behavior expected of the nurse in a professional role.
Each standard below is followed by measurement criteria that give key indicators of competent practice for that standard. This adaptation of the standards doesn’t present the standards that are specific only to advanced practice nurses.
| Standards of Practice |
| Standard 1: Assessment |
| The nurse collects patient health data. Measurement criteria
|
| Standard 2: Diagnosis |
| The nurse analyzes the assessment data in determining the diagnosis. Measurement criteria
|
| Standard 3: Outcomes identification |
| The nurse identifies expected outcomes individualized to the patient. Measurement criteria
|
| Standard 4: Planning |
| The nurse develops a care plan that prescribes interventions to attain expected outcomes. Measurement criteria
|
| Standard 5: Implementation |
| The nurse implements the plan. Measurement criteria
|
| Standard 5a: Coordination of care |
| The nurse coordinates care delivery. Measurement criteria
|
| Standard 5b: Health teaching and health promotion |
| The nurse promotes health and a safe environment. Measurement criteria
|
| Standard 6: Evaluation |
| The nurse evaluates the patient’s progress toward attaining outcomes. Measurement criteria
|
| Standards of Professional Performance |
| Standard 7: Ethics |
| The nurse integrates ethics in all areas of practice. Measurement criteria
|
| Standard 8: Education |
| The nurse acquires current knowledge and competency in nursing practice. Measurement criteria
|
| Standard 9: Evidence-Based Practice and Research |
| The nurse uses research findings in practice. Measurement criteria
|
| Standard 10: Quality of practice |
| The nurse systematically enhances the quality and effectiveness of nursing practice. Measurement criteria
|
| Standard 11: Communication |
| The nurse communicates effectively in all areas of practice. Measurement criteria
|
| Standard 12: Leadership |
| The nurse shows leadership in the practice setting and in the profession. Measurement criteria
|
| Standard 13: Collaboration |
| The nurse collaborates with the patient, family, and others in providing patient care. Measurement criteria
|
| Standard 14: Professional practice evaluation |
| The nurse evaluates her own nursing practice in relation to professional practice standards and relevant statutes and regulations. Measurement criteria
|
| Standard 15: Resource utilization |
| The nurse considers factors related to safety, effectiveness, cost, and impact in planning and delivering patient care. Measurement criteria
|
| Standard 16: Environmental Health |
| The nurse practices in an environmentally safe and healthy manner. Measurement Criteria
|
The nurse practice act of each state defines the practice of nursing for that state. Nurse practice acts are broadly worded, and the wording varies from state to state. Understanding your nurse practice act’s general provisions will help you stay within the legal limits of nursing practice. With the emergence of more autonomous and expanded roles for nurses, many states have started to revise their nurse practice acts to reflect the greater responsibilities associated with current nursing practice.
Interpreting your nurse practice act isn’t always easy. One problem stems from the fact that nurse practice acts are statutory laws. So, any amendment to a nurse practice act must be accomplished by means of the inevitably slow legislative process. Because of the time involved in pondering, drafting, and enacting laws, amendments to the nurse practice acts lag well behind the changes in nursing.
You may be asked to perform tasks that seem to be within the accepted scope of nursing but in fact violate your state’s nurse practice act. Your state’s nurse practice act isn’t a word-for-word checklist on how you should do your work. You must rely on your own education and knowledge of your facility’s policies and procedures.

Make sure you’re familiar with the legally permissible scope of your nurse practice act, as defined in your state’s nurse practice act and board of nursing rules and regulations. Otherwise, you’re inviting legal trouble.
All nurses must be licensed in the state in which they practice. The National Council Licensure Examination (NCLEX) must be taken and passed by all RN candidates. The test is exactly the same in all states.
The practicing nurse may choose to be certified in a specialty area in which she works. Each certification has minimum requirements, such as education and current work experience. After the nurse has met these requirements and passed an examination, she maintains the certification by continuing education and clinical or administrative practice.
| It’s all in the certification This list includes some of the nursing specialty certifications and their appropriate credentials. Addictions nursing
Advanced practice nursing
Childbirth educators
Critical care nursing
Diabetes educators
Emergency nursing
Flight nursing
Gastroenterology nursing
Genetic nursing
Health care quality nursing
HIV-AIDS nursing
Holistic nursing
Hospice and palliative nursing
Infection control nursing
Infusion nursing
Lactation consultant
Legal nurse consulting
Managed care nursing
Maternal-neonatal nursing
Medical-surgical nursing
Nephrology nursing
Neuroscience nursing
Nurse administration: Long-term care
Nurse anesthetist
Nurse midwifery and midwifery
Nutrition support nursing
Occupational health nursing
Oncology nursing
Ophthalmic nursing
Orthopedic nursing
Pediatric nursing
Pediatric oncology nursing
Perianesthesia nursing
Perioperative nursing
Rehabilitation nursing
School nursing
Urology nursing
|
Professional organizations are an important part of your nursing profession. They provide current information and resource material and allow you a voice in your profession.
| Individual state nurses associations Contacting your state nurses association is only a click away. Can you find the Web site for your state’s association in this list?
|
Nursing organizations include the ANA, the National League for Nursing, the International Council of Nurses, and the National Student Nurses Association. Nurse specialty groups include the Association of Critical Care Nurses, Sigma Theta Tau, the American Association of Nurse Anesthetists, and the Academy of Medical Surgical Nursing, to name just a few.
In addition, each state has its own nursing association that’s a division of the ANA.
Recent changes in health care reflect changes in the population that require nursing care and a philosophical shift toward health promotion rather than treatment of illness. The role of the nurse has broadened in response to these changes. Nurses are caregivers, as always, but now they’re also educators, advocates, leaders and managers, charge agents, and researchers.
Nurses have always been caregivers, but the activities this role encompasses changed dramatically in the 20th century. Increased education of nurses expanded nursing research, and the consequent recognition that nurses are autonomous and informed professionals have caused a shift from a dependent role for the nurse to one of independence and collaboration.
Unlike earlier models, medical-surgical nurses now conduct independent assessments and implement patient care based on their knowledge and skills. They also collaborate with other members of the health care team to implement and evaluate that care.

With greater emphasis on health promotion and illness prevention, the nurse’s role as educator has become increasingly important. The nurse assesses learning needs, plans and implements teaching strategies to meet those needs, and evaluates the effectiveness of the teaching. To be an effective educator, the nurse must have effective interpersonal skills and be familiar with principles of adult learning.
Patient teaching is also a major part of discharge planning. Along with teaching come responsibilities for making referrals, identifying community and personal resources, and arranging for necessary equipment and supplies for home care.
As an advocate, the nurse helps the patient and his family members interpret information from other health care providers and make decisions about his health-related needs. The nurse must accept and respect a patient’s decision, even if it differs from the decision the nurse would make.
All nurses practice leadership and manage time, people, resources, and the environment in which they provide care. They carry out these tasks by directing, delegating, and coordinating activities.
All health care team members, including the nurse, provide patient care. Although the doctor is usually considered the head of the team, the nurse plays an important role in coordinating the efforts of all team members to meet the patient’s goals and may conduct team conferences to facilitate communication among team members.

As a change agent, the nurse works with the patient to address his health concerns and with staff members to address organizational and community concerns. This role demands knowledge of change theory, which provides a framework for understanding the dynamics of change, human responses to change, and strategies for effecting change.
In the community, nurses serve as role models and assist people in bringing about changes to improve the environment, work conditions, or other factors that affect health. Nurses also work together to bring about change through legislation by helping to shape and support the laws that mandate the use of car safety seats and motorcycle helmets.
As a discharge planner, the nurse assesses the patient’s needs at discharge, including the patient’s support systems and living situation. The nurse also links the patient with available community resources.
The primary tasks of nursing research are to promote growth in the science of nursing and to develop a scientific basis for nursing practice. Every nurse should be involved in nursing research and apply research findings to her nursing practice.

Although not all nurses are trained in research methods, each nurse can participate by remaining alert for nursing problems and asking questions about care practices. Many nurses who give direct care identify such problems, which then serve as a basis for research. Nurses can improve nursing care by incorporating research findings into their practice and communicating the research to others.
In today’s nursing profession, nurses have a broad area of opportunity. They may be staff nurses, nurse educators, nurse managers, case managers, clinical nurse specialists, nurse practitioners, and nurse researchers.
The staff nurse functions as a primary caregiver by independently making assessments, planning and implementing patient care, and providing direct nursing care. For example, a staff nurse may make clinical observations and execute interventions, such as administering medications and treatments and promoting such activities of daily living as bathing and toileting.
As the emphasis on health promotion and illness prevention has increased, the nurse’s role as educator has become increasingly important. The nurse educator’s students include patients and family members as well as other health professionals.
The nurse assesses patients’ and family members’ learning needs, plans and implements teaching strategies to meet those needs, and evaluates the effectiveness of the teaching.
To be an effective educator, the nurse must have excellent interpersonal skills and be familiar with the appropriate developmental stages of children, adolescents, and adults as well as the principles of learning for each age-group.
The nurse manager acts as a staff nurse and an administrative representative of the unit, ensuring that effective and quality nursing care is being provided in a timely and fiscally managed environment.
To counter the trend toward fragmented, depersonalized nursing care, hospitals have developed the role of case manager. This role enables the nurse to manage comprehensive care of an individual patient.

Case management is a systematic approach to delivering total patient care within specified time frames and economic resources. Case management encompasses the patient’s entire illness episode, crosses all care settings, and involves the collaboration of all personnel who care for the patient.
The case manager is also involved in planning for discharge, making referrals, identifying community and personal resources, and arranging for equipment and supplies needed by the patient on discharge.
The clinical nurse specialist has obtained an MSN and acquired expertise in a clinical specialty, such as critical care, emergency care, or maternal-neonatal care. The clinical nurse specialist provides evidence-based nursing care by participating in education and direct patient care, consulting the patient and family members, and collaborating with other nurses and health care team members to deliver high-quality patient care.
A nurse practitioner has also obtained an MSN and specializes in a clinical area such as critical care. The nurse practitioner provides primary health care to patients and families and can function independently. The nurse practitioner may obtain histories and conduct physical examinations, order laboratory and diagnostic tests and interpret results, diagnose disorders, treat patients, counsel and educate patients and family members, and provide continual follow-up care after patients are discharged from the critical care unit.

The nurse researcher promotes the science of nursing by investigating problems related to nursing. The goal is to develop and refine nursing knowledge and practice. Staff nurses participate in nursing research by reading current nursing literature, applying the information in practice, and then collecting data. Advanced practice nurses (clinical nurse specialists and nurse practitioners) can assist staff nurses by conducting the research study and serving as a consultant to the nurses during implementation of a research study.
Many nursing leaders believe that the profession must establish itself as a scientific discipline to enhance its reputation. To do that, nursing needs a theoretical base that simultaneously shapes and reflects its practice.
Four themes guide the development of nursing theory:
 Principles and laws that govern life processes, well-being, and the optimal functioning of people—sick or well
Principles and laws that govern life processes, well-being, and the optimal functioning of people—sick or well Patterns of human behavior that describe how people interact with the environment in critical life situations
Patterns of human behavior that describe how people interact with the environment in critical life situations Processes for bringing about positive changes in the health status of individuals
Processes for bringing about positive changes in the health status of individuals Nursing’s key role as the central focus of all nursing theories.
Nursing’s key role as the central focus of all nursing theories.
A holistic way of organizing nursing information is by using functional health patterns—patterns that outline human needs. These patterns, described by Marjory Gordon, focus on behaviors that occur over time and present a total picture of the patient. The patterns represent the patient’s basic health needs and are unique and interrelated.
| Gordon’s functional health patterns These health patterns represent broad categories within the wellness–illness continuum. The categories focus on a person’s functional abilities.
|
Theorists and researchers are now collaborating with practicing nurses in the development, testing, and refining of nursing theory.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Many theories not specifically developed for nursing have been adopted by the nursing profession to provide guidelines for practicing excellent patient care.
In systems theory, a system can be an individual, a family, or a community. System theories are the basis for holistic nursing when the patient is viewed not as a whole but as many parts that are interrelated.

In general, system theories include a purpose (or goal), content (the information obtained from the system), and a process used to achieve the goal. The whole (be it an individual, family, or community) is broken down, and all of the parts are examined. System theories integrate each part of the whole and examine how each part affects the whole.
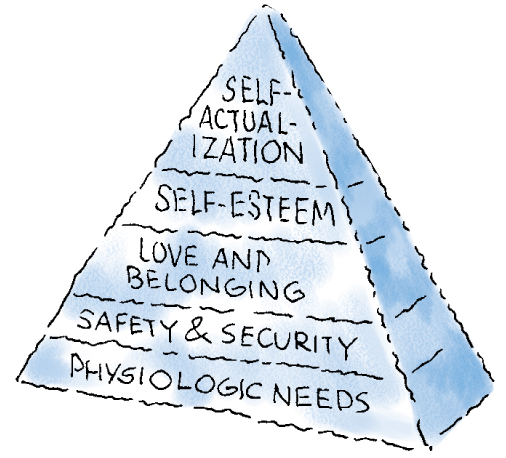
Human needs are the physiologic or psychological factors that must be met for an individual to have a healthy existence. These are basic needs that were categorized by Maslow according to importance. Lower level physiologic needs, such as the need for oxygen, food, elimination, temperature control, sex, rest, and comfort, must be met before higher level needs, such as a sense of self-worth and self-respect, can be met. These theories are useful when applying nursing diagnoses.
| Maslow’s hierarchy of needs To formulate nursing diagnoses, you must know your patient’s needs and values. Of course, physiologic needs—represented by the base of the pyramid in the diagram below—must be met first.
|
Developmental theories classify an individual’s behavior or tasks according to their age or development. These theories use categories to describe characteristics associated with the majority of individuals at periods when distinctive developmental changes occur. However, they don’t take into account individual differences. These types of theories focus on only one type of development, such as cognitive, psychosocial, psychosexual, and moral or faith development. Even so, developmental theories do allow the nurse to describe typical behavior within a certain age-group, which can be helpful during patient teaching and counseling.

Research is the foundation on which all sciences are based. Its reliance on observations made in a controlled setting limits confusion over which factors actually produce the results. Health care professionals have long recognized the importance of research in the laboratory setting but recently have begun to develop ways to make research information more useful in the clinical setting.
The goal of research is to improve the delivery of care and, thereby, improve patient outcomes. Nursing care is commonly based on evidence that’s derived from research. Evidence can be used to support current practices or to change practices.
Research and nursingAll scientific research is based on the same basic process.
| Research steps The research process consists of these steps:
|
The best way to get involved in research is to be a good consumer of nursing research. You can do so by reading nursing journals and being aware of the quality of research and reported results.
Don’t be afraid to share research findings with colleagues. Sharing promotes sound clinical care, and all involved may learn about easier and more efficient ways to care for patients.

One of the newest ways to make research results more useful in clinical practice is by delivering evidence-based care. Evidence-based care isn’t based on traditions, customs, or intuition. It’s derived from various concrete sources, including:
Formal nursing research
Clinical knowledge
Scientific knowledge.
Research results may provide insight into the treatment of a patient who, for example, doesn’t respond to a medication or treatment that seems effective for other patients.
In this example, you may believe that a certain drug should be effective for pain relief based on previous experience with that drug. The trouble with such an approach is that other factors can contribute to pain relief, such as the route of administration, the dosage, and concurrent treatments.

Regardless of the value of evidence-based care, you should always use professional clinical judgment when dealing with critically ill patients and their families. Remember that each patient’s condition ultimately dictates treatment.
References
Association of Colleges of Nursing. (n.d.). Your guide to graduate nursing programs. Retrieved from http://www.aacn.nche.edu/publications/GradStudentsBrochure.pdf
Nurses Association. (2010). Nursing: Scope and standards of practice (2nd ed.). Silver Springs, MD: Nursesbook.org.
![]()
- The way you practice your profession of nursing should be guided by standards of nursing care and which of the following?
- The standards of nursing care are administered by the:
- Nurse practice acts are administered by your:
- A nurse who can obtain histories, conduct physical examinations, order laboratory and diagnostic tests, interpret results, diagnose disorders, and treat patients has what nursing credentials?
- The easiest way to participate in research is to:
- The purpose of evidence-based practice is to:
 If you answered all six questions correctly, fantastic! You’re building a good nursing foundation.
If you answered all six questions correctly, fantastic! You’re building a good nursing foundation. If you answered four or five questions correctly, super! Your foundation is getting strong.
If you answered four or five questions correctly, super! Your foundation is getting strong. If you answered fewer than four questions correctly, don’t worry! With a little review, your foundation will be strong before you know it.
If you answered fewer than four questions correctly, don’t worry! With a little review, your foundation will be strong before you know it.Outline