![]()
In this chapter, you’ll learn:
Uses of I.V. therapy
I.V. delivery methods
I.V. infusion rates
Legal and professional standards governing the use of I.V. therapy
Patient teaching regarding I.V. therapy
Proper procedures for documenting I.V. therapy.
One of your most important nursing responsibilities is to administer fluids, medications, and blood products to patients. In I.V. therapy, liquid solutions are introduced directly into the bloodstream.
I.V. therapy is used to:
Restore and maintain fluid and electrolyte balance
Provide medications and chemotherapeutic agents
Transfuse blood and blood products
Deliver parenteral nutrients and nutritional supplements.
I.V. therapy has great benefits. For example, it can be used to administer fluids, drugs, nutrients, and other solutions when a patient can’t take oral substances.
I.V. drug delivery also allows more accurate dosing. Because the entire amount of a drug given I.V. reaches the bloodstream immediately, the drug begins to act almost instantaneously.
Like other invasive procedures, I.V. therapy has its downside. Risks include:
Bleeding
Blood vessel damage
Infiltration (infusion of the I.V. solution into surrounding tissue rather than the blood vessel)
Infection
Overdose (because response to I.V. drugs is more rapid)
Incompatibility when drugs and I.V. solutions are mixed
Adverse or allergic responses to infused substances.
Patient activity can also be problematic. Simple tasks, such as transferring to a chair, ambulating, and washing oneself, can become complicated when the patient must cope with I.V. poles, I.V. lines, and dressings.
Finally, I.V. therapy is more costly than oral, subcutaneous, or I.M. methods of delivering medications.
One of the primary objectives of I.V. therapy is to restore and maintain fluid and electrolyte balance. To understand how I.V. therapy works to restore fluid and electrolyte balance, let’s first review some basics of fluids and electrolytes.
The human body is composed largely of liquid. These fluids account for about 60% of total body weight in an adult who weighs 155 lb (70.3 kg) and about 80% of total body weight in an infant.
Body fluids are composed of water (a solvent) and dissolved substances (solutes). The solutes in body fluids include electrolytes (such as sodium) and nonelectrolytes (such as proteins).
What functions do body fluids provide? They:
Help regulate body temperature
Help transport nutrients throughout the body
Carry cellular waste products to excretion sites.
When fluid levels are optimal, the body performs swimmingly; however, when fluid levels deviate from the acceptable range, organs and systems can quickly become congested.
Body fluids exist in two major compartments: inside the cells and outside the cells. Normally, the distribution of fluids between the two compartments is constant. Fluid is classified by whether it’s inside or outside:
Intracellular fluid (ICF)—the fluid inside the cells, which is about 55% of the total body fluid
Extracellular fluid (ECF)—accounts for the rest of the body fluid.
ECF occurs in two forms: interstitial fluid (ISF) and intravascular fluid. ISF surrounds each cell of the body; even bone cells are bathed in it. Intravascular fluid is blood plasma, the liquid component of blood. It surrounds red blood cells and accounts for most of the blood volume.
In an adult, about 5% of body fluid is intravascular ECF; about 15% is interstitial ECF. Part of that interstitial ECF is transcellular fluid, which includes cerebrospinal fluid and lymph. Transcellular fluid contains secretions from the salivary glands, pancreas, liver, and sweat glands.
Maintaining fluid balance in the body involves the kidneys, heart, liver, adrenal and pituitary glands, and nervous system. This balancing act is affected by:
Fluid volume
Distribution of fluids in the body
Concentration of solutes in the fluid.
Remember, when it comes to body fluids, two i’s make an e. The two i’s (intravascular and interstitial fluid) are part of the e (extracellular fluid), not the i (intracellular fluid).
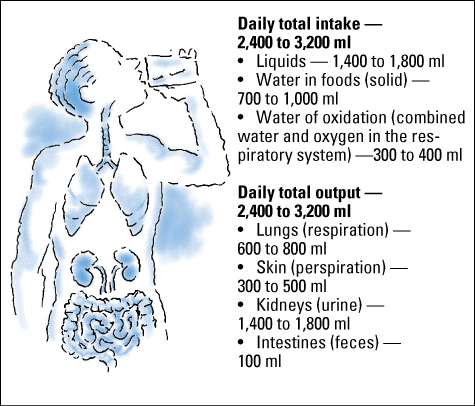
Every day, the body gains and loses fluid. To maintain fluid balance, the gains must equal the losses.
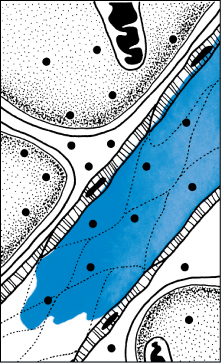
Each day the body gains and loses fluid through several different processes. This illustration shows the main sites involved. The amounts shown apply to adults; infants exchange a greater amount of fluid than adults.
Note: Gastric, intestinal, pancreatic, and biliary secretions total about 8,200 ml. However, because they’re almost completely reabsorbed, they aren’t usually counted in daily fluid gains and losses.
Fluid volume and concentration are regulated by the interaction of two hormones: antidiuretic hormone (ADH) and aldosterone. ADH, sometimes referred to as the water-conserving hormone, affects fluid volume and concentration by regulating water retention. It’s secreted when plasma osmolarity increases or circulating blood volume decreases and blood pressure drops. Aldosterone acts to retain sodium and water. It’s secreted when the serum sodium level is low, the potassium level is high, or the circulating volume of fluid decreases.
The thirst mechanism (awareness of the desire to drink) also regulates water volume and participates with hormones in maintaining fluid balance. Thirst is experienced when water loss equals 2% of body weight or when osmolarity (solute concentration) increases. Drinking water restores plasma volume and dilutes ECF osmolarity.
Nurses must anticipate changes in fluid balance that may take place during I.V. therapy. Therefore, it’s important to establish the patient’s baseline fluid status before starting fluid replacement therapy. During I.V. therapy, changes in fluid status alert the nurse to impending fluid imbalances.
Identifying fluid imbalancesBy carefully assessing a patient before and during I.V. therapy, you can identify fluid imbalances early—before serious complications develop. The following assessment findings and test results indicate fluid deficit or excess.
Fluid deficit
|
Fluid excess
|
Electrolytes are a major component of body fluid. There are six major electrolytes:
 Sodium
Sodium Potassium
Potassium Calcium
Calcium Chloride
Chloride Phosphorus
Phosphorus Magnesium.
Magnesium.As the name implies, electrolytes are associated with electricity. These vital substances are chemical compounds that dissociate in solution into electrically charged particles called ions. Like wiring for the body, the electrical charges of ions conduct current that’s necessary for normal cell function.
Six major electrolytes play important roles in maintaining chemical balance: sodium, potassium, calcium, chloride, phosphorus, and magnesium. Electrolyte concentrations are expressed in milliequivalents per liter (mEq/L) and milligrams per deciliter (mg/dl).
| |||||||||||||||||||||||||||||||||||||||
Fluids and electrolytes are usually discussed in tandem, especially where I.V. therapy is concerned, because fluid balance and electrolyte balance are interdependent. Any change in one alters the other, and any solution given I.V. can affect a patient’s fluid and electrolyte balance.
Not all electrolytes are distributed evenly. The major intracellular electrolytes are:
Potassium
Phosphorus.
The major extracellular electrolytes are:
Sodium
Chloride.
ICF and ECF contain different electrolytes because the cell membranes separating the two compartments have selective permeability—that is, only certain ions can cross those membranes. Although ICF and ECF contain different solutes, the concentration levels of the two fluids are about equal when balance is maintained.
The two ECF components—ISF and intravascular fluid (plasma)—have identical electrolyte compositions. Pores in the capillary walls allow electrolytes to move freely between the ISF and plasma, allowing for equal distribution of electrolytes in both substances.
The protein content of ISF and plasma differs, however. ISF doesn’t contain proteins because protein molecules are too large to pass through capillary walls. Plasma has a high concentration of proteins.
Fluid movement is another mechanism that regulates fluid and electrolyte balance.
Body fluids are in constant motion. Although separated by membranes, they continually move between the major fluid compartments. In addition to regulating fluid and electrolyte balance, this movement is how nutrients, waste products, and other substances get into and out of cells, organs, and systems.
Fluid movement is influenced by membrane permeability and colloid osmotic and hydrostatic pressures. Balance is maintained when solute and fluid molecules are distributed evenly on each side of the membrane. When this scale is tipped, these molecules are able to restore balance by crossing membranes as needed.
Solute and fluid molecules have several modes for moving through membranes. Solutes move between compartments mainly by:
Diffusion (passive transport)
Active transport.
Fluids (such as water) move between compartments by:
Osmosis
Capillary filtration and reabsorption.
Most solutes move by diffusion—that is, their molecules move from areas of higher concentration to areas of lower concentration. This change is referred to as “moving down the concentration gradient.” The result is an equal distribution of solute molecules. Because diffusion doesn’t require energy, it’s considered a form of passive transport.
By contrast, in active transport, molecules move from areas of lower concentration to areas of higher concentration. This change, referred to as “moving against the concentration gradient,” requires energy in the form of adenosine triphosphate.
In active transport, molecules are moved by physiologic pumps. You’re probably familiar with one active transport pump—the sodium-potassium pump. It moves sodium ions out of cells to the ECF and potassium ions into cells from the ECF. This pump balances sodium and potassium concentrations.
Fluids (particularly water) move by osmosis. Movement of water is caused by the existence of a concentration gradient. Water flows passively across the membrane from an area of higher water concentration to an area of lower water concentration. This dilution process stops when the solute concentrations on both sides of the membrane are equal.

Osmosis between the ECF and the ICF depends on the osmolarity (concentration) of the compartments. Normally, the osmotic (pulling) pressures of ECF and ICF are equal.
Osmosis can create a fluid imbalance between the ECF and ICF compartments, despite equal concentrations of solute, if the concentrations aren’t optimal. This imbalance can cause complications such as tissue edema.
Of all the vessels in the vascular system, only capillaries have walls thin enough to let solutes pass. Water and solutes move across capillary walls by two opposing processes:
 Capillary filtration
Capillary filtration Capillary reabsorption.
Capillary reabsorption.Filtration is the movement of substances from an area of high hydrostatic pressure to an area of lower hydrostatic pressure. (Hydrostatic pressure is the pressure at any level on water at rest due to the weight of water above it.) Capillary filtration forces fluid and solutes through capillary wall pores and into the ISF.
Left unchecked, capillary filtration would cause plasma to move in only one direction—out of the capillaries. This movement would cause severe hypovolemia and shock.
Fortunately, capillary reabsorption keeps capillary filtration in check. During filtration, albumin (a protein that can’t pass through capillary walls) remains behind in the diminishing volume of water. As the albumin concentration inside the capillaries increases, the albumin begins to draw water back in by osmosis. Water is thus reabsorbed by capillaries.
The osmotic, or pulling, force of albumin in capillary reabsorption is called colloid osmotic pressure or oncotic pressure. As long as capillary blood pressure exceeds colloid osmotic pressure, water and diffusible solutes can leave the capillaries and circulate into the ISF. When capillary blood pressure falls below colloid osmotic pressure, water and diffusible solutes return to the capillaries.
In any capillary, blood pressure normally exceeds colloid osmotic pressure up to the vessel’s midpoint, and then falls below colloid osmotic pressure along the rest of the vessel. That’s why capillary filtration takes place along the first half of a capillary and reabsorption occurs along the second half. As long as capillary blood pressure and plasma albumin levels remain normal, no net movement of water occurs. Water is equally lost and gained in this process.
The effect an I.V. solution has on fluid compartments depends on the solution’s osmolarity compared with serum osmolarity.
Osmolarity is the concentration of a solution. It’s expressed in milliosmoles of solute per liter of solution (mOsm/L). Normally, serum has the same osmolarity as other body fluids, about 300 mOsm/L. A lower serum osmolarity suggests fluid overload; a higher serum osmolarity suggests hemoconcentration and dehydration.
The doctor may order I.V. solutions to maintain or restore fluid balance. There are three basic types of I.V. solutions:
 Isotonic
Isotonic Hypotonic
Hypotonic Hypertonic.
Hypertonic.Solutions used for I.V. therapy may be isotonic, hypotonic, or hypertonic. The type you give a patient depends on whether you want to change or maintain his body fluid status.
| Isotonic solution
An isotonic solution has an osmolarity about equal to that of serum. Because it stays in the intravascular space, it expands the intravascular compartment. |
| Hypotonic solution
A hypotonic solution has an osmolarity lower than that of serum. It shifts fluid out of the intravascular compartment, hydrating the cells and the interstitial compartments. |
| Hypertonic solution
A hypertonic solution has an osmolarity higher than that of serum. It draws fluid into the intravascular compartment from the cells and the interstitial compartments. |
A few common solutions can be used to illustrate the role of I.V. therapy in restoring and maintaining fluid and electrolyte balance. A solution is isotonic if its osmolarity falls within (or near) the normal range for serum (240 to 340 mOsm/L). A hypotonic solution has a lower osmolarity; a hypertonic solution, a higher osmolarity. This chart lists common examples of the three types of I.V. solutions and provides key considerations for administering them.
|
An isotonic solution has the same osmolarity (or tonicity) as serum and other body fluids. Because the solution doesn’t alter serum osmolarity, it stays where it’s infused—inside the blood vessel (the intravascular compartment). The solution expands this compartment without pulling fluid from other compartments.
One indication for an isotonic solution is hypotension due to hypovolemia. Common isotonic solutions include lactated Ringer’s and normal saline.
A hypertonic solution has an osmolarity higher than serum osmolarity. When a patient receives a hypertonic I.V. solution, serum osmolarity initially increases, causing fluid to be pulled from the interstitial and intracellular compartments into the blood vessels.
Hypertonic solutions may be ordered for patients postoperatively because the shift of fluid into the blood vessels caused by a hypertonic solution has several beneficial effects for these patients. For example, it:
Reduces the risk of edema
Stabilizes blood pressure
Regulates urine output.
A hypotonic solution has an osmolarity lower than serum osmolarity. When a patient receives a hypotonic solution, fluid shifts out of the blood vessels and into the cells and interstitial spaces, where osmolarity is higher. A hypotonic solution hydrates cells while reducing fluid in the circulatory system.
Hypotonic solutions may be ordered when diuretic therapy dehydrates cells. Other indications include hyperglycemic conditions, such as diabetic ketoacidosis and hyperosmolar hyperglycemic nonketotic syndrome. In these conditions, high serum glucose levels draw fluid out of cells.
Because hypotonic solutions flood cells, certain patients shouldn’t receive them. For example, patients with cerebral edema or increased intracranial pressure shouldn’t receive hypotonic solutions because the increased ECF can cause further edema and tissue damage.
In addition to restoring and maintaining fluid and electrolyte balance, I.V. therapy is used to administer drugs, transfuse blood and blood products, and deliver parenteral nutrition.
The I.V. route provides a rapid, effective way of administering medications. Commonly infused drugs include antibiotics; thrombolytics; histamine-receptor antagonists; and antineoplastic, cardiovascular, and anticonvulsant drugs.
Drugs may be delivered long-term by continuous infusion, over a short period, or directly as a single dose.
Your nursing responsibilities may include giving blood and blood components and monitoring patients receiving transfusion therapy. Blood products can be given through a peripheral or central I.V. line. Various blood products are given to:
Restore and maintain adequate circulatory volume
Prevent cardiogenic shock
Increase the blood’s oxygen-carrying capacity
Maintain hemostasis.
Whole blood is composed of cellular elements and plasma. Cellular elements include:
Erythrocytes (red blood cells)
Leukocytes (white blood cells)
Thrombocytes (platelets).
Each of these elements is packaged separately for transfusion. Plasma may be delivered intact or separated into several components that may be given to correct various deficiencies. Whole blood transfusions are unnecessary unless the patient has lost massive quantities of blood (25% to 30%) in a short period.
Parenteral nutrition provides essential nutrients to the blood, organs, and cells by the I.V. route. It isn’t the same as a seven-course meal in a fine restaurant, but parenteral nutrition can contain the essence of a balanced diet.
Total parenteral nutrition (TPN) is customized for each patient. The ingredients in solutions developed for TPN are designed to meet a patient’s energy and nutrient requirements, including:
Proteins
Carbohydrates
Fats
Electrolytes
Vitamins
Trace elements
Water.

TPN should be used only when the gastrointestinal (GI) tract is unable to absorb nutrients. A patient can receive TPN indefinitely; however, long-term TPN can cause liver damage.
Peripheral parenteral nutrition (PPN) is delivered by peripheral veins. PPN is used in limited nutritional therapy. The solution contains fewer nonprotein calories and lower amino acid concentrations than TPN solutions. It may also include lipid emulsions. A patient can receive PPN for approximately 3 weeks. It can be used to support the nutritional status of a patient who doesn’t require total nutritional support. Complications associated with PPN include the risks of vein damage and infiltration.

When your patient is receiving parenteral nutrition, keep close track of changes in his fluid and electrolyte status and glucose levels. You’ll also need to assess your patient’s response to the nutrient solution to detect early signs of such complications as alterations in the pancreatic enzymes (lipase, amylase trypsin, and chymotrypsin), triglycerides, or albumin.
Depending in part on how concentrated an I.V. solution is, it may be delivered through a peripheral vein or a central vein. Usually, a low concentration solution is infused through a peripheral vein in the arm or hand; a more concentrated solution must be given through a central vein. Medications or fluids that may be administered centrally include:
Those with a pH less than 5 or greater than 9
Those with an osmolarity greater than 500 mOsm/L
Parenteral nutrition formulas containing more than 10% dextrose or more than 50% protein
Continuous vesicant chemotherapy (chemotherapy that’s toxic to tissues).
This illustration shows the veins commonly used for peripheral and central venous therapy.

There are three basic methods for delivering I.V. therapy:
 Continuous infusion
Continuous infusion Intermittent infusion
Intermittent infusion Direct injection.
Direct injection.Continuous I.V. therapy allows you to give a carefully regulated amount of fluid over a prolonged period. In intermittent I.V. therapy, a solution (commonly a medication) is given for shorter periods at set intervals. Direct injection (sometimes called I.V. push) is used to deliver a single dose (bolus) of a drug.
The choice of I.V. delivery method depends not only on the purpose and duration of therapy but also on the patient’s condition, age, and health history.

At times, a patient may receive I.V. therapy by more than one delivery method. Also, variations of each delivery method may be used. Some therapies also require extra equipment. For example, in some long-term chemotherapy, an implanted central venous access device is needed.
This chart lists the indications, advantages, and disadvantages of methods commonly used to administer I.V. medications.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
A continuous I.V. infusion helps maintain a constant therapeutic drug level. It’s also used to provide I.V. fluid therapy or parenteral nutrition.
Continuous I.V. infusion has its advantages. For example, less time is spent mixing solutions and hanging containers than with the intermittent method. You’ll also handle less tubing and access the patient’s I.V. device less often, decreasing the risk of infection.
Continuous administration has some disadvantages, too. For example, the patient may become distressed if the equipment hinders mobility and interferes with other activities of daily living. Also, the drip rate must be carefully monitored to ensure that the I.V. fluid and medication don’t infuse too rapidly or too slowly.
The most common and flexible method of administering I.V. medications is by intermittent infusion.
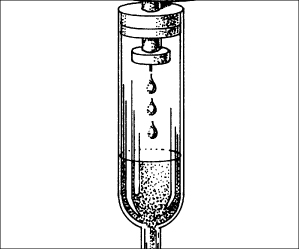
In intermittent infusion, drugs are administered over a specified period at varying intervals, thereby maintaining therapeutic blood levels. A small volume (1 to 250 ml) may be delivered over several minutes or a few hours, depending on the infusion prescription. You can deliver an intermittent infusion through a primary line (the most common method) or a secondary line. The secondary line is usually connected or piggybacked into the primary line by way of a Y-site (a Y-shaped section of tubing with a self-sealing access port).
You might say that I.V. therapy by direct injection gets right to the point. A vein can be accessed directly for a single dose of a prescribed drug or solution. The needle is then removed when the bolus is completed. A bolus injection may also be administered through an intermittent infusion device that’s already in place.
You need to choose the correct administration set for your patient’s infusion. Your choice depends on the type of infusion to be provided, the infusion container, and whether you’re using a volume-control device.
I.V. administration sets come in two forms: vented and unvented. The vented set is for containers that have no venting system (I.V. plastic bags and some bottles). Unvented bottles have their own venting system.
I.V. administration sets come with various other features as well, including ports for infusing secondary medications and filters for blocking microbes, irritants, or large particles. The tubing also varies. Some types are designed to enhance the proper functioning of devices that help regulate the infusion rate. Other tubing is used specifically for continuous or intermittent infusion or for infusing parenteral nutrition and blood.
A key aspect of administering I.V. therapy is maintaining accurate infusion rates for the solutions. If an infusion runs too fast or too slow, your patient may suffer complications, such as phlebitis, infiltration, circulatory overload (possibly leading to heart failure and pulmonary edema), and adverse drug reactions.
Volume-control devices and the correct administration set help prevent such complications. You can help, too, by being familiar with all of the information in doctors’ orders and being able to recognize incomplete or incorrectly written orders for I.V. therapy.
Reading an I.V. orderOrders for I.V. therapy may be standardized for different illnesses and therapies or individualized for a particular patient. Some facility policies dictate an automatic stop order for I.V. fluids. For example, I.V. orders are good for 24 hours from the time they’re written, unless otherwise specified.
| It’s complete A complete order for I.V. therapy should specify:
|
| When it isn’t complete If you find that an order isn’t complete or if you think an I.V. order is inappropriate because of the patient’s condition, consult the doctor. |
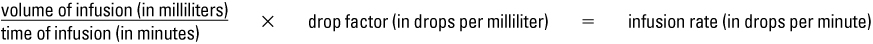
There are two basic types of infusion rates available with I.V. administration sets: macrodrip and microdrip. Each set delivers a specific number of drops per milliliter (gtt/ml). Macrodrip delivers 10, 15, or 20 gtt/ml; microdrip delivers 60 gtt/ml. Regardless of the type of set you use, the formula for calculating infusion rates is the same.
Calculating infusion ratesWhen calculating the infusion rate (drops per minute) of I.V. solutions, remember that the number of drops required to deliver 1 ml varies with the type of administration set used and its manufacturer:
Administration sets are of two types—macrodrip (the standard type) and microdrip. Macrodrip delivers 10, 15, or 20 gtt/ml; microdrip usually delivers 60 gtt/ml .
Manufacturers calibrate their devices differently, so be sure to look for the “drop factor”—expressed in drops per milliliter or gtt/ml—in the packaging that accompanies the set you’re using. (This packaging also has crucial information about such things as special infusions and blood transfusions.) When you know your device’s drop factor, use the following formula to calculate specific infusion rates:
After you calculate the infusion rate for the set you’re using, remove your watch or position your wrist so you can look at your watch and the drops at the same time. Next, adjust the clamp to achieve the ordered infusion rate and count the drops for 1 full minute. Readjust the clamp as necessary and count the drops for another minute. Keep adjusting the clamp and counting the drops until you have the correct rate.
| Macrodrip
|
| Microdrip
|

When a patient’s condition requires you to maintain precise I.V. infusion rates, use an infusion control device, such as:
Clamps
Volumetric pumps.
When you regulate the I.V. infusion rate with a clamp, the rate is usually measured in drops per minute (gtt/minute). If you use a pump, the infusion rate is measured in milliliters per hour (ml/hour).
You can regulate the infusion rate with two types of clamps: screw and roller. The screw clamp offers greater accuracy, but the roller clamp, used for standard fluid therapy, is faster and easier to manipulate. A third type, the slide clamp, can stop or start the infusion but can’t regulate the rate.
New pumps are being developed all the time; be sure to attend instruction sessions to learn how to use them. On your unit, keep a file of instruction manuals (provided by the manufacturers) for each piece of equipment used.
When you’re using a clamp for infusion regulation, you must monitor the infusion rate closely and adjust as needed. Such factors as vein spasm, vein pressure changes, patient movement, manipulations of the clamp, and bent or kinked tubing can cause the rate to vary markedly. For easy monitoring, use a time tape, which marks the prescribed solution level at hourly intervals.
Here’s a simple way to monitor I.V. infusion rate: Attach a piece of tape or a preprinted strip to the I.V. container; then write hourly times on the tape or strip beginning with the time you hung the solution.
By comparing the actual time with the label time, you can quickly see if the rate needs to be adjusted. Remember that you should never increase I.V. infusion rates by more than 30% unless you first check with the doctor.

Other factors that affect infusion rate include the type of I.V. fluid and its viscosity, the height of the infusion container, the type of administration set, and the size and position of the venous access device.
Infusion rates can be fickle; you must check and adjust them regularly. The frequency with which you should check infusion rates depends on the patient’s condition and age and the solution or medication being administered.

Many nurses check the I.V. infusion rate every time they’re in a patient’s room and after each position change. Assess the infusion rate more frequently for some patients, such as:
Critically ill patients
Patients with conditions that might be exacerbated by fluid overload
Pediatric patients
Elderly patients
Patients receiving a drug that can cause tissue damage if infiltration occurs.
When checking the infusion rate, inspect and palpate the I.V. insertion site, and ask the patient how it feels.
If the infusion rate slows significantly, you can usually get it back on schedule by adjusting the rate slightly. Don’t make a major adjustment, though. If the rate must be increased by more than 30%, check with the doctor.
You should also time an infusion control device or rate minder for 1 to 2 hours per shift. (These devices have an error rate ranging from 2% to 10%.) Before using any infusion control device, become thoroughly familiar with its features. Attend instruction sessions and perform return demonstrations until you learn the system.
Administering drugs and solutions to patients is one of the most legally significant tasks nurses perform. Unfortunately, the number of lawsuits directed against nurses who are involved in I.V. therapy is increasing. For example, a 1995 Missouri study reported a high incidence of errors involving I.V. solution administration in which wrong solutions were used or solutions were administered by an incorrect route. Many lawsuits centered on errors in infusion pump use.
Lawsuits may also result from administration of the wrong medication dosage, inappropriate placement of an I.V. line, and failure to monitor for adverse reactions, infiltration, dislodgment of I.V. equipment, or other mishaps.

Here are some examples of lawsuits involving I.V. therapy.
In Los Angeles, a nurse administered midazolam (Versed) through a port in an I.V. line to an infant, leading to the infant’s death. This nurse had never administered I.V. Versed to an infant or child before. A facility protocol prohibited the use of Versed on the pediatric floor. The manufacturer recommended a dosage of 0.1 mg/kg, and the infant weighed 9 kg. The hospital record indicated 5 mg had been administered. A settlement awarded the plaintiff $225,000.
In another Los Angeles case, continuous infusion of 145 mg of morphine over 18 hours led to a patient’s death. The doctor failed to limit the amount to be infused. Nevertheless, the charge nurse and staff nurse were held accountable for failing to recognize a “gross overdose.” The patient’s widow and children were awarded more than $2 million for lost wages and general damages.
In Illinois, a nurse administered the wrong dose of lidocaine (Xylocaine). The order was for 100 mg; the nurse injected 2 g. The packaging caused confusion: the Xylocaine was provided in a 2-g syringe for mixing into an I.V. solution and in a 100-mg syringe for direct injection. The nurse accidentally used the 2-g syringe. However, information about previous overdose incidents from the Food and Drug Administration and medical literature had been available to the hospital.
In Ohio, a nurse failed to clamp a pump regulating the flow of an antibiotic through a central line to a child. This resulted in delivery of nearly seven times the prescribed dosage of gentamicin, causing the child to become totally deaf.
In Pennsylvania, an emergency department nurse misplaced an I.V. line, which infiltrated the patient’s hand, resulting in reflex sympathetic dystrophy. The patient couldn’t return to work and won a $702,000 award.
Several recent lawsuits have involved allegations that a nurse struck a patient’s radial nerve during insertion of an I.V. line. Such injuries can cause compartment syndrome and may require emergency fasciotomy, skin grafts, and other surgery. Uncorrected compartment syndrome can progress to gangrene and amputation of fingers. One New York case involving finger amputation resulted in a $40 million jury verdict, which was later reduced to $5 million.
When monitoring an I.V. line, listening to the patient is as important as monitoring the site, pump, and tubing. In the Tampa, Florida, case of Frank v. Hillsborough County Hospital, a patient’s frequent complaints of pain were ignored. The patient suffered permanent nerve damage and later obtained an award of almost $60,000.
As a nurse, you have a legal and ethical responsibility to your patients. The good news is that if you honor these duties and meet the appropriate standards of care, you’ll be able to hold your own in court.
By becoming aware of professional standards and laws related to administering I.V. therapy, you can provide the best care for your patients and protect yourself legally. Professional and legal standards are defined by state nurse practice acts, federal regulations, and facility policies.

Each state has a nurse practice act that broadly defines the legal scope of nursing practice. Your state’s nurse practice act is the most important law affecting your nursing practice.
Every nurse is expected to care for patients within defined limits. If a nurse gives care beyond those limits, she becomes vulnerable to charges of violating her state nurse practice act. For a copy of your state nurse practice act, contact your state nurse’s association or your state board of nursing or its Web site.
Many states’ nurse practice acts don’t specifically address scope of practice regarding I.V. therapy by registered nurses (RNs). However, many nurse practice acts do address whether licensed practical nurses (LPNs) or licensed vocational nurses (LVNs) can administer I.V. therapy. It’s important for LPNs and LVNs as well as for the RNs who are supervising or training them to be familiar with this information.

The federal government issues regulations and establishes policies related to I.V. therapy administration. For example, it mandates adherence to standards of I.V. therapy practice for health care facilities so that they can be eligible to receive reimbursement under Medicare, Medicaid, and other programs.
Medicare and Medicaid, the two major federal health care programs, serve about 75 million Americans. They’re run by the Health Care Financing Administration (HCFA), which is part of the U.S. Department of Health and Human Services. HCFA formulates national Medicare policy, including policies related to I.V. therapy, but contracts with private insurance companies to oversee claims and make payment for services and supplies provided under Medicare. These agencies, in turn, enforce HCFA policy by accepting or denying claims for reimbursement. When reviewing claims, agencies may evaluate practices and quality of care—an important factor underlying the emphasis on proper documentation in health care.

Medicaid, which serves certain low-income people, is a state-federal partnership administered by a state agency. There are broad federal requirements for Medicaid, but states have a wide degree of flexibility to design their own programs.
To be eligible for reimbursement, health care agencies must comply with the standards of a complex network of regulators. Consider, for example, a patient receiving I.V. medications at home with a reusable pump. This patient is primarily covered by Medicare with secondary Medicaid coverage. A variety of carriers, fiscal intermediaries, and agencies share responsibility for reimbursement and regulatory oversight of the patient’s care:
An insurance carrier contracts with Medicare to cover services such as refilling the pump.
A separate insurance carrier (a durable medical equipment carrier designated by HCFA) covers administered drugs, the pump, and pump supplies.
Another insurance carrier (called a fiscal intermediary) contracts with Medicare to cover preliminary in-hospital training of the patient in I.V. therapy techniques.
A Medicaid agency also covers a portion of the patient’s care.
Nursing documentation must be complete to meet the requirements of all these different agencies. The underlying (though unstated) philosophy of these agencies is that “if it isn’t documented, it isn’t done.” The regulatory network is becoming more complicated as many Medicare and Medicaid patients are being covered by managed care organizations that have their own rules and procedures.
Every health care facility has I.V. therapy policies for nurses. Such policies are required to obtain accreditation from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) and other accrediting bodies. These policies can’t go beyond what a state’s nurse practice act permits, but they more specifically define your duties and responsibilities.
Awareness of facility policy is particularly important in rapidly developing areas of practice such as home care, where the intensity of service and patient needs is increasing dramatically. For example, home health nurses must be acutely aware of patient and family education policies because infusion systems are being used in the home 24 hours per day without the presence of full-time nursing staff.

The Infusion Nurses Society (INS) has developed a set of standards, the Infusion Nursing Standards of Practice, that are commonly used by committees developing facility policy. According to the INS, the goals of these standards are to “protect and preserve the patient’s right to safe, quality care and protect the nurse who administers infusion therapy.” These standards address all aspects of I.V. nursing. For more information, contact the INS at (781) 440-9408 or at http://www.ins1.org.
You must document I.V. therapy for several reasons. Proper documentation provides:
Accurate description of care that can serve as legal protection (e.g., as evidence that a prescribed treatment was administered)
Mechanism for recording and retrieving information
Record for health care insurers of equipment and supplies used.

When you initiate I.V. therapy, it’s important to include specific information about where the I.V. was started, what kind of equipment was used, and what solution was infused.
Follow these tips to document your care when you perform I.V. site care or catheter removal or when you document I.V. infusion using a sequential system or on a flow sheet or an intake and output sheet.
| I.V. site care When you perform I.V. site care, document the following:
If complications are present, document:
|
| I.V. catheter removal When an I.V. catheter is removed, document the following:
|
| Sequential system One way to document I.V. solutions throughout therapy is to number each container sequentially. For example, if a patient is to receive normal saline solution at 125 ml/hour (3,000 ml/day) on day 1, number the 1,000-ml containers as 1, 2, and 3. If another 3,000 ml is ordered on day 2, number those containers as 4, 5, and 6. This system may reduce administration errors. Also, check your facility’s policy and procedures; some facilities require beginning the count again if the type of fluid changes, whereas others keep the count sequential regardless of the type of fluid. |
| Flow sheets Flow sheets highlight specific patient information according to preestablished parameters of nursing care. They have spaces for recording dates, times, and specific interventions. When you use an I.V. flow sheet, record:
|
| Intake and output sheets When you’re documenting I.V. therapy on an intake and output sheet, follow these guidelines:
|
I.V. therapy may be documented on progress notes, a sequential system, a special I.V. therapy sheet or flow sheet, a nursing care plan on the patient’s chart, or an intake and output sheet.
In addition to documentation in the patient’s chart, you need to label the dressing on the catheter insertion site. Whenever you change the dressing, label the new one.
| How to label a dressing To label a new dressing over an I.V. site, include:
|
You should also label the fluid container and place a time tape on it. With a child, you may need to label the volume-control set as well. In labeling the container and the set, follow your facility’s policy and procedures.
| How to label an I.V. bag When you place a label on an I.V. bag, be sure not to cover the name of the I.V. solution. To properly label an I.V. solution container, include (in addition to the time tape):
|
It’s equally important to document how the I.V site is maintained, including the conditions of the site; care that was provided; dressing, solution, tubing, or equipment changes you made; and teaching you provided.
Although you may be accustomed to I.V. therapy, many patients aren’t. Your patient may be apprehensive about the procedure and concerned that his condition has worsened.
Teaching the patient and, when appropriate, members of his family will help him relax and take the mystery out of I.V. therapy.
| Based on past experience Begin by determining your patient’s previous infusion experience, expectations, and knowledge of venipuncture and I.V. therapy. Then base your teaching on your findings. Your teaching should include these steps:
|
| The whole story Give the patient as much information as possible. Consider providing pamphlets, sample catheters and I.V. equipment, slides, videotapes, and other appropriate information. Make sure you tell the whole story:
|
| Easing anxiety Give the patient time to express concerns and fears, and take the time to provide reassurance. Also, encourage the patient to use stress-reduction techniques such as deep, slow breathing. Allow the patient and their family to participate in the patient’s care as much as possible. |
| But did they get it? Make sure you evaluate how well your patient and members of the patient’s family understand your instruction. Evaluate their understanding while you’re teaching and when you’re done. You can do this by asking frequent questions and having them explain or demonstrate what you have taught. |
| Don’t forget the paperwork Document all your teaching in the patient’s records. Note what you taught and how well the patient understood it. |

References
Berman, A., & Snyder, S. J. (2012). Skills in clinical nursing (7th ed.). Upper Saddle River, NJ: Pearson Education.
Berman, A., Snyder, S. J., & McKinney, D. S. (2011). Nursing basics for clinical practice. Upper Saddle River, NJ: Pearson Education.
Treas, L. S., & Wilkinson, J. M. (2014). Basic nursing concepts, skills & reasoning. Philadelphia, PA: F. A. Davis.
![]()
- The fluid located inside the cell is called:
- The major extracellular electrolytes are:
- An example of a hypertonic solution is:
- When capillary blood pressure exceeds colloid osmotic pressure, which situation occurs?
 If you answered all four questions correctly, super! Your knowledge of I.V. therapy is diffuse.
If you answered all four questions correctly, super! Your knowledge of I.V. therapy is diffuse. If you answered three questions correctly, bravo! You’re no drip when it comes to I.V. therapy.
If you answered three questions correctly, bravo! You’re no drip when it comes to I.V. therapy. If you answered fewer than three questions correctly, don’t despair! Review the chapter for an infusion of I.V. know-how and try again.
If you answered fewer than three questions correctly, don’t despair! Review the chapter for an infusion of I.V. know-how and try again.Outline