= INTRACEREBRAL HEMATOMA
Etiology:
- Very common
- Chronic hypertension (50%)
Age:>60 years
Location: external capsule and basal ganglia (putamen in 65%) / thalamus (25%), pons (5%), brainstem (10%), cerebellum (5%), cerebral hemisphere (5%) - Trauma
- Aneurysm
- Vascular malformation: AVM, cavernous hemangioma, venous angioma, capillary telangiectasia
- Chronic hypertension (50%)
- Common
- Hemorrhagic infarction = hemorrhagic transformation of stroke
- Amyloid angiopathy (20%): elderly patients
- Coagulopathy (5%): DIC, hemophilia, idiopathic thrombocytopenic purpura; aspirin, heparin, coumadin
- Drug abuse (5%): amphetamines, cocaine, heroine
- Bleeding into tumor
- primary: GBM, ependymoma, oligodendroglioma, pituitary adenoma
- metastatic: melanoma, choriocarcinoma, renal cancer, thyroid cancer, adenocarcinoma
- Uncommon
- Venous infarction
- Eclampsia
- Septic emboli
- Vasculitis (especially fungal)
- Encephalitis
Progression: hematoma gradually “snowballs” in size, dissects along white matter tracts; may decompress into ventricular system / subarachnoid space
Resolution: resorption from outside toward the center; rate depends on size of hematoma (usually 1–6 weeks)
FALSE-NEGATIVE CT:
- Impaired clotting
- Anemia
- iso- / hypodense stage
Hyperacute Cerebral Hemorrhage
Time period: 4–6 hr
Substrate: fresh oxygenated arterial blood contains 95% diamagnetic (= NO unpaired electrons) intracellular oxyhemoglobin (Fe2+) with higher water contents than white matter; oxyhemoglobin persists for 6–12 hr)
NECT:
- homogeneous consolidated high-density lesion (50–70 HU) with irregular well-defined margins increasing in density during day 1–3 (hematoma attenuation dependent on hemoglobin concentration + rate of clot retraction)
- usually surrounded by low attenuation appearing within 24–48 hours ← edema, contusion
- irregular shape in trauma
- spherical + solitary in spontaneous hemorrhage
- less mass effect compared with neoplasms
MR (less sensitive than CT during first hours):
- little difference to normal brain parenchyma = center of hematoma iso- to hypointense on T1WI + minimally hyperintense on T2WI
- peripheral rim of hypointensity (= degraded blood products as clue for presence of hemorrhage)
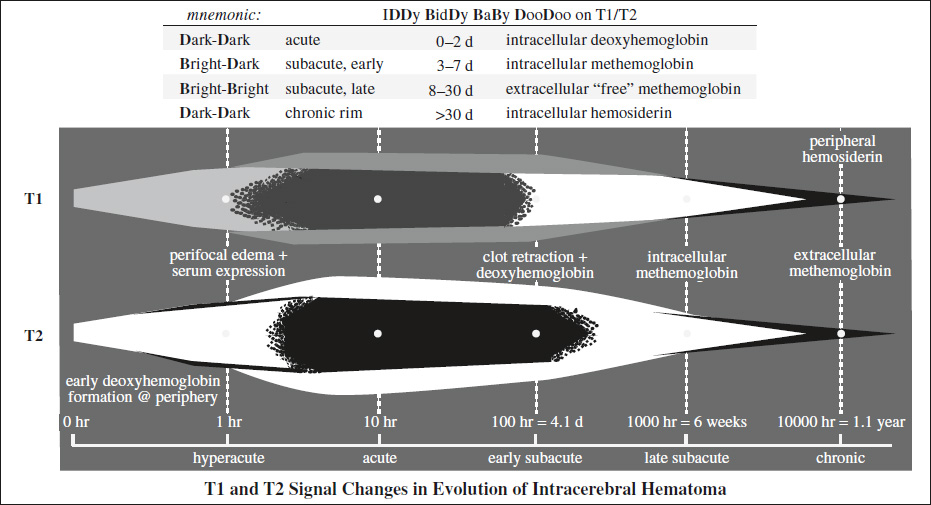
Acute Cerebral Hematoma
Time period: 12–48 hours
Substrate: paramagnetic (= 4 unpaired electrons) intracellular deoxyhemoglobin (Fe2+); deoxyhemoglobin persists for 3 days
MR:
- slightly hypo- / isointense on T1WI (= paramagnetic deoxyhemoglobin in intact hypoxic RBCs within blood clot does not cause T1 shortening)
- very hypointense on T2WI ← progressive concentration of RBCs, blood clot retraction, and fibrin production shorten T2
- surrounding tissue isointense on T1WI / hyperintense on T2WI ← edema
Early Subacute Cerebral Hematoma
Time period: 3–7 days
Substrate: intracellular strongly paramagnetic (= 5 unpaired electrons) methemoglobin (Fe3+) inhomogeneously distributed within cells
NECT:
- increase in size of hemorrhagic area over days / weeks
- high-density lesion within 1st week; often with layering
MR:
- very hyperintense on T1WI (= oxidation of deoxyhemo-globin to methemoglobin → marked shortening of T1)
- beginning peripherally in parenchymal hematomas
- beginning centrally in partially thrombosed aneurysm (oxygen tension higher in lumen)
DDx: melanin, high-protein concentration, flow-related enhancement, gadolinium-based contrast agent - very hypointense on T2WI (= intracellular methemoglobin causes T2 shortening)
Late Subacute Cerebral Hematoma
Time period:>1 week
Substrate: extracellular strongly paramagnetic methemoglobin (homogeneously distributed)
NECT:
- gradual decrease in density from periphery inward (1–2 HU per day) during 2nd + 3rd week
CECT:
- peripheral rim enhancement at inner border of perilesional lucency (1–6 weeks after injury) in 80% ← blood-brain barrier breakdown / luxury perfusion / formation of hypervascular granulation tissue
- ring blush may be diminished by administration of corticosteroids
MR:
- hyperintense on T1WI (= RBC lysis allows free passage of water molecules across cell membrane)
- hyperintense on T2WI (= compartmentalization of methemoglobin is lost ← RBC lysis)
- surrounding edema isointense on T1WI + hyperintense on T2WI
Chronic Cerebral Hematoma
Time period:>1 months
Substrate: superparamagnetic ferritin (= soluble and stored in intracellular compartment) and hemosiderin (= insoluble and stored in lysosomes) cause marked field inhomogeneities
NECT:
- isodense hematoma from 3rd–10th week with perilesional ring of lucency
CT:
- hypodense phase (4–6 weeks) ← fluid uptake by osmosis
- decreased density (3–6 months) / invisible
- after 10 weeks lucent hematoma (= encephalomalacia ← proteolysis and phagocytosis + surrounding atrophy) with ring blush (DDx: tumor)
MR:
- rim slightly hypointense on T1WI and very hypointense on T2WI (= superparamagnetic hemosiderin + ferritin within macrophages); rim gradually increases over weeks in thickness, eventually fills in entire hematoma = HALLMARK
- center hyperintense on T1WI + T2WI (= extracellular methemoglobin of lysed RBCs just inside the darker hemosiderin ring); present for months to 1 year
- surrounding hyperintensity on T2WI (= edema + serum extruded from clot) with associated mass effect; should resorb within 4–6 weeks (DDx: malignant hemorrhage)
Prognosis:
- Herniation (if hematoma 3–4 cm in size)
- Death (if hematoma >5 cm in size)
= rupture of small distal microaneurysms in lenticulostriate arteries in patients with poorly controlled systemic arterial hypertension
MR Appearance of Intracerebral Hematoma
|
Cx:
- Dissection into adjacent ventricles (⅔)
- Porencephaly
- Atrophy with ipsilateral ventricular dilatation
