Bone and Soft-Tissue Disorders
Pathogenesis: (controversial)
- Extrinsic theory (Neer):
- hypertrophic changes of acromion
- osteophytes from acromioclavicular joint
- Type 3 hooked acromion
→ impingement of subacromial-subdeltoid bursa and rotator cuff
- Intrinsic (intratendinous) theory: tendon degeneration → partial-thickness tear → superior migration of humeral head → abrasion of rotator cuff against undersurface of acromion → full-thickness tear
- Impingement syndrome
- Rotator cuff tendinitis
- Degeneration without impingement
- Shoulder instability with secondary impingement
- Instability without impingement
= clinical NOT radiographic diagnosis consisting of lateral shoulder pain with abduction and forward flexion
Cause: inadequate space for the normal motion of rotator cuff
Age: lifelong process; 1st stage <25 years; 2nd stage 25–40 years; complete rotator cuff tear >40 years
Pathophysiology:
movement of humerus impinges rotator cuff tendons against coracoacromial arch resulting in microtrauma, which causes inflammation of subacromial bursa (= fibrous thickening of subacromial bursa) / rotator cuff (critical zone of rotator cuff = supraspinatus tendon 2 cm from its attachment to humerus)
Impingement anatomy:
narrowing of subacromial space secondary to
- Acquired
- degenerative subacromial enthesophyte / osteophyte
- traction enthesophyte at coracoacromial ligament (= subacromial spur)
- osteophytes ← acromioclavicular joint hypertrophy in osteoarthrosis
- hypertrophy of coracoacromial ligament
- primary bursitis in rheumatoid arthritis
- swollen supraspinatus tendon ± calcific tendinosis impinging upon coracoacromial arch
- degenerative subacromial enthesophyte / osteophyte
- Congenital
- curvature of acromion in anterior third (SAG)
- flat (type 1)
- curved downward (type 2)
- hooked downward (type 3)
- curved upward (type 4)
- Type 3 and possibly type 2 acromion processes have a higher prevalence of bursal-side rotator cuff tears!
- lateral acromial angle (COR)
- downsloping of acromion in lateral direction
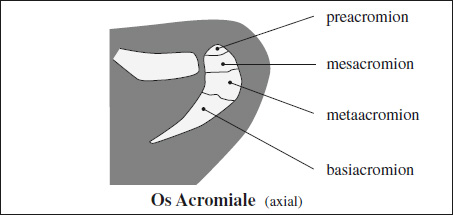
- os acromiale = unfused acromial apophysis (8% of population)
- curvature of acromion in anterior third (SAG)
◊Impingement syndrome may exist without impingement anatomy and may be secondary to primary instability!
- night pain
- passive elevation of arm to 170° followed by passive internal + external rotation while arm adducted against ear → increased pain with rotation = test positive
- “arc of pain” sign = pain during active descent of abducted arm in abduction plane → minimal pain at full elevation with maximal pain between 70° and 120° = test positive
X-ray (AP view):
- inferolateral tilt of acromion (on AP view)
X-ray (supraspinatus outlet [modified Y] view + caudal tilt view):
- type III acromion = anterior aspect of acromion hooked inferiorly
- anterior tilt / low position of acromion
- anterior subacromial spur on undersurface of AC joint (= enthesophyte) at insertion site of coracoacromial lig.
MR (can identify the anatomy predisposing to impingement):
- unstable os acriomale pulled downward by deltoid muscle during abduction
- thickening of coracoacromial ligament
- acromioclavicular joint osteoarthritis ± bone spurs
US:
- bunching of subdeltoid bursa during abduction of arm
- US can direct steroid injection into bursa
Cx:
- partial / complete tear (may be precipitated by acute traumatic event on preexisting degenerative changes; common cause of rotator cuff tears)
- cuff tendinitis / degenerative tendinosis
Dx: Lidocaine impingement test (= subacromial lidocaine injection relieves pain)
Rx: acromioplasty (= removal of a portion of the acromion), removal of subacromial osteophytes, removal / lysis / débridement of coracoacromial ligament, resection of distal clavicle, removal of acromioclavicular joint osteophytes
Internal Impingement
- humeral head cysts / defects
- undersurface degeneration + tearing of posterior supraspinatus and anterior infraspinatus tendons
- posterosuperior labral tear
- posterosuperior glenoid chondral lesion + cyst
Anterosuperior Impingement
= intraarticular impingement = pulley lesions (Habermeyer classification)
- Group 1 lesion
= isolated superior GHL lesions - Group 2 lesion
= superior GHL lesion + partial articular-side supraspinatus tendon tear - Group 3 lesion
= superior GHL lesion + partial articular-side subscapularis tendon tear - Group 4 lesion
= superior GHL lesions + partial articular-side tears of supraspinatus and subscapularis tendons
Glenohumeral stability is dependent on a functional anatomic unit (= anterior capsular mechanism) formed by: glenoid labrum, joint capsule, superior + middle + inferior (anterior + posterior parts) glenohumeral ligaments, coracohumeral ligament, subscapularis tendon, rotator cuff
Age:<35 years
Frequency: acute, recurrent, fixed
Cause: traumatic, microtraumatic, atraumatic
Direction: anterior >multidirectional >inferior >posterior
Type of lesions: labral abnormalities (compression, avulsion, shearing), capsular / ligamentous tear / avulsion
Associated osseous lesions:
Hill-Sachs defect, glenoid rim fracture, trough line fracture
Associated soft-tissue lesions:
Bankart lesion, GLAD, Perthes, ALPSA, HAGL, labral cyst
- Normal clefts may exist within labrum!
False positive for labral separation:
- Articular cartilage deep to labrum
- Glenohumeral ligaments passing adjacent to labrum
Etiology:
- Attritional change ← repetitive microtrauma = overuse of shoulder from professional / athletic activities
- Subacromial impingement between humeral head + coracoacromial arch
- Tendon degeneration ← hypovascularity ← aging
- Acute trauma (rare)
Prevalence in asymptomatic patients:
in 40% of patients >50 years (full-thickness tear); in >60% of patients >60 years (partial & full thickness)
Age: most commonly >50 years; young athletic patient may have “rim-rent” tear (= avulsion of attachment at greater tuberosity
Location:
Supraspinatus tendon tear:
- “critical zone” of anterior supraspinatus tendon 1 cm medial to attachment (= area of relative hypovascularity)
Infraspinatus tendon tear (30–40%):
- precludes arthroscopic repair
- worst postoperative prognosis
- isolated tear more common in throwing sports
Teres minor tendon tear (rare):
- also affected by posterior instability
Subscapularis tendon tear:
- more common in superior articular surface
- associated with supraspinatus tendon tear + rotator interval lesion + biceps tendon pathology
- cysts of lesser tuberosity + edema (common)
- clinical assessment (during US):
- test of supraspinatus m.
- supraspinatus weakness
- straight hanging and 20° abducted arm pushed against applied force = assessment of strength
- impingement: 97% sensitive + 67% PPV
- “arc of pain”: 98% sensitive + 67% PPV
- weakness of abduction: 64% sensitive + 78% PPV
- drop-arm test = active abduction of arm to 90° then slowly lowering arm: if arm drops abruptly test is positive (98% specific, 10% sensitive)
- combination of (a) + (b) + (c) = 98% chance of rotator cuff tear
- supraspinatus weakness
- test of infraspinatus m. + teres minor m.
- weakness of external rotation: 76% sensitive + 79% PPV
- resist inward force with elbow flexed 90° + shoulder internally rotated
- weakness of external rotation: 76% sensitive + 79% PPV
- test of subscapularis m.
- passive positioning of arm behind back with palm facing outward: failure to hold forearm + hand off the back = positive test
- patient age
- night pain: 88% sensitive + 70% PPV
- test of supraspinatus m.
Assessment:
- Depth of tear
- incomplete rupture = partial-thickness tear involves either bursal or synovial surface or remains intratendinous
- Articular-surface partial-thickness tear >>bursal-surface partial thickness tear
- PASTA = partial thickness articular supraspinatus tendon avulsion (at attachment of tendon to greater tuberosity = footprint)
- PAINT = partial articular tear with intratendinous extension
- fluid-filled defect not extending across the entire tendon width
- disruption of superior / inferior tendon fibers only
- complete rupture = full-thickness tear from subacromial bursal surface to articular surface of glenohumeral joint
- pure transverse tear
- pure vertical / longitudinal tear
- tear with retraction of tendon edges
- global tear = massive tear / avulsion of cuff involving more than one of the tendons
- incomplete rupture = partial-thickness tear involves either bursal or synovial surface or remains intratendinous
- Size of tear
Depth of partial tear (normal thickness = 12 mm):- small = grade 1 (<25%) = <3 mm
- medium = grade 2 (25–50%) = 3–6 mm
- large = grade 3 (>50%) = >6 mm
Greatest dimension of full-thickness tear:- small = <1 cm
- medium = 1–3 cm
- large = 3–5 cm
- massive = >5 cm
- Geometry of tear (as viewed from tendon surface)
- crescentic = minimal retraction of tendon
- U-shaped = massive tear that may extend to level of glenoid fossa
- L-shaped = massive tear with longitudinal component
- Injury extension (to adjacent structures)
- in anterior direction: supraspinatus tendon → medial aspect of coracohumeral ligament (rotator interval) → superior subscapularis tendon fibers
- in posterior direction: supraspinatus tendon → infraspinatus tendon → teres minor tendon
- involvement of long head of biceps brachii tendon
- Injury / disruption of LHBB tendon in up to 77%
- Subluxation / dislocation in up to 44%
- Muscle atrophy (decreased bulk, fatty infiltration) as strongest prognosticator of surgical outcome
- Muscle cross-sectional area measurement correlates with muscle strength!
- on SAG OBL plane at level of medial coracoid process:
- “tangent” sign = supraspinatus muscle does not cross a line drawn through superior border of scapular spine + superior margin of coracoid process
- scapular ratio of <50% = occupation ratio of cross-sectional area of supraspinatus m. to area of supraspinatus fossa
- Impingement anatomy
X-ray (AP view):
- usually normal in acute rotator cuff tear
- acromiohumeral distance ≤2 mm (with active abduction to 90°) ← absence / retraction of supraspinatus tendon
- flattened / ill-defined superior soft-tissue contour with heterogeneous decreased density → fatty replacement (on supraspinatus outlet [modified Y] view)
X-ray (late findings):
- superior migration of humeral head = acromiohumeral distance <7 mm
- cuff arthropathy = sclerosis, subchondral cysts, osteolysis, notching / pitting of greater tuberosity ← repetitive contact between humeral head + acromion
- remodeling of acromial undersurface with matching sclerosis, faceting, concavity of inferolateral aspect of acromion
US (scans in hyperextended position, 75–100% sensitive, 43–97% specific, 65–95% NPV, 55–75% PPV):
Sequence of examination:
biceps, subscapularis, supraspinatus, infraspinatus, teres minor, posterior glenohumeral joint
- direct primary signs of tendon tear
- focal absence of rotator cuff= partial thickness:
- well-defined hypo- / anechoic defect in tendon replaced by fluid → with extension either to bursal /or articular surface
- abrupt + sharply demarcated focal thinning
- small comma-shaped area of hyperechogenicity (= small tear filled with granulation tissue / hypertrophied synovium)
- nonvisualization of retracted tendon in massive supraspinatus tear (most reliable sign):
- discontinuity of rotator cuff filled with joint fluid
- defect filled with hypoechoic thickened bursa + peribursal fat
- “naked tuberosity” sign = retracted tendon leaves a bare area of bone
- deltoid muscle directly on top of humeral head
- hypervascularity of defect on color Doppler
- focal absence of rotator cuff= partial thickness:
- indirect primary signs of tendon tear
- “double cortex” / “cartilage interface” sign = 2 hyperechoic lines representing cartilage + cortex ← fluid-enhanced increase in through-transmission
- compressibility = loss of normal convex contour of peribursal fat ← displacement of fluid with compression by transducer over hypoechoic defect
- “sagging peribursal fat” sign = depression of hyperechoic peribursal fat into area of torn tendon
- increased echogenicity + decreased bulk of muscle = muscle atrophy (in 77% of rotator cuff tears)
- secondary signs of tendon tear:
- cortical irregularity of greater tuberosity
- shoulder joint effusion = anechoic fluid in axillary pouch, posterior recess, biceps tendon sheath
False negative: longitudinal tear, partial tear
False positive: intraarticular biceps tendon, soft-tissue calcification, small scar / fibrous tissue
Arthrography (71–100% sensitive, 71–100% specific for combined full + partial thickness tears):
- opacification of subacromial-subdeltoid bursa
- contrast enters substance of rotator cuff tendons
MR (41–100% sensitive and 79–100% specific for combined full + partial thickness tears):
- discontinuity of cuff with retraction of musculotendinous junction
- focal / generalized intense / markedly increased SI on T2WI (= fluid within cuff defect) in <50%
- fluid within subacromial-subdeltoid bursa (most sensitive)
- low / moderate SI on T2WI (= severely degenerated tendon, intact bursal / synovial surface, granulation / scar tissue filling the region of torn tendinous fibers)
- cuff defect with contour irregularity
- abrupt change in signal character at boundary of lesion
- supraspinatus muscle atrophy (MOST SPECIFIC)
Pitfalls:
- hyperintense focus in distal supraspinatus tendon
- gray signal isointense to muscle on all pulse sequences:
- partial volume averaging with superior + lateral infraspinatus tendon
- vascular “watershed” area
- magic angle effect = orientation of collagen fibers at 55° relative to main magnetic field
- hyperintense focus within rotator cuff on T2WI:
- partial volume averaging with fluid in biceps tendon sheath / subscapularis bursa
- partial volume averaging with fat of peribursal fat
- motion artifacts: respiration, vascular pulsation, patient movement
- fatty atrophy of muscle
- impingement of axillary / suprascapular nn. = quadrilateral space syndrome
DDx:
- Partial-thickness tear with diffuse less-than-fluid intensity on T2WI
- Tendon degeneration (tendinopathy)
- Tendinitis
- Full-thickness tear containing granulation tissue
Subacromial-Subdeltoid Bursitis
common finding in rotator cuff tears
- peribursal fat totally / partially obliterated + replaced by low-signal-intensity tissue on all pulse sequences
- fluid accumulation within bursa
Supraspinatus Tendinopathy / Tendinosis
= chronic tendon degeneration with disorganized repair
Cause: impingement, acute / chronic stress
Histo: mucinous + myxoid degeneration
- increase in tendon SI on proton-density images without disruption of tendon
- tendinous enlargement + inhomogeneous signal pattern
- fibers on superior + inferior tendon surface remain visible and contiguous
Cx: main risk factor for subsequent rotator cuff tear (not impingement)
DDx: supraspinatus tear (tendon has fluid intensity)