![]()
In this chapter, you’ll learn:
Basics of medication administration
Drug administration routes
Key concepts of pharmacokinetics and pharmacodynamics
Dosage and administration considerations
Various drug delivery systems
Common medication errors.
When you care for a patient in your day-to-day nursing practice, one of the most crucial skills you bring to the bedside is your ability to administer medications. From legal, ethical, and practical standpoints, medication administration is much more than simply a delivery service. It’s a highly technical skill that requires you to exercise wide-ranging knowledge, analytical skill, professional judgment, and clinical expertise. Indeed, some would consider the safe, effective administration of medications the foundation of your success as a professional nurse.
To deliver medications accurately, you need a sound working knowledge of:
Drug terminology
Routes by which drugs are delivered
Effects the drugs produce after they’re inside the body.
Pharmacology is the scientific study of the origin, nature, chemistry, effects, and uses of drugs. This chapter reviews some concepts basic to pharmacology—and essential to your ability to administer drugs wisely—starting with the most basic of all: drug names.
The typical drug has three or more names:
The chemical name describes the drug’s atomic and molecular structure.
The generic name is a shorter, simpler version of the drug’s chemical name.
The trade name (also known as the brand name or propriety name) is the name selected by the drug company that sells it. Trade names are protected by copyright laws.
Most drugs have three names—chemical, generic, and trade/brand—as this example demonstrates. Some drugs may have more than one trade name. The best way to avoid confusion is to use the generic name when speaking or writing about a drug.
| Chemical name
|
| Generic name
|
| Trade name or brand name
|
Drugs that share similar characteristics are grouped together into pharmacologic classes or families. For example, the class known as beta-adrenergic blockers contains several drugs with similar properties.
Drugs can also be grouped according to their therapeutic class, which classifies drugs according to their use. For example, thiazide diuretics and beta-adrenergic blockers are both antihypertensives, but they belong to different pharmacologic classes because they share few characteristics.
A drug’s administration route influences the quantity given and the rate at which the drug is absorbed and distributed. These variables in turn affect the drug’s action and the patient’s response. Routes of administration that involve the gastrointestinal (GI) tract are known as enteral routes, which are from the mouth to the rectum. The enteral routes include oral, sublingual, translingual, buccal, tube feedings and rectal. Those that don’t involve the GI tract or respiratory tract and include the use of a needle are known as parenteral routes. Parenteral routes can be useful for treating a patient who can’t take a drug orally. Compare the advantages and disadvantages of the following routes.
The topical route is used to deliver a drug via the skin or a mucous membrane. The advantages of delivering drugs by this route include:
Easy administration
Few allergic reactions
Fewer adverse reactions than drugs administered by systemic routes.
Delivering precise doses can be difficult with the topical route. Also, these medications can be messy to apply—and even messier for your patient to wear! They may stain the patient’s clothing and bed linens, have a distinctive smell, or get on you as well.

Ophthalmic administration involves drugs such as creams, ointments, and liquid drops that are placed in the conjunctival sac or directly onto the surface of the eye. Intraocular inserts and collagen shields can be used to deliver drugs to the eye as well. For all types of ophthalmic administration, take care to avoid contaminating the medication container or transferring organisms to the patient’s eye.
Ocusert Pilo, one type of intraocular insert, supplies pilocarpine to the ciliary muscles to treat glaucoma. Because this eye medication disk releases the drug for an entire week, it’s more convenient than eyedrops. However, intraocular inserts cost much more than eyedrops and they may be uncomfortable. Also, the drug may be absorbed systemically, causing adverse effects.
Collagen shields that have been presoaked in a drug solution can be applied to the eye to treat corneal ulcers and severe iridocyclitis (inflammation of the iris and ciliary body). Collagen shields may prove more effective than injections of collagen beneath the conjunctiva, where the substance is poorly absorbed.
Otic administration involves drugs that are placed directly into the ear. Solutions placed into the ear can be used to treat infection or inflammation of the external ear canal, produce local anesthesia, or soften built-up cerumen (earwax) for removal.

Bring otic solutions to room temperature before administering them because cold solutions can cause pain or vertigo.
Nasal administration involves drugs that are placed directly into the patient’s nostrils. Medicated solutions can be placed into the patient’s nostrils from a dropper or as an atomized spray from a squeeze bottle or pump device.
The highly vascular nasal mucosa allows systemic absorption while avoiding first-pass metabolism by the liver (the liver changes the drug to a more water-soluble form for excretion before it enters circulation).
Drugs that are lipid-soluble and available as gases can be administered into the respiratory tree. The respiratory tree provides an extensive, highly perfused region for enhanced absorption. Smaller doses of potent drugs can be given by this route to minimize their adverse effects. Because this route is easily accessible, it provides a convenient alternative when other routes are unavailable.
In emergencies, some injectable drugs, such as atropine, lidocaine, and epinephrine, can be given directly into the lungs via an endotracheal tube. A drug administered into the trachea is absorbed into the bloodstream from the alveolar sacs. Surfactant, for example, is administered to premature neonates via the trachea to improve their respiratory function. Also, atropine can be administered to patients with symptomatic bradycardia and no vascular access to increase their heart rate.
| Memory Jogger |
How about ALE to remember the emergency medications that can be administered through an endotracheal tube?
|
A major disadvantage of the respiratory route is that few drugs can be given this way. Other disadvantages include:
Difficulty in administering accurate doses—or full doses, if the patient isn’t cooperative
Nausea and vomiting when certain drugs are delivered into the lungs
Irritation of the tracheal or bronchial mucosa, causing coughing or bronchospasm
Possible infection from the equipment used to deliver drugs into the lungs.
Certain drugs are given buccally (in the pouch between the cheek and teeth), sublingually (under the tongue), or translingually (on the tongue) to prevent their destruction or transformation in the stomach or small intestine. Drugs given by these routes act quickly because the oral mucosa’s thin epithelium and abundant vasculature allow direct absorption into the bloodstream.
These routes can be used if the patient can take nothing by mouth, can’t swallow, or is intubated. What’s more, the drugs have no first-pass effect in the liver and don’t cause GI irritation. However, only drugs that are highly lipid-soluble may be given by these routes, and they may irritate the oral mucosa.
Oral administration is usually the safest, most convenient, and least expensive method. For that reason, most drugs are administered by this route to patients who are conscious and able to swallow.
The oral route does have some disadvantages:
It produces variable drug absorption.
Because it moves drugs through the liver, first-pass metabolism may take place.
Drugs can’t be given orally in most emergencies because of their unpredictable and relatively slow absorption.
Oral drugs may irritate the GI tract, discolor the patient’s teeth, or taste unpleasant.
Oral drugs can be accidentally aspirated if the patient has trouble swallowing or is combative.
| Enteral administration: Why absorption varies A drug that’s administered enterally—orally or by gastric tube—can undergo variable rates of absorption due to:
|
The gastric route allows direct instillation of medication into the GI system of patients who can’t ingest the drug orally. A variety of tubes can be placed for instillation. Oily medications and enteric-coated or sustained-release tablets or capsules can’t be administered by this route.
You may instill suppositories, ointments, creams, or gels into the rectum or vagina to treat local irritation or infection. Some drugs applied to the mucosa of the rectum or vagina can be absorbed systemically. Drugs may also be delivered to the rectum in a medicated enema or to the vagina in a medicated douche.

Drugs administered through the rectal or vaginal routes don’t irritate the upper GI tract, as some oral medications do. Also, these drugs avoid destruction by digestive enzymes in the stomach and small intestine.
However, there are some disadvantages to the rectal and vaginal routes:
The rectal route is usually contraindicated when the patient has a disorder affecting the lower GI tract, such as rectal bleeding or diarrhea.
Drug absorption may be irregular or incomplete with these routes.
The rectal route usually can’t be used in an emergency.
Rectal doses of some drugs may need to be larger than oral doses.
Because rectal administration typically stimulates the vagus nerve, this route may pose a risk for cardiac patients.
Drugs given rectally may irritate the rectal mucosa.
Administering a drug by the rectal or vaginal route may cause discomfort and embarrassment for the patient.
Intradermal drug administration is used mainly for diagnostic purposes when testing for allergies or tuberculosis. To administer drugs intradermally, inject a small amount of serum or vaccine between the skin layers just below the stratum corneum. Because this route results in little systemic absorption, it produces mainly local effects.
You must be sure not to inject the substance too deeply. If you do, you’ll have to reinject it, causing added stress, cost, and delay of treatment for the patient.
When using the subcutaneous route, you inject small amounts of a drug beneath the dermis and into the subcutaneous tissue, usually in the patient’s upper arm, thigh, or abdomen. Patients with diabetes use this technique to give themselves insulin. The drug is absorbed slowly from the subcutaneous tissue, thus prolonging its effects.
There are disadvantages to the subcutaneous route:
Subcutaneous injection may damage tissue.
The subcutaneous route can’t be used when the patient has occlusive vascular disease and poor perfusion because decreased peripheral circulation delays absorption. Exceptions to this are heparin (Lovenox) and insulin.
The subcutaneous route can’t be used when the patient’s skin or underlying tissue is grossly adipose, edematous, burned, hardened, swollen at the common injection sites, damaged by previous injections, or diseased.
Aside from injection, another method of subcutaneous administration is to implant beneath the skin pellets or capsules that contain small amounts of a drug. From the dermis, the medication seeps slowly into the tissues. Goserelin, one such implant, is inserted into the upper abdominal wall to manage advanced prostate cancer.
Because subcutaneous implants require no patient action after they’re in place, they eliminate the problem of noncompliance. Their major drawback is the need for minor surgery to insert or remove them.
The I.M. route allows you to inject drugs directly into various muscle groups at varying tissue depths. You’ll use this route to give aqueous suspensions and solutions in oil and to give medications that aren’t available in oral form. The effect of a drug administered by the I.M. route is relatively rapid, and aqueous I.M. medications can be given to adults in doses of up to 5 ml in some sites. The I.M. route also eliminates the need for an I.V. site.

Despite the advantages, there are many disadvantages to the I.M. route:
A drug delivered I.M. may precipitate in the muscle, thereby reducing absorption.
The drug may not absorb properly if the patient is hypotensive or has a poor blood supply to the muscle.
Improper technique can cause accidental injection of the drug into the patient’s bloodstream, possibly causing an overdose or an adverse reaction.
The I.M. route may cause pain and local tissue irritation, damage bone, puncture blood vessels, injure nerves, or break down muscle tissue, thus interfering with myoglobin—a marker for acute myocardial infarction.
The I.V. route allows injection of substances directly into the bloodstream through a vein. Appropriate substances include drugs, fluids, diagnostic contrast agents, and blood or blood products. Administration can range from a single dose to an ongoing infusion delivered with great precision.
Because the drug or solution is absorbed immediately and completely, the patient’s response is rapid. Instant bioavailability (the drug’s availability for target tissues) makes the I.V. route the first choice for giving drugs during an emergency to relieve acute pain. This route has no first-pass effect in the liver and avoids damage to muscle tissue caused by irritating drugs. Because absorption into the bloodstream is complete and reliable, large drug doses can be delivered at a continuous rate.
Life-threatening adverse reactions may arise if I.V. drugs are administered too quickly, if the flow rate isn’t monitored carefully enough, or if incompatible drugs are mixed together. Also, the I.V. route increases the risk of complications, such as extravasation, vein irritation, systemic infection, and air embolism. Follow the I.V. administration guidelines in chapter 11, Intravenous administration, to help pave your way to success.
Under certain circumstances, drug infusion may take place directly at the site of intended activity. Using specialized catheters and devices, drugs and solutions can be delivered to an organ or its blood vessels to manage emergencies, treat disease, infuse tumors, or relieve pain. These infusions may be given by the epidural, intrapleural, intraperitoneal, intra-articular, or intraosseous routes.
If drug therapy needs to take a direct route to a specific site in the patient’s body, you may use one of the specialized routes of drug administration as shown in this chart.
|
A solid understanding of pharmacokinetics—the movement of a drug through the body—can help you predict your patient’s response to a prescribed drug regimen and anticipate potential problems. Any time you give a drug, a series of physiochemical events takes place in the patient’s body and includes four basic processes:
 Absorption
Absorption Distribution
Distribution Metabolism
Metabolism Excretion.
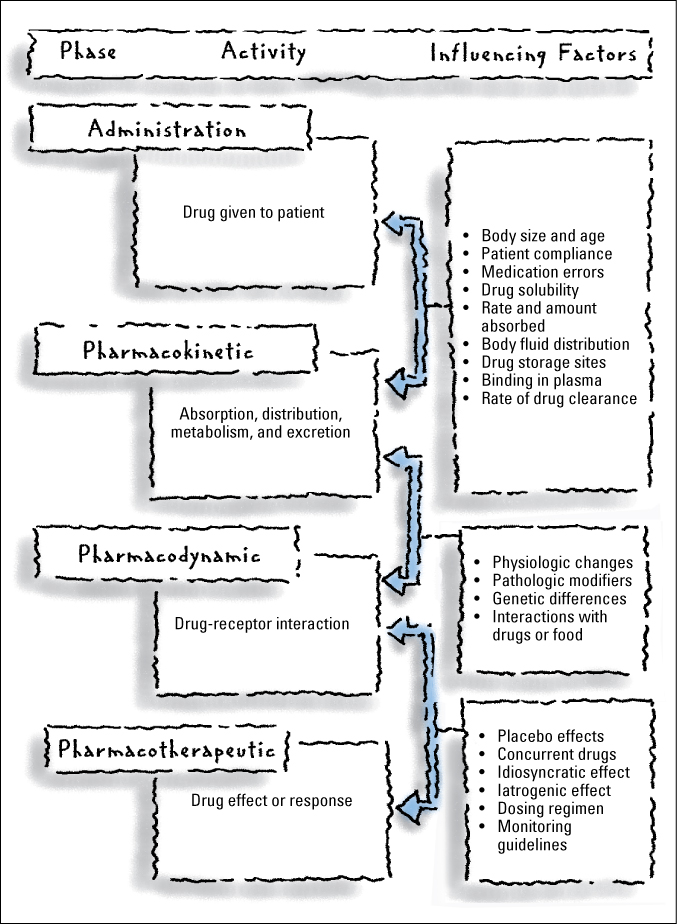
Excretion.Drug disposition begins as soon as a drug is administered. The drug proceeds through pharmacokinetic, pharmacodynamic, and pharmacotherapeutic phases. This chart shows the various phases, the activities that occur during them, and the factors that influence those activities.

Before a drug can act on the body, it must be absorbed into the bloodstream. How well a patient’s body absorbs a drug depends on several factors. These include:
The drug’s physiochemical properties
The drug’s form
The route of administration
The drug’s interactions with other substances in the GI tract
Various patient characteristics, especially the site and the condition of the absorbing surface.
These factors can also determine the speed and amount of drug absorption.
When taken orally, some drug forms, such as tablets and capsules, may have to disintegrate before free particles are available to dissolve in the gastric juices. Only after dissolving in these juices can the drug be absorbed, circulate in the bloodstream, and thus become bioavailable. A bioavailable drug is one that’s ready to produce a physiologic effect.
Some tablets have enteric coatings, which delay disintegration until after the tablets leave the acidic environment of the stomach. Others, such as liposome capsules, have special delivery systems that release the drug only at a specific osmotic pressure. Oral solutions and elixirs, which don’t have to disintegrate and dissolve to take effect, are usually absorbed more rapidly.
If the patient has had a bowel resection, anticipate slow absorption of any oral drug you administer. And remember that a drug given I.M. must first be absorbed through the muscle before it can enter the bloodstream. Rectal suppositories must first dissolve to be absorbed through the rectal mucosa. Drugs administered I.V.—thereby placed directly into the bloodstream—are completely and immediately bioavailable.
When a drug enters the bloodstream, it’s distributed to body tissues and fluids through the circulatory system. To better understand drug distribution, think of the body as a system of physiologic compartments defined by blood flow. The bloodstream and highly perfused organs—such as the brain, heart, liver, and kidneys—make up the central compartment. Lesser perfused areas form the peripheral compartment, which is subdivided into the tissue compartment (viscera, muscle, and skin) and the deep compartment (fat and bone).
Highly perfused tissues receive the drug before lesser perfused areas do. Each compartment then stores portions of the drug, releasing it as plasma drug levels decline.
How the body stores a drugThe body can store a drug in fat, bone, or skin. Knowing the characteristics of each drug storage compartment will help you understand how distribution can affect a drug’s duration of action.
| Fat storage A drug that dissolves easily in lipids migrates to adipose tissue (what we commonly think of as fatty tissue). Because this tissue lacks receptors for drug action, the drug remains inactive there. Eventually, it’s released by fat cells to exert its pharmacologic effect. With some drugs, this slow, prolonged action is an advantage. For example, slow release of anesthetic barbiturates provides effective anesthesia during surgery. With other drugs, such prolonged action can be dangerous. |
| Bone storage Bone acts as a storage compartment for certain drugs. Tetracycline, for example, is distributed throughout bone and may eventually crystallize there. In a growing child, this can cause tooth discoloration. Lead and some chemicals can also accumulate in bone, resulting in prolonged exposure to toxins. |
| Skin storage Storage of drugs in the skin typically causes photosensitivity. Tetracycline and amiodarone are examples of drugs that are stored in the skin. |
Distribution also depends partly on a drug’s ability to cross lipid membranes. Some drugs can’t cross certain cell membranes and thus have limited distribution. For example, antibiotics have trouble permeating the prostate gland, abscesses, and exudates.
Distribution can also be affected if the drug binds to plasma proteins, especially albumin. Only a free, unbound drug can produce an effect at the drug receptor site, so such binding greatly influences the drug’s effectiveness and duration of action.
Certain diseases impede drug distribution by altering the volume of distribution—the total amount of drug in the body in relation to the amount in plasma. Heart failure, dehydration, and burns are examples of such disorders. If the patient has heart failure, expect to increase the dosage because the drug must be distributed to a larger fluid volume. On the other hand, if the patient is dehydrated, expect to decrease the dosage because the drug will be distributed to a much smaller fluid volume.
Some drugs—such as digoxin, gentamicin, and tobramycin—are poorly distributed to fatty tissue. Therefore, dosing based on actual body weight in a highly obese patient may lead to overdose and serious toxicity.
| Go lean When administering such drugs, calculate the dose based on lean body weight, which you can estimate from actuarial tables that give average weight ranges for various heights. |
Most drugs are metabolized in the liver and excreted by the kidneys. The rate at which a drug is metabolized varies with the individual. Some patients metabolize drugs so quickly that their blood and tissue levels prove therapeutically inadequate. Others metabolize drugs so slowly that even ordinary doses can produce toxic results.
Drug metabolism may be faster in smokers than in nonsmokers because cigarette smoke contains substances that induce production of hepatic enzymes. Also, a diet high in fat or carbohydrates may slow the metabolism of certain drugs, whereas a diet high in protein may speed metabolism.
Hepatic diseases, or diseases that interfere with hepatic blood flow or transport of drugs to the liver, may affect one or more of the liver’s metabolic functions. Thus, in patients with hepatic disease, drug metabolism may be increased or decreased. All patients with hepatic disease must be monitored closely for drug effects and toxic reactions.
Some drugs, such as digoxin and gentamicin, are eliminated almost unchanged by the kidneys. Thus, inadequate renal function causes the drug to accumulate, producing toxic effects. Some drugs can block renal excretion of other drugs, thereby allowing them to accumulate and enhancing their effects. In contrast, some drugs can promote renal excretion of other drugs, thus diminishing their effects.
Although most drugs are excreted by the kidneys, not all are. Some are excreted hepatically, via the bile and into stool. A few drugs leave the body in sweat, saliva, and breast milk. Certain volatile anesthetics—for example, halothane—are eliminated primarily by exhalation. When natural excretion mechanisms fail, as in drug overdose or renal dysfunction, many drugs can be removed through dialysis.
Underlying disease can have a marked influence on drug action and effect. For example, acidosis may cause insulin resistance. Genetic diseases, such as glucose-6-phosphate dehydrogenase (G6PD) deficiency and hepatic porphyria, may turn drugs into toxins. As a result, patients with G6PD deficiency may develop hemolytic anemia when given sulfonamides or certain other drugs.

A genetically susceptible patient can develop an acute porphyria attack if given a barbiturate.
Also, patients with highly active hepatic enzyme systems (rapid acetylators, for example) can develop hepatitis when treated with isoniazid because of the rapid intrahepatic buildup of a toxic metabolite.
Other conditions that may influence a patient’s response to drug therapy include infection; fever; stress; starvation; hypersensitivity; sunlight; exercise; variations in circadian rhythm; alcohol intake; pregnancy; lactation; immunization; barometric pressure; and GI, renal, hepatic, cardiovascular, and immunologic function.
The patient’s age has an important influence on a drug’s overall action and effect. Older adults usually have decreased hepatic function, less muscle mass, and diminished renal function. Consequently, they need lower doses and, sometimes, longer dosage intervals to avoid toxicity.
Neonates have underdeveloped metabolic enzyme systems and inadequate renal function, which can also lead to toxicity. They need highly individualized dosages and careful monitoring.
In an outpatient setting, the process of ordering a medication is rather simple. A prescriber typically writes the order on a prescription pad and gives it to the patient. The patient then takes the written prescription and has it filled at a pharmacy.
In an inpatient setting, however, the process may be somewhat more complex. Several types of medication orders can be used for in patient, including:
Standard orders
Single (or one-time) orders
Stat orders
P.r.n. orders
Standing orders
Verbal orders
Telephone orders.
A standard order is a prescription that remains in effect indefinitely or for a specified period. The prescriber either writes the order—along with instructions, such as for diet, X-rays, and laboratory work—on the order sheet in the patient’s chart or enters the order into a computer, and then the order is printed out on a computer-generated patient record.
The order must specify the name of the medication, dosage, route of administration, frequency, duration (if time limited), and indication (if p.r.n.). For example, the order might be written this way: Amoxil 500 mg P.O. q 8 hr × 10 days.
Components of a medication orderFor a hospitalized patient, a prescriber writes a medication order on an order sheet in the patient’s chart or enters the order into the computer system. An example of a written order is shown here.
| Component list Whether written or entered into the computer, all drug orders must contain:
|

It’s your job to schedule administration times based on the order, your facility’s policies, and pertinent characteristics of the medication itself, such as onset and duration of action and whether it’s to be given with or without food.
If a standard order doesn’t specify a termination time, the order usually remains in effect until the prescriber writes another order to replace or discontinue it. For some types of drugs, however, the amount of time covered by the order may be limited by facility policy. For example, opioid orders may have a controlled delivery time of 3 days. Some antibiotics may have a controlled delivery time of 7 days. If the patient still needs the drug after the termination date has passed, the prescriber must write another order. The same is true for postoperative medications; the prescriber must rewrite standard orders for all medications that are to continue after surgery.
When a medication is to be given only once, a prescriber writes what’s called a single order. For example, he may order one injection of tetanus toxoid for a patient with a puncture wound who received a primary tetanus toxoid series more than 5 years earlier.
If a patient needs a medication right away for an urgent problem, a prescriber writes a stat order. For example, he may order an immediate single dose of an antianxiety drug to calm an acutely agitated patient. For a patient with acute chest pain, he may write a stat order for nitroglycerin (sublingual, spray, or I.V. form).
The term p.r.n. comes from a Latin phrase that means “as the occasion arises.” A p.r.n. order allows you to give a medication when the patient needs it for a specified problem, such as pain, fever, and constipation. Naturally, you should exercise sound professional judgment in determining when and how often to administer a drug p.r.n.
Sometimes, a p.r.n. order specifies a reason for giving the drug. For example, the prescriber may order acetaminophen 650 mg P.O. q 4 hr, p.r.n. for a temperature above 101.3° F (38.5° C).
Although acetaminophen can be used to treat various problems, in this case, your facility may allow you to give it only for the purpose stated in the medication order. In other words, under such a policy, you couldn’t give the acetaminophen ordered above if the patient complained of a headache but had no fever.
Any time you administer a p.r.n. medication, explain your reason for giving it in the patient’s record. Also, describe its degree of effectiveness.
Also known as protocols, standing orders are derived from guidelines created by health care providers for use in specific settings to treat certain diseases or sets of symptoms. Some units of a health care facility (such as the coronary care unit) routinely employ standing orders. For example, the unit may have standing orders for morphine sulfate to treat chest pain and anxiety, for lidocaine to treat ventricular tachycardia, and for furosemide to treat pulmonary congestion.

Standing orders specify which drugs you’re permitted to administer and under which circumstances. They must still be individually reviewed and ordered for each patient by his provider. That is, there must be an order to enact the standing orders. Standing orders may also provide guidelines or algorithms for making dosage adjustments. For example, you may need to change the dosage of a heparin infusion based on your patient’s anticoagulation studies.
Standing orders require considerable judgment and expertise on your part in assessing a patient’s need for a drug and detecting any dose-related adverse reactions that could occur. No standing order should be automatically implemented without a careful review regarding its appropriateness for a given patient at a given time.
Medication orders given orally rather than in writing are known as verbal orders. Whenever possible, avoid them. Why? Because miscommunications can occur and you’ll lack a written record of the order.
| Stay on the Ball |
| Telephone order accuracy If you have to take a medication order over the telephone, follow these steps to help ensure its accuracy:
|
The danger of miscommunication rises even higher when a prescriber gives a verbal medication order over the telephone. A bad connection, commotion on either end, or the lack of nonverbal communication cues can easily result in medication errors if you fail to clarify exactly what the prescriber wants.
If possible, use a fax machine to obtain a written order, instead of taking a verbal order over the phone.

In urgent situations, you may not be able to avoid verbal orders. Repeat the order aloud so the prescriber can verify that you understood it. For example, your patient goes into hypoglycemic or insulin shock and the doctor tells you to immediately prepare 50 ml of 50% glucose for I.V. administration. To verify the order, show the doctor the label on the empty glucose vial and say the drug’s name out loud as you hand him the syringe. That way, he can confirm the accuracy of the drug and its dose.
Anytime you accept a verbal order, it’s your responsibility to ensure the accuracy of the communication. This holds true even in an emergency. Ask the prescriber to spell the drug’s name if you aren’t sure what it is. Afterward, write and sign the order that was given to you verbally by the prescriber. Then have the prescriber sign your written copy as soon as possible. Your facility should have a policy that specifies a time frame allotted for a prescriber to sign a verbal order.
Making sure you understand a medication order is just the start of your responsibilities when it comes to administering medications correctly. Next, you have to make your own judgment about the correctness of the order based on your knowledge of the medication and your understanding of the patient’s condition.

After you have looked up the drug in the drug guide and you’re convinced that a medication order is appropriate for the drug and the patient involved, your next step is to prepare the drug correctly for administration.
Orders into actionAfter you receive a written medication order, transcribe it onto a working document approved by your health care facility. For example, your facility may want you to use a medication administration record (MAR), a medication Kardex, medication cards or tickets, or a computer printout.
| Stepping away from errors Each time you copy a medication order, you introduce the possibility of making an error. Make sure you follow these steps:
|
| Don’t rely on memory Next, prepare the medication from the approved copy. Never prepare a medication from memory or from your personal worksheets or notes. To reduce the risk of overlooking a medication order, your facility may require you to periodically check all MARs against the original order sheets. |
After you transcribe the medication order onto a working document, go to a quiet area to prepare the medication for delivery. Then follow the 6 rights of medication administration.
Following a tried-and-true set of safeguards known as the 6 rights can quickly and easily help you avoid the most basic and common sources of medication error. Each time you administer a medication, confirm that you have the:
 Right drug
Right drug Right dose
Right dose Right patient
Right patient Right time
Right time Right route
Right route Right documentation.
Right documentation.
Always compare the name of an ordered drug with the name printed on the container label. Take your time and do it carefully; drugs with similar-sounding and similar-looking names may have very different indications and effects.

For example, Celexa (citalopram hydrobromide) and Celebrex (celecoxib) sound quite similar. But Celexa is a selective serotonin reuptake inhibitor used to treat depression. Celebrex is a nonsteroidal anti-inflammatory drug used to treat osteoarthritis and rheumatoid arthritis. Other similar-sounding drugs may raise a similar risk of mix-ups.
When a medication is individually wrapped in single doses, check the name when removing it from the drawer and again when unwrapping and giving the drug to the patient. Always mention the drug name and the reason you’re giving it before actually giving it to the patient.
Besides carefully checking the ordered drug name against the container label, also check the patient’s reaction to the drug as you try to administer it. If he says, “I usually take one pink pill, but you’ve given me two yellow pills,” stop what you’re doing and recheck the order. Perhaps you’ll simply explain to the patient that the pink pill contains 10 mg of the drug and the yellow ones contain 5 mg each. Or perhaps, you’ll discover that you’re giving the patient the wrong medication. Either way, you must carefully follow up on any comment a patient makes about changes in a medication before you administer it.
The growing use of unit-dose medications (in which a single dose of medication is wrapped and labeled for individual use) has greatly reduced the risk of giving a patient the wrong drug dose. Also, many commercially prepared medications are available in various tablet sizes, decreasing the number of calculations you have to do to determine the dosage.
Even so, you still need to know how and when to perform the appropriate dose calculations.
| Stay on the Ball |
| Keeping calculations correct A recent study of 200 equation-based prescribing errors found that more than one half resulted from calculation mistakes. To help keep your medication calculations correct, use these safeguards:
|
Whenever possible, double-check all your calculations with another nurse or with a pharmacist. Many hospitals require these double checks when your dosage calculations involve children’s medications or drugs with narrow safety margins, such as heparin and insulin.
No matter what, never take it upon yourself to alter the drug dosage specified in a prescriber’s order. Say, for example, that a doctor orders 75 mg of meperidine for postoperative pain. You give the medication after the patient’s surgery, but he says he still has intense pain. Your conclusion may be that 75 mg of meperidine isn’t enough and that 100 mg would probably do the trick. But that doesn’t give you the authority to change the dose.
Instead, consult with the doctor and obtain a new standard order. However, if the prescriber’s original medication order specifies a range of dosages, then you must determine the most appropriate dose for the patient—within that range.
To reduce the risk of medication errors, never assume that the patient in a labeled bed is indeed the patient named on the label. Instead, always use two patient identifiers (neither of which should be the patient’s room number) before giving any medication. One new identifier used by some hospitals is the bar code medication administration method. The nurse scans their identification badge, the patient’s bracelet, and the medication bar code on the drug that is to be administered to the patient. (Follow agency policy for patient identification.)
As an additional check, also ask the patient to tell you his name and birthdate. (Don’t say something like, “You’re John, right?” because the patient could misunderstand you, could be confused, or could be a different John than the one scheduled for a medication.)
The considerations that make an administration time the “right” time may be therapeutic, practical, or both. For therapeutic purposes, the right time is one that appropriately maintains the level of drug in the patient’s bloodstream. For practical purposes, the right time is one that’s convenient for the staff and the patient. Naturally, therapeutic goals take precedence over practical ones.

To meet therapeutic goals, you may need to space the delivery of some medications evenly around the clock. Doing so helps to maintain a consistent level of the drug in the patient’s bloodstream. If you don’t have a particular need to space the drug delivery over 24 hours, you can space it over the patient’s waking hours to avoid disrupting his sleep.
For some drugs, you may need to measure the patient’s therapeutic response before determining whether it’s the right time to give another dose. For example, you should check the patient’s apical pulse rate (determined by cardiac auscultation for 1 minute) before giving digoxin, and you should assess the patient’s respiratory rate before giving morphine.
Besides maximizing the therapeutic effect, giving medications at specified, evenly spaced intervals provides some practical benefits. For one thing, it allows you to plan administration times that don’t interfere with meals or especially busy times on the nursing unit. For example, instead of scheduling twice-daily administration times at 8 a.m. and 6 p.m., which are common times for shift changes, schedule them at 9 a.m. and 7 p.m. instead.
Another practical benefit of standardized administration times is that they establish a habit in the patient’s mind. This may make it easier for him to keep taking the medication appropriately when he gets home.
Regardless of the reasons behind the administration times you establish for the patient, you’ll need to follow those times carefully. In fact, many facilities consider it a medication error if you fail to give a medication within 30 minutes before or after its scheduled administration time.

Always pay careful attention to the administration route specified in the medication order, on the product’s label, and in the drug guide. Also, make sure the ordered form of the drug is appropriate for the intended route. Only drugs labeled “for injection” should be used for injections of any kind.
Before you give the drug, consider whether the amount ordered is appropriate for the route by which you’re preparing to give it. For example, 10 mg is an appropriate amount of morphine sulfate to give by the I.M. route to relieve pain in an adult. If the patient will be receiving it by the I.V. route, however, the equivalent dose would be more like 2 to 4 mg. If they are taking the drug orally, they will need more than 10 mg to achieve the same effect.

Remember that the route by which you give a drug affects the rate at which it gets absorbed into the patient’s bloodstream. Because certain forms of a drug may be intended for specific routes, be careful not to interfere with a drug’s action by changing routes or circumventing the chemical preparation. For example, you wouldn’t want to crush an enteric-coated tablet or open a sustained-release capsule.
Working with sustained-release drugsA growing number of drugs are being formulated to exert an effect over many hours. The components of each drug dose dissolve at different rates, thus releasing the drug gradually but continuously into the patient’s bloodstream. Convenient for staff and patients, sustained-release drugs require fewer doses per day and provide steadier control over symptoms.
| Easy identification Sustained-release drugs are supplied as plain tablets, coated tablets, and capsules filled with tiny granules. They may be identified by an SR (for sustained release) after the drug name, or they may have one of a number of prefixes attached to the name that suggests an extended effect. Some common examples include Quinaglute Dura-Tabs, Dimetapp Extentabs, Chlor-Trimeton Repetabs, and Desoxyn Gradumets. You may also see such names as Spansules and Gyrocaps. |
| Don’t split, crush, or chew Never split or crush a sustained-release drug. Warn the patient not to chew the drug and to never open a sustained-release capsule to mix the granules into foods or beverages. All of these actions could alter the drug’s absorption rate, put too much drug into the patient’s bloodstream too quickly, or reduce the drug’s overall effect. |
You can also help increase the speed at which topical nitroglycerin enters a patient’s bloodstream by spreading it over a larger skin area and covering it with plastic wrap.
On the other hand, you can decrease the rate of absorption and effectiveness of a drug. For example, if a patient chews or swallows a sublingual drug, such as sublingual nitroglycerin, the rate of absorption and effectiveness will be decreased.
After administering the medication with the 5 rights completed, your 6th right is to document the administration correctly on the right patient following your facilities policy on documenting medications. There are many ways to document for example: paper charts, computerized charting, finger printing and bar-code scanning.
The 6 rights of medication administration afford you a basic level of protection against medication errors. However, most experts consider them the minimum requirement. Here are some additional measures you should take to help avoid medication errors.
Follow these guidelines when storing and preparing drugs:
Store and handle drugs carefully to maintain their stability and potency. Remember that some drugs can be altered by temperature, air, light, and moisture; make sure you follow all drug-specific precautions. Some drugs may need to be kept in brown bottles. Some I.V. bags may need to be covered with foil to block the light during infusion.
Always keep drugs in the containers in which the pharmacy dispensed them. Cap all containers tightly. If you see small cylinders in a container, they probably serve to absorb moisture and keep the product fresh; don’t remove them.
Store drugs at room temperature unless you’re instructed to refrigerate them. Refrigeration causes moisture to form and could alter some drugs through condensation.
As required by law, keep opioids and controlled substances under double lock.

Always note a drug’s expiration date—the date after which it loses some amount of potency. Never administer an outdated drug or one that looks or smells unusual.
If the original package looks like someone may have tampered with it, don’t give the drug; instead, return it in its package to the pharmacy for an investigation.
Check the medication label three times—when you take it from the shelf or drawer, before putting it into the medication cup, and before returning the container to the shelf or drawer—to make sure you’re giving the prescribed medication. For a unit-dose medication, check the label just after obtaining the medication and again before discarding the wrapper.
You may need to reconstitute a drug dispensed as a powder just before you administer it. If medication is left over after you remove your dose, label the container with the date, time, strength, and your initials or signature.
Never administer a drug that wasn’t labeled properly after reconstitution.
Discard any drug that will reach its expiration date before another dose is scheduled.
If you find an unlabeled syringe with medication inside, discard it.
Let a refrigerated drug reach room temperature before administering it, unless you’re instructed otherwise.

Follow these guidelines when administering drugs:
Before administering a medication based on new orders, review the patient’s medication history for known allergies or other problems. Always ask the patient if they have any allergies to medications including over-the-counter medications.
If you know a patient has a drug allergy, make sure the chart clearly displays the allergy.
Never administer a drug to you patient that you haven’t given before if you haven’t first looked it up in the drug guide.
When you deliver drugs to a patient’s room, stay with the medication cart. Never leave without locking the cart and taking it back to the medication room or its usual storage place.
Assess the patient’s physiologic and psychological condition before administering any medication.
Stay with the patient until they take the medication to verify that they took it as directed.
Never leave medication doses at a patient’s bedside unless you have a specific order to do so.
Administer only medications you’ve prepared personally or that the pharmacist prepared.
Never administer a drug that another nurse asks you to give to their patient.
Don’t open individually prepared doses (unit-dose medications) until you’re at the bedside and you’ve confirmed the patient’s identity.
When administering an oral drug, urge the patient to drink a full glass of water, if appropriate. Doing so helps move the medication out of the esophagus and into the stomach. It also dilutes the drug, thus reducing the chance of gastric irritation.
If a medication order specifies that you should leave a drug at the patient’s bedside for self-administration, label the drug with:
Patient’s name
Drug name
Dosage
Instructions the patient needs.
Drugs commonly left at the patient’s bedside include antacids and nitroglycerin tablets.
| Supervision requires a super nurse In most health care facilities, you’re responsible for supervising a patient whose drugs are left at the bedside. For example, you must know how many nitroglycerin tablets the patient took, the exact times of self-administration, the degree of relief he obtained, and any unusual reactions he had to the drug. Record this information in the patient’s chart, and report it to the prescriber. |

Document drugs immediately after you administer them. Delayed charting, especially of p.r.n. medications, can result in repeated doses. Documenting before giving a medication can lead to missed doses.
Record your observations of the patient’s positive and negative responses to the medication. For example, if you give an antibiotic to a patient with pneumonia, chart such positive responses as decreased sputum, reduced fever, and easier breathing to confirm the drug’s effectiveness. Also, chart such adverse reactions as skin eruptions or gastric upset. Severe adverse reactions may prompt the prescriber to substitute another drug.
Yet another area of medication administration that you’ll need to master is the drug delivery system. Your facility may use one of several systems by which you can obtain ordered drugs from the pharmacy. In each one, you serve a vital coordinating function between the prescriber and the pharmacist.

Regardless of the delivery system used by your facility, the doctors, nurses, and pharmacists must collaborate to make it work effectively. Common drug delivery systems include:
Unit-dose system
Automated systems
Individual prescriptions.
In a unit-dose system, the pharmacist dispenses a supply of wrapped, labeled individual doses of all forms of drugs: oral, injectable, and I.V. solutions with additives. The pharmacist usually dispenses sufficient drugs and I.V. solutions to last 24 hours; he may also prepare trays of medications for you to administer at specified hours.
The pharmacist may prepare unit doses or purchase them commercially. They usually place each patient’s drugs in an individual drawer of a portable medication cart. Keep the drugs in their labeled wrappers until you actually administer them. The unit-dose system reduces the likelihood of drug administration errors.
In essence, an automated drug delivery system is a computerized version of the unit-dose system. A pharmacist fills an electronic drug-dispensing unit and keeps it locked. The unit then delivers individually wrapped and labeled medications when you request them. A computer records all drug transactions on electronic tape and furnishes requested printouts.
To avoid the possibly disastrous effects from computer downtime, facilities that use automated dispensing systems must have a backup plan for dispensing medications and documenting their delivery.

An automated system greatly simplifies record keeping because the computer can monitor and track drugs from the original inventory to patient billing. It saves staff time and may allow you to spend more time teaching and consulting with patients.
Understanding automated drug deliveryAn automated drug delivery system may free you from doing some of what you currently do by hand. For example, you may no longer have to transcribe medication orders or procure and store drugs.
| The responsibility stays the same However, keep in mind that an automated system doesn’t relieve you of the responsibility for noting medication orders and administering medications properly. It also can’t take your place in unusual patient circumstances in which a computer can’t render your professional judgments. |
In an individual prescription system, a pharmacist fills a prescription using a container that has been labeled for a particular patient. You then administer the drug to the patient directly from the container. Because the drug is designated for a particular person, this system reduces the risk that you’ll give a drug to the wrong patient. However, the system is cumbersome and slow because the medication order must travel from you to the pharmacy and back to you again.
In addition to following your facility’s policies faithfully, you can help prevent medication errors by studying common ones and avoiding the slip-ups that allowed them to happen.
As you read earlier, drugs with similar-sounding names can be easy to confuse. Keep in mind, however, that even different-sounding names can look similar when written out rapidly by hand on a medication order: Soriatane and Loxitane, for example, both of which are capsules. Any time a patient’s drug order doesn’t seem right for the diagnosis, call the doctor to clarify the order.
Many nurses have confused an order for morphine with one for hydromorphone (Dilaudid). Both drugs come in 4-mg prefilled syringes. If you give morphine when the doctor really ordered hydromorphone, the patient could develop respiratory depression or even arrest.
Consider posting a prominent notice in your medication room that warns the staff about this common mix-up. Or try attaching a fluorescent sticker printed with “not morphine” to each hydromorphone syringe and a sticker of a different color printed with “not hydromorphone” to each morphine syringe.
Drug names aren’t the only kinds of words you can confuse. Patient names can cause trouble as well if you fail to verify each person’s identity. This problem can be especially troublesome if two patients have the same first name.

Consider this clinical scenario: Robert Brewer, age 5, was hospitalized for measles. Robert Brinson, also age 5, was admitted after a severe asthma attack. The boys were assigned to adjacent rooms on a small pediatric unit. Each had a nonproductive cough. When Robert Brewer’s nurse came to give him an expectorant, the child’s mother told the nurse that Robert had already inhaled a medication through a mask.
The nurse quickly figured out that another nurse, new to the unit, had given Robert Brinson’s medication (acetylcysteine, a mucolytic) to Robert Brewer in error. Fortunately, no harmful adverse effects ensued. Had the nurse checked the patient’s identity more carefully, however, no error would have occurred in the first place.
Always check each patient’s full name and birthdate. Also, teach each patient (or parent) to offer an identification bracelet for inspection and to state a full name and birthdate when anyone enters the room with the intention of giving a medication. In addition, urge patients to tell you if an identification bracelet falls off, is removed, or gets lost. Replace it right away.
You aren’t the only one who’s at risk for making medication errors. Patients are at an even greater risk because they know so much less about medications than you do.
Clearly, patient teaching is a crucial aspect of your responsibility in minimizing medication errors and their consequences—especially as more patients receive outpatient rather than inpatient care.
| Teaching tips You can help minimize medication errors by:
|
After you’ve verified your patient’s full name, take time to check whether he has drug allergies—even if they are in distress. If the patient has an allergy, immediately document the allergy in the appropriate places such as the chart, MAR, wristband, and the pharmacy and report to the doctor.
Consider this real-life example: A doctor issued a stat order for chlorpromazine (Thorazine) for a distressed patient. By the time the nurse arrived with it, the patient had grown more distressed and was demanding relief. Unnerved by the patient’s demeanor, the nurse gave the drug without checking the patient’s MAR or documenting the order—and the patient had an allergic reaction to it.

Any time you’re in a tense situation with a patient who needs or wants medication fast, resist the temptation to act first and document later. Skipping that crucial assessment step could easily lead to a medication error.
A patient who’s severely allergic to peanuts could have an anaphylactic reaction to Atrovent aerosol given by metered-dose inhaler. Ask the patient or the parents whether they are allergic to peanuts before you administer this drug.
If you find that they have such an allergy, you’ll need to use the nasal spray and inhalation solution form of Atrovent. Because it doesn’t contain soy lecithin, this form of the drug is safe for patients who are allergic to peanuts.
Many medication errors stem from compound problems—a mistake that could have been caught at any of several steps along the way. For a medication to be administered correctly, each member of the health care team must fulfill the appropriate role. The doctor must write the order correctly and legibly. The pharmacist must evaluate whether the order is appropriate and then fill it correctly. In addition, the nurse must evaluate whether the order is appropriate and then administer it correctly.
A breakdown anywhere along this chain of events can lead to a medication error. That’s why it’s so important for members of the health care team to act as a real team, checking each other and catching any problems that arise before those problems affect the patient’s health. Do your best to foster an environment in which professionals can double-check each other.

For example, the pharmacist can help clarify the number of times a drug should be given each day, help you label drugs in the most appropriate way, and remind you to always return unused or discontinued medications to the pharmacy.
You must clarify any doctor’s order that doesn’t seem clear or correct. You must also correctly handle and store any multi-dose vials obtained from the pharmacist. Additionally, store drugs in their original containers to avoid errors.
Even a confusing container can cause a medication error if you aren’t careful. For example, it’s easy to mistake eyedrops for the developers used for the Hemoccult test. Some patients have sustained permanent eye damage as a result. The best way to avoid this mistake is to keep Hemoccult developers in an appropriate room (such as the utility room). Never keep them in a patient’s room.
Only administer drugs that you’ve prepared personally. Never give a drug that has an ambiguous label or no label at all. Here’s an actual example of what could happen if you do: A nurse placed an unlabeled cup of phenol (used in neurolytic procedures) next to a cup of guanethidine (a postganglionic-blocking agent). The doctor accidentally injected the phenol instead of the guanethidine, causing severe tissue damage to a patient’s arm. The patient needed emergency surgery and developed neurologic complications.
Obviously, this was a compound problem. The nurse should have labeled each cup clearly, and the doctor shouldn’t have given an unlabeled substance to a patient.
Many medication errors stem at least in part from problems related to the route of administration. The risk of error increases when a patient has several lines running for different purposes.
Consider this example: A nurse prepared a dose of digoxin elixir for a patient who had a central I.V. line and a jejunostomy tube—and she mistakenly administered the drug into the central I.V. line. Fortunately, the patient had no adverse reaction. To help prevent such mix-ups in administration route, prepare all oral medications in a syringe that has a tip small enough to fit an abdominal tube but too big to fit a central line.
Here’s another error that could have been avoided: To clear air bubbles from a 9-year-old patient’s insulin drip, a nurse disconnected the tubing and raised the pump rate to 200 ml/hour to flush the bubbles through quickly. The nurse then reconnected the tubing and restarted the drip, but she forgot to reset the rate back to 2 units/hour. The child received 50 units of insulin before the error was detected. To prevent this kind of error, never increase a drip rate to clear bubbles from a line. Instead, remove the tubing from the pump, disconnect it from the patient, and use the flow-control clamp to establish gravity flow.
You carry a great deal of responsibility for making sure that patients get the right drugs in the right concentrations at the right times and by the right routes. By diligently applying the guidelines offered here, you can minimize your risk of medication errors and maximize the therapeutic effects of your patients’ drug regimens.
References
Berman, A., & Snyder, S. J. (2012). Skills in clinical nursing (7th ed.). Upper Saddle River, NJ: Pearson Education.
Berman, A., Snyder, S. J., & McKinney, D. S. (2011). Nursing basics for clinical practice. Upper Saddle River, NJ: Pearson Education.
Hogan, M., Bolten, S., Ricci, M., & Taliaferro, D. (2008). Nursing fundamentals (2nd ed.). Upper Saddle River, NJ: Pearson Prentice Hall.
Treas, L. S., & Wilkinson, J. M. (2014). Basic nursing concepts, skills & reasoning. Philadelphia, PA: F.A. Davis.
![]()
Which branch of pharmacology deals with the study of interactions between drugs and living tissues and serves as the basis of drug treatment?
Which type of order poses the highest risk of error?
Which type of inpatient medication order remains in effect indefinitely or for a specified period?
 If you answered all three questions correctly, excellent! You’re on the route to greatness.
If you answered all three questions correctly, excellent! You’re on the route to greatness. If you answered two questions correctly, you’re getting the essentials! You used the key concepts to unlock the door to understanding.
If you answered two questions correctly, you’re getting the essentials! You used the key concepts to unlock the door to understanding. If you answered fewer than two questions correctly, don’t worry! Go back and review this chapter, and soon you’ll be pharmaco-dynamite.
If you answered fewer than two questions correctly, don’t worry! Go back and review this chapter, and soon you’ll be pharmaco-dynamite.Outline