- Therapeutic decision-making should be based on clinical assessment alone!
- There are no prognostic indicators on images in patients with acute lumbar radiculopathy!
- 35% of individuals without back trouble have abnormal findings (HNP, disk bulging, facet degeneration, spinal stenosis)
- Imaging is only justified in patients for whom surgery is considered!
Pathophysiology:
- loss of disk height leads to stress on facet joints + uncovertebral joints (= uncinate process), exaggerated joint motion with misalignment (= rostrocaudal subluxation) of facet joints, spine instability with arthritis, capsular hypertrophy, hypertrophy of posterior ligaments, facet fracture
Plain film:
- intervertebral osteochondrosis = disease of nucleus pulposus (= desiccation = loss of disk water):
- narrowing of disk space
- vacuum disk phenomenon
- disk calcification
- bone sclerosis of adjacent vertebral bodies
- spondylosis deformans = degeneration of the outer fibers of the annulus fibrosus:
- endplate osteophytosis growing initially horizontally and then vertically several millimeters from diskovertebral junction ← displacement of nucleus pulposus in anterior + anterolateral direction producing traction on osseous attachment of annulus fibrosus [= fibers of Sharpey])
- enlargement of uncinate processes
- osteoarthritis = degenerative disease of synovium-lined apophyseal / costovertebral joints:
- degenerative spondylolisthesis
- cartilaginous node = intraosseous disk herniation
Myelography:
- delineation of thecal sac, spinal cord, exiting nerve roots
CT (accuracy >90%):
- facet joint disease (marginal sclerosis, joint narrowing, cyst formation, bony overgrowth)
- uncovertebral joint disease of cervical spine (osteophytes project into lateral spinal canal + neuroforamen)
MR:
- scalloping of cord (T2WI FSE / GRE images):
- anterior encroachment by disk / spondylosis
- posterior encroachment by ligamentum flavum hypertrophy
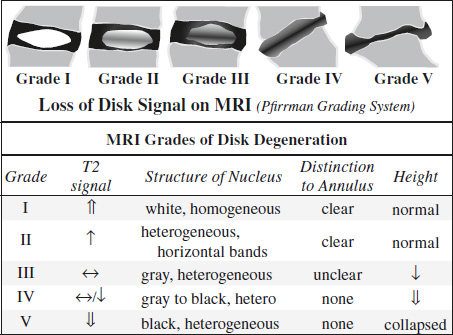
- loss of disk signal← desiccation ←decrease in water-binding proteoglycans + increase in collagen within nucleus pulposus) on T2WI
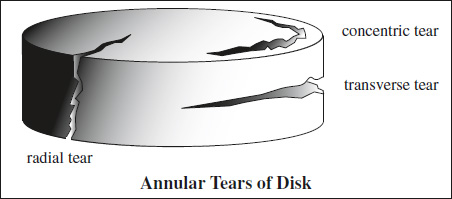
- annular tear:
- concentric tear - separation of annular lamellae
- transverse tear
- radial tear - crossing multiple annular lamellae with greater vertical dimension + more limited horizontal extent
- diskogenic pain
- does NOT imply disk herniation
- gap near middle of annulus
Modified Dallas Diskogram Classification
Grade Description 0 contrast confined within nucleus pulposus 1 contrast extends to inner third of annulus 2 contrast extends to middle third of annulus 3 outer third of annulus + <30° of circumference 4 outer third of annulus + >30° of circumference 5 extension of contrast beyond annulus - cleft of high SI in a normally hypointense outer annulus on T2WI
- contrast enhancement ← granulation tissue / hyperemia / inflammation
- reduction in disk height (late):
- Schmorl's node
- moderate linear uniform enhancement on T1WI
- vacuum phenomenon with low signal on T1WI
- endplate + marrow changes (Modic & DeRoos):
= linear signal alterations paralleling adjacent endplates- Type 1 (4%) = edema pattern
Cause: replacement of bone marrow with hyperemic fibrovascular tissue + edema ← acute disk degeneration- hypointense on T1WI + hyperintense on T2WI
- contrast-enhancement of marrow
- Type 2 (16%) = fatty marrow pattern
Cause: replacement of bone marrow with fat ← chronic disk degeneration- hyperintense marrow signal on T1WI
- iso- to mildly hyperintense on T2WI
- hypointense on STIR
- Type 3 = bony sclerosis pattern
Cause: replacement of bone marrow with sclerotic bone ← chronic disk degeneration after a few years- hypointense marrow signal on T1WI + T2WI
- Type 1 (4%) = edema pattern
- juxtaarticular synovial cyst in posterolateral spinal canal (most frequently at L4-5):
- smooth well-defined extradural mass adjacent to facet joint
- variable signal pattern ← serous, mucinous, gelatinous fluid components, air, hemorrhage
- contrast-enhancing hypointense perimeter ← fibrous capsule with calcium + hemosiderin
NUC:
SPECT imaging of vertebrae can aid in localizing increased uptake to vertebral bodies, posterior elements, etc.
- eccentrically placed increased uptake on either side of an intervertebral space (osteophytes, diskogenic sclerosis)
Sequelae:
- Disk bulging
- Disk herniation
- Spinal stenosis
- Facet joint disease
- Instability
- dynamic slip >3 mm on flexion-extension
- static slip >4.5 mm
- traction spurs
- vacuum phenomenon
DDx:Idiopathic segmental sclerosis of vertebral body (middle-aged / young patient, hemispherical sclerosis in anteroinferior aspect of lower lumbar vertebrae with small osteolytic focus, only slight narrowing of intervertebral disk; unknown cause)
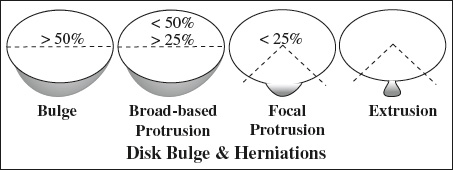
= concentric smooth expansion of softened disk material beyond the confines of endplates with disk extension outward involving >50% of disk circumference
Cause: weakened and lengthened but intact annulus fibrosus + posterior longitudinal ligament
Age: common finding in individuals >40 years of age
Location: L4-5, L5-S1, C5-6, C6-7
- rounded symmetric defect localized to disk space level
- smooth concave indentation of anterior thecal sac
- encroachment on inferior portion of neuroforamen
- accentuated by upright myelography
MR:
- nucleus pulposus hypointense on T1WI + hyperintense on T2WI ← desiccation (= water loss through degeneration + fibrosis)
Herniation of Nucleus Pulposus
= HNP = protrusion of disk material >3 mm beyond margins of adjacent vertebral endplates involving <50% of disk circumference
Cause: rupture of annulus fibrosus with disk material confined within posterior longitudinal ligament
- 21% of an asymptomatic population has a herniated disk!
- local somatic spinal pain = sharp / aching, deep, localized
- centrifugal radiating pain = sharp, well-circumscribed, superficial, “electric,” confined to dermatome
- centrifugal referred pain = dull, ill-defined, deep or superficial, aching or boring, confined to somatome (= dermatome + myotome + sclerotome)
Site:
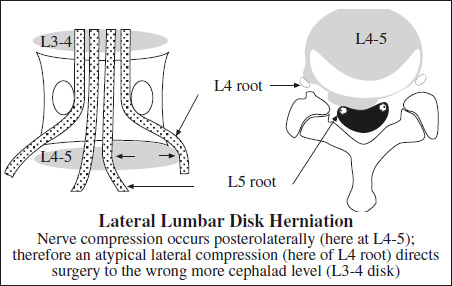
- posterolateral (49%) = weakest point along posterolateral margin of disk at lateral recess of spinal canal
- The posterior longitudinal ligament is tightly adherent to posterior central margins of disk!
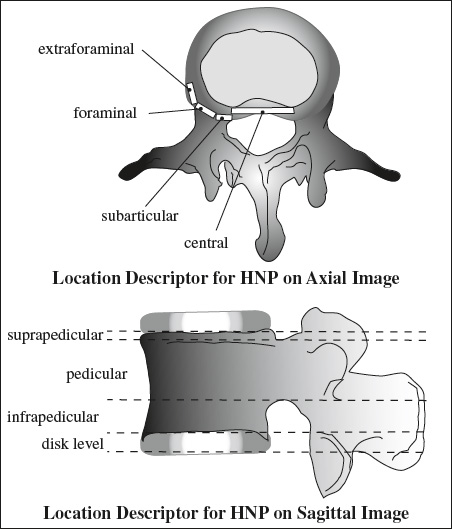
- posterocentral (8%)
- bilateral (to both sides of posterior ligament)
- lateral / foraminal (<10%)
- extraforaminal = anterior (commonly overlooked) (29%)
- intraosseous / vertical = Schmorl node (14%)
Myelography:
- sharply angular indentation on lateral aspect of thecal sac with extension above / below level of disk space (ipsilateral oblique projection best view)
- asymmetry of posterior disk margin
- double contour ← superimposed normal + abnormal side (horizontal beam lateral view)
- narrowing of intervertebral disk space (most commonly a sign of disk degeneration)
- deviation of nerve root / root sleeve
- enlargement of nerve root (“trumpet” sign) ← edema
- amputated / truncated nerve root (= nonfilling of root sleeve)
MR:
- herniated disk material of low SI displaces the posterior longitudinal ligament and epidural fat of relative high SI on T1WI
- “squeezed toothpaste” effect = hourglass appearance of herniated disk at posterior disk margin on sagittal image
- asymmetry of posterior disk margin on axial image
Cx:
- spinal stenosis mild = <⅓ moderate = ⅓ to ⅔ severe = >⅔
- neuroforaminal stenosis
Prognosis:
conservative therapy reduces size of herniation by
- 0–50% in 11% of patients,
- 50–75% in 36% of patients,
- 75–100% in 46% of patients
(secondary to growth of granulation tissue)
Broad-based Disk Protrusion
- triangular shape of herniation with a base wider than the radius of its depth
- 25–50% of disk circumference
Focal Disk Protrusion
- triangular shape of herniation with a base wider than the radius of its depth
- <25% of disk circumference
Disk Extrusion
= prominent focal extension of disk material through the annulus with only an isthmus of connection to parent disk through intact / ruptured posterior longitudinal ligament
- mushroom-shaped herniation with base narrower than the radius of its depth
- “toothpaste” sign
Disk Sequestration
= FREE FRAGMENT HERNIATION
= complete separation of disk material from parent disk with rupture through posterior longitudinal ligament into epidural space
- Missed free fragments are a common cause of failed back surgery!
- migration superiorly / inferiorly away from disk space with compression of nerve root above / below level of disk herniation
- disk material >9 mm away from intervertebral disk space = NO continuity
- soft-tissue density with higher value than thecal sac
DDx:
- Postoperative scarring (retraction of thecal sac to side of surgery)
- Epidural tumor
- Tarlov cyst (dilated nerve root sleeve)
- Conjoined nerve root (2 nerve roots arising from thecal sac simultaneously representing mass in ventrolateral aspect of spinal canal; normal variant in 1–3% of population)
Free Fragment Migration
= separated disk material travels above / below intervertebral disk space
- ± continuity
Peak age: 3rd–4th decade
- neck stiffness, muscle splinting; dermatomic sensory loss
- weakness + muscle atrophy; reflex loss
Sites: C6-7 (69%); C5-6 (19%); C7-T1 (10%); C4-5 (2%)
Sequelae:
- compression of exiting nerve roots with pain radiating to shoulder, arm, hand
- cord compression (spinal stenosis + massive disk rupture)
Prevalence: 1% of all disk herniations
Sites: T11-12
- calcification of disk fragments + parent disk (frequent)
- sciatica =
- Stiffness in back
- Pain radiating down to thigh / calf / foot
- Paresthesia / weakness / reflex changes
- pain exaggerated by coughing, sneezing, physical activity + worse while sitting / straightening of leg
Sites: L4-5 (35%) >L5/S1 (27%) >L3-4 (19%) >L2-3 (14%) >L1-2 (5%)