| Skill 3-1 | Performing a General Survey | ||||||||||||||||||||||||||||||
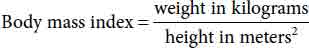
The general survey is the first component of the physical assessment, beginning with the first moment of patient contact and continuing throughout the nurse-patient relationship. The general survey helps to develop an overall impression of the patient. It includes observing the patient's overall appearance and behavior; taking vital signs; measuring height, weight, and waist circumference; head circumference (infants and children) and calculating the body mass index (BMI). BMI and waist circumference are indicators of risk for developing obesity-associated diseases or conditions, such as cardiovascular disease, high blood pressure, and type 2 diabetes (National Heart, Lung, and Blood Institute, n.d.). Delegation Considerations Measurement of the patient's weight and height, and vital signs may be delegated to assistive personnel (AP). Depending on the state's nurse practice act and the organization's policies and procedures, the licensed practical/vocational nurses (LPN/LVNs) may perform some or all the parts of the general survey. The decision to delegate must be based on careful analysis of the patient's needs and circumstances as well as the qualifications of the person to whom the task is being delegated. Refer to the Delegation Guidelines in Appendix A. Assessment Develop an overall impression of the patient, focusing on appearance and behavior, vital signs, height, and weight. Ask the patient about any changes in weight, pain or discomfort, sleeping patterns, and any difficulty sleeping. Actual or Potential Health Problems and Needs Many actual or potential health problems or needs may require the use of this skill as part of related interventions. An appropriate health problem or need may include: Outcome Identification and Planning The expected outcome to achieve in performing a general survey is that the assessment is completed without the patient experiencing anxiety or discomfort, an overall impression of the patient is formulated, the findings are documented, and the appropriate referral is made to other health care professionals, as needed, for further evaluation. Other outcomes may be appropriate, depending on the specific diagnosis or patient problem identified for the patient. Implementation
Evaluation The expected outcomes have been met when the assessment has been completed without the patient experiencing anxiety or discomfort; an overall impression of the patient has been formulated; the findings have been documented; and the appropriate referrals have been made to other health care professionals, as needed, for further evaluation. Documentation Guidelines Document findings related to assessment of the patient's physical appearance, body structure, mobility, and behavior. Document the patient's height, weight, BMI, and waist circumference. Document the presence or absence of pain as well as an initial pain assessment if present. Record the patient's temperature (T), pulse (P), respiration (R), and blood pressure (BP) measurements as well as the oxygen saturation measurement. Note any referrals. Sample Documentation
1/26/25 1015 Patient admitted to room 432. Patient is a 23-year-old Asian female graduate student at a local university, living in an apartment with three other female students. Appears well nourished, disheveled, clothing appropriate for age and season, and tired. Oriented, cooperative, with no signs of acute distress; patient denies pain at present. T 98.9°F, P 78, R 16, BP 114/58 mm Hg (left arm), sitting O2 sat 96% on room air. Height 144 cm (5 ft). Weight 55 kg (121 lb). BMI 26.5. Waist circumference 32 inches. Information provided regarding use of call bell, lights, and phone, and location of bathroom. Patient verbalizes an understanding of information.Developing Clinical Reasoning and Clinical Judgment Unexpected Situations and Associated Interventions
Special Considerations General Considerations
Infant and Child Considerations
| |||||||||||||||||||||||||||||||