Differential Diagnosis of Musculoskeletal Disorders
- INTRAARTICULAR
- Osteocartilaginous bodies
- EXTRAARTICULAR = tendon slippage
- Fascia lata / gluteus maximus over greater trochanter
- Iliopsoas tendon over iliopectineal eminence
- Long head of biceps femoris over ischial tuberosity
- Iliofemoral ligament over anterior portion of hip capsule
- increase in distance between teardrop + femoral head
Cause: hip joint effusion - increase in mediolateral size of teardrop
Cause: hip dysplasia, chronic hip joint effusion during skeletal maturation
= acetabular floor bulging into pelvis
- center-edge angle of Wiberg of >40°
- medial wall of acetabulum projecting medially to ilioischial line by >3 mm (in males) / >6 mm (in females)
- crossing of medial + lateral components of pelvic “teardrop” (U-shaped radiodense area medial to hip joint)
- Anatomy:
- lateral aspect = articular surface of acetabular fossa
- medial aspect = anteroinferior margin of quadrilateral surface of ilium)
- obscured “teardrop” sign = pelvic teardrop obscured by femoral head
- UNILATERAL
- Tuberculous arthritis
- Trauma
- Fibrous dysplasia
- BILATERAL
- Rheumatoid arthritis
- Paget disease
- Osteomalacia
mnemonic: PROT
- Paget disease
- Rheumatoid arthritis
- Osteomalacia (HPT)
- Trauma
Pain with / after Hip Prosthesis
= pain in groin / thigh after hip arthroplasty
Prevalence of pain: 40%; ~ 120,000 hip arthroplasties per year in USA
- Postoperative hematoma
Incidence: 1.7% (within first 2 weeks)
Cx: wound dehiscence, infection - Heterotopic ossification
Incidence: 50–60% (within 8 weeks after surgery)
Risk factors: male gender, DISH, history of heterotopic ossification, osteoarthritis with preexisting heterotopic bone, ankylosing spondylitis- loss of motion ← ossifications bridging the joint
- Trochanteric bursitis
- Prosthetic / periprosthetic / cement fracture
- audible crack during tapping of stem (intraoperative!)
Incidence: in up to 18%
Predisposition: osteoporosis, osteolysis, stress shielding (= bone resorption due to decreased stress to bone) typically at base of greater trochanter and calcar - Dislocation
Risk factors: component malposition, imbalance of tissue tension, implant design, surgical approach, extent of surgical soft-tissue dissection, small femoral head, failure of abductor mechanism- posterior joint instability disruption of posterior joint capsule + short external rotator muscles / muscle atrophy
- anterior joint instability excessive acetabular cup anteversion >30° → impingement of femoral neck onto posterior rim of acetabular component → creation of posterior lever mechanism forcing femoral head out anteriorly
- Synovitis
- nonspecific mechanical irritation
- small amount of joint fluid without debris
- thin synovial lining
- polyethylene wear-induced = polymeric debris
- slowly progressive typically bulky osteolysis
- expansion of hip pseudocapsule by thick + particulate-appearing synovitis
- adverse local tissue reaction (metal hypersensitivity, metallosis)
- synovial thickness >7 mm
- infection (see below)
- nonspecific mechanical irritation
- Iliopsoas impingement syndrome & tendinopathy
Incidence: 4.3%
Cause:- idiopathic
- prominent oversized / malpositioned acetabular component
- retained cement
- excessively long iliac screws
- femoral head larger than native head
- gluteus medius and minimus tendon thickening / tear
- Aseptic loosening
= complete loss of implant fixation
Frequency: 50% of prostheses after 10 years; 30% require revision
Cause:- mechanical wear + tear of components
- small-particle disease
- Path: particulate debris incites inflammatory / immune reaction → unsuccessful enzymatic destruction of debris → cytokines and proteolytic enzymes damage bone and cartilage → osteolysis
- Histo: synovium-like pseudomembrane of histiocytes (95% of specimens), giant cells (80%), lymphocytes and plasma cells (25%), neutrophils (<10%)
- thin and enlarging >2 mm radiolucent area around component / between cement mantle + bone
- NEW radiolucent area <2 mm
- increasing osteolysis (due to particulate debris with foreign body granuloma)
- increasingly wide / asymmetric periprosthetic radiolucency
- endosteal scalloping around femoral stem
- pedestal formation = bone sclerosis distal to prosthetic tip in medullary canal ← micromotion
- bead shedding = punctate pieces of metal around in-growth component
- fractured cement mantle
- fractured acetabular cup screw
- newly tilted / migrated acetabular cup
- rotated / migrated / toggled femoral stem:
- subsidence (= distal migration) of prosthesis (up to 5 mm is normal for noncemented femoral component in first few months)
- “sinking” of femoral flange into lesser trochanter
- contrast medium between points of fixation
- motion of components on stress views / fluoroscopy
- inflammatory benign solid soft-tissue mass / pseudotumor around metal-on-metal implants
Rx: 30% require single-stage revision arthroplasty - Infection of Hip Prosthesis (= septic loosening)
- Frequency: 0.3–1.7–9.0%; <2% of primary arthroplasties; <5% of revisions
- Organism: Staphylococcus epidermidis (31%), Staphylococcus aureus (20%), Streptococcus viridans (11%), Escherichia coli (11%), Enterococcus faecalis (8%), group B streptococcus (5%)
- Time of onset: ¹/³ within 3 months, ¹/³ within 1 year, ¹/³ >1 year
- Path: bacteria bind to implant
- Histo: neutrophils present in large numbers
- Rx: excisional arthroplasty + protracted course of antimicrobial therapy + revision arthroplasty
- clinical signs of infection often absent
Plain film:- “aggressive” osteolysis with ill-defined margins ← particulate debris with foreign body granuloma / abscess
- periostitis = periosteal new bone (100% specific, 16% sensitive for infection)
- periarticular fluid collection with irregular walls communicating with joint (CT arthrography) and sinus track to skin
NUC (83% sensitive, 88% specific): (see below)
PET:- NO advantage over bone marrow imaging as a combination of 111In-labeled leukocytes and 99mTc sulfur colloid
Arthrography:- irregularity of joint pseudocapsule
- filling of nonbursal spaces / sinus tracts / abscess cavities
Aspiration of fluid under fluoroscopy (12–93% sensitive, 83–92% specific for infection):- joint aspiration: high number of FP + FN
- injection of contrast material to confirm intraarticular location
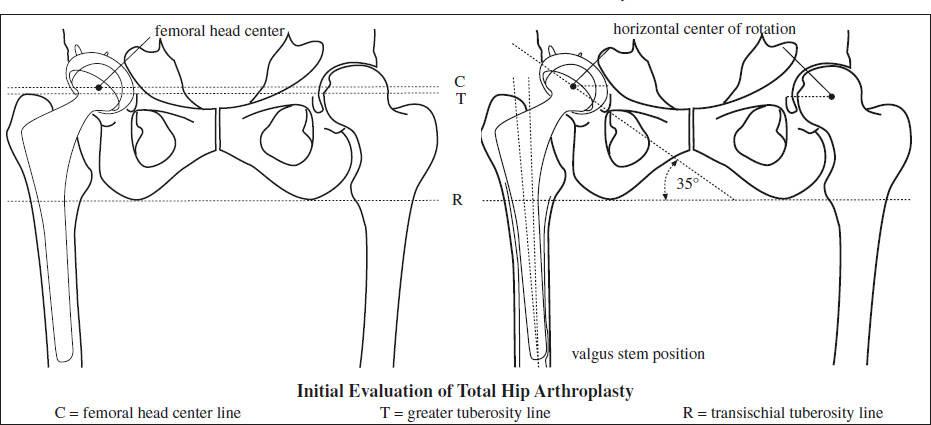
Evaluation of Total Hip Arthroplasty
MEASUREMENTS
Reference line: transischial tuberosity line (R)
- Leg length = vertical position of acetabular component
= comparing level of greater / lesser tuberosity (T) with respect to line R
High placement: shorter leg, less effective muscles crossing the hip joint
Low placement: longer leg, muscles stretched to point of spasm with risk of dislocation - Vertical center of rotation
= distance from center of femoral head (C) to line R - Horizontal center of rotation
= distance from center of femoral head (C) to teardrop / other medial landmark
Lateral position: iliopsoas tendon crosses medial to femoral head center of rotation increasing risk of dislocation - Lateral acetabular inclination = horizontal version
= angle of cup in reference to line R (40° ± 10° desirable)
Less angulation: stable hip, limited abduction
Greater angulation: risk of hip dislocation - Acetabular anteversion (15° ± 10° desirable)
= lateral radiograph of groin
Retroversion: risk of hip dislocation - Varus / neutral / valgus stem position
Varus position: tip of stem rests against lateral endosteum, increased risk for loosening
Valgus position: tip of stem rests against medial endosteum, not a significant problem - Femoral neck anteversion works synergistically with acetabular anteversion, true angle assessed by CT
- Cup overhang >12 mm associated with iliopsoas impingement, assessed by CT
- Unfavorable position of screw tip eg, abutting the L5 nerve root in sciatic notch
Type of Hip Prosthesis
- Hemiprosthesis
- preservation of acetabular cartilage + subchondral bone plate
- only femoral stem is fixed by
- bone cement (polymethylmethacrylate)
- press-fit / in-growth with textured surface facilitating in-growth of trabecular bone
- Unipolar head
= 1 articulation between metal implant head + native acetabular cartilage - Bipolar head
= 2 articulations to improve range of motion:- between inner head + liner of bipolar head
- between bipolar head (shell) + acetabulum
- smooth outer surface
- slightly greater than hemispheric shape
- no screw holes
- Total prosthesis (mostly for treatment of arthritis)
- acetabulum reamed
- Conventional
- screw holes in acetabular cup
- Resurfacing
- = replacing articulating surfaces of hip joint and removing very little bone
- small acetabular cup in pelvic socket
- femoral head component seated with a pegged stem inside a preserved femoral neck
Radiographic Findings in Total Hip Arthroplasty
- NORMAL
- irregular cement-bone interface
- = normal interdigitation of PMMA (polymethylmethacrylate) with adjacent bone remodeling providing a mechanical interlock
- PMMA is not a glue!
- thin lucent line along cement-bone interface
- = 0.1–1.5-mm thin connective tissue membrane (“demarcation”) along cement-bone interface accompanied by thin line of bone sclerosis
- irregular cement-bone interface
- ABNORMAL
- wide lucent zone at cement-bone interface
- = ≥2-mm lucent line along bone-cement interface due to granulomatous membrane
- Cause: component loosening ± reaction to particulate debris (eg, PMMA, polyethylene)
- lucent zone at metal-cement interface along proximal lateral aspect of femoral stem
- = suboptimal metal-cement contact at time of surgery / loosening
- well-defined area of bone destruction (= histiocytic response, aggressive granulomatous disease)
- Cause: granulomatous reaction as response to particulate debris / infection / tumor
- asymmetric positioning of femoral head within acetabular component
- Cause: acetabular wear / dislocation of femoral head / acetabular disruption / liner displacement / deformity
- cement fracture
- Cause: loosening
- wide lucent zone at cement-bone interface
Scintigraphy for Prosthetic Failure
- increased uptake of bone agent, 67Gallium, 111Indium-labeled leukocytes, complementary technetium-labeled sulfur colloid + combinations
- Bone Scintigraphy (high NPV):
- negative
- periprosthetic uptake indistinguishable from surrounding nonarticular bone = no prosthetic abnormality (= high NPV)
- positive for infection / loosening:
- diffuse intense uptake around femoral component (= generalized osteolysis unreliable in separating infection from loosening)
- diffuse periprosthetic uptake favors infection
- focal uptake at distal tip of femoral component in >1 year old prosthesis = aseptic loosening
- diffuse intense uptake around femoral component (= generalized osteolysis unreliable in separating infection from loosening)
- nonspecific:
- periprosthetic activity generally decreases with time:
- variable uptake patterns in 1st year after implantation
- persistent uptake >1 year is frequent in cementless / porous-coated hip replacements
- periprosthetic activity generally decreases with time:
- negative
- Sequential bone/gallium scintigraphy (60–80% accurate, modest improvement over bone scintigraphy alone):
- negative for infection:
- gallium distribution normal regardless of findings on bone imaging
- spatially congruent distribution of both radiotracers + gallium intensity less than bone tracer
- inconclusive:
- spatially congruent radiotracer distribution + similar uptake intensity for both radiotracers
- positive for infection:
- spatially incongruent distribution of the 2 radiotracers
- gallium uptake intensity exceeds that of bone agent
- negative for infection:
- Labeled leukocyte scintigraphy:
- positive for infection:
- intensity exceeds that of a reference point
- activity outside normal distribution
- positive for infection:
- Combined labeled leukocyte–marrow scintigraphy
= WBC/sulfur colloid scintigraphy (study of choice):- Accuracy: 88–98%
- Concept:99mTc-sulfur colloid maps aberrantly located normal bone marrow as a point of reference for leukocyte tracer
- positive for infection:
- labeled leukocyte activity without corresponding sulfur colloid activity ← osteomyelitis stimulates WBC uptake + depresses sulfur colloid uptake
- negative for infection:
- spatially congruent distribution of both radiotracers / any other pattern of uptake