Bone and Soft-Tissue Disorders
= CONGENITAL DYSPLASIA OF HIP
= deformity of acetabulum ← disrupted relationship between femoral head and acetabulum
◊Acetabular dysplasia (without femoral subluxation / dislocation) can be determined only by imaging!
Etiology:
- Late intrauterine event (98%)
- mechanical:
- oligohydramnios (restricted space in utero)
- firstborn (tight maternal musculature)
- in 60% of patients with DDH
- breech position (hip hyperflexion results in shortening of iliopsoas muscle; L÷R = 4÷1)
- in 30–50% of patients with DDH
- only 2–4% of deliveries are breech
- physiologic (females are more sensitive to):
- maternal estrogen (not inactivated by immature fetal liver) blocks cross-linkage of collagen fibrils
- pregnancy hormone relaxin
- mechanical:
- Teratologic (2%) ← neuromuscular disorder (myelodysplasia, arthrogryposis) occurring during 12th–18th week GA
- Postnatal onset (<1%)
Prevalence: 0.15% of neonates (Australia 1%, Netherlands 3.7%, Poland 3.9%, Israel 5.9%, Austria 6.6%, Norway 16.9%)
Age: most dislocations probably occur after birth; M÷F = 1÷4–1÷8; Caucasians >Blacks
Increased risk:
- infants born in frank breech position (25%; risk of breech÷vertex = 6–8÷1)
- congenital torticollis (10–20%)
- skull-molding deformities; scoliosis; generalized joint laxity (Larsen syndrome, Ehlers-Danlos syndrome, Down syndrome [5%]); neuromuscular disorders (eg, myelodysplasia, spina bifida, sacral agenesis, arthrogryposis multiplex)
- family history of DDH (6–20%): 6% risk for subsequent sibling of normal parents, 36% risk for subsequent sibling of one affected parent; 12% risk for patient's own children
- foot deformities [metatarsus adductus, clubfoot (2%)]
- neonatal hyperextension of hips: swaddling of infants in hip extension / strapping to cradle board
Anatomy: acetabulum has a small bony component + a large cartilaginous component at birth; acetabulum highly susceptible for modeling within first 6 weeks of age + less susceptible >16 weeks of age
Classification:
- Normal hip
- Lax = subluxable hip
- Subluxability up to 6 mm is normal in newborns (still under influence of maternal hormones); decreasing to 3 mm by 2nd day of life
- Concentric dislocatable unstable hip
= joint laxity allowing nondisplaced femoral head to become subluxed / dislocated under stress
Prevalence: 0.25–0.85% of all newborn infants (⅔ are firstborns)- Barlow positive
- slight increase in femoral anteversion
- mild marginal abnormalities in acetabular cartilage
- early labral eversion
Prognosis: 60% will become stable after 1 week; 88% will become stable by age of 2 months - Decentered subluxed hip
= femoral head shallow in location- loss of femoral head sphericity
- increased femoral anteversion
- early labral inversion
- shallow acetabulum
- Eccentric dislocated hip
= femoral head frankly displaced out of acetabulum- reducible = Ortolani positive
- irreducible = Ortolani negative
- accentuated flattening of femoral head
- shallow acetabulum
- limbus formation (= inward growth + hypertrophy of labrum)
- “hip click” = usually result of joint capsule and tendon stretching + snapping (often confused with “hip clunk”)
- positive examination result (up to 3 months of age):
- positive Ortolani reduction test = reduction of dislocated femoral head into the acetabulum by lifting the flexed thigh + pushing the greater trochanter anteriorly; may be associated with audible “clunk”
- positive Barlow dislocation test = posterior displacement of nondislocated proximal femur by progressive adduction with downward pressure (piston maneuver) on flexed hips and knees associated with audible “clunk”
- warning signs on physical examination:
- limited hip abduction on affected side
- shortening of thigh on affected side:
- asymmetric thigh / buttock creases
- Allis sign = Galeazzi sign = affected knee is lower with knees bent in supine position
- Trendelenburg test = visible drooping + shortening on dislocated side with child standing on both feet, then one foot
Location: left÷right÷bilateral = 11÷1÷4
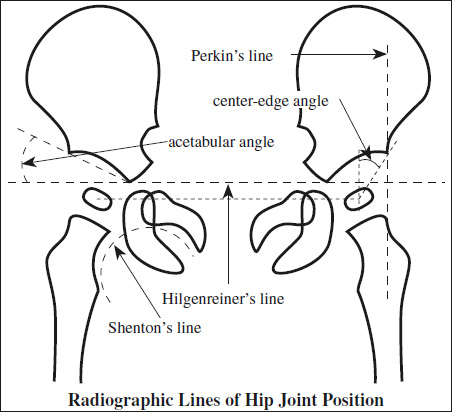
Radiologic lines:
- Line of Hilgenreiner
= line connecting superolateral margins of triradiate cartilage - Acetabular angle / index
= slope of acetabular roof = angle that lies between Hilgenreiner's line and a line drawn from most superolateral ossified edge of acetabulum to superolateral margin of triradiate cartilage - Perkin line
= vertical line to Hilgenreiner's line through the lateral rim of acetabulum - Shenton curved line
= arc formed by inferior surface of superior pubic ramus (= top of obturator foramen) + medial surface of proximal femoral metaphysis to level of lesser trochanter- disruption of line (DDx: coxa valga)
- Center-edge angle of Wiberg = angle subtended by one line drawn from the acetabular edge to center of femoral head + second line perpendicular to line connecting centers of femoral heads
- <25° suggests femoral head instability
AP pelvic radiograph: >4– 6 months of age (von Rosen view = legs abducted 45° + thighs internally rotated)
◊Not reliable first 3 months of life!
- proximal + lateral migration of femoral neck:
- eccentric position of proximal femoral epiphysis (position estimated by a circle drawn with a diameter equivalent to width of femoral neck)
- interrupted discontinuous arc of Shenton's line
- line drawn along axis of femoral shaft will not pass through upper edge of acetabulum but intersect the anterior-superior iliac spine (during Barlow maneuver)
- apex of metaphysis lateral to edge of acetabulum
- femoral shaft above horizontal line drawn through the Y-synchondrosis
- unilateral shortening of vertical distance from femoral ossific nucleus / femoral metaphysis to Hilgenreiner's line
- femoral ossific nucleus / medial beak of femoral metaphysis outside inner lower quadrant of coordinates established by Hilgenreiner's + Perkin's lines
- acetabular dysplasia = shallow incompletely developed acetabulum:
- acetabular angle >30° strongly suggests dysplasia
- development of false acetabulum
- delayed ossification of femoral epiphysis (usually evident by 4 months (range, 2nd–8th months) of life
US (practical only):
Screening period: >2 weeks and up to 4–6 months of age
- Instability often resolves spontaneously by 2 weeks of age!
- Examination impractical beyond 4–6 months of age
- static evaluation (popularized in Europe by Graf)
- dynamic evaluation (popularized in USA by Harcke)
- Relationship of femoral head & acetabulum
- femoral head position at rest in neutral position
- hip instability under motion + stress maneuvers
- dislocated (= eccentric) hip can be reduced (Ortolani positive):
- hypoechoic femoral head not centered over triradiate cartilage between pubis + ischium (on transverse view)
- increased amount of soft-tissue echoes (“pulvinar”) between femoral head and acetabulum
- cartilaginous acetabular labrum interposed between head and acetabulum (inverted labrum)
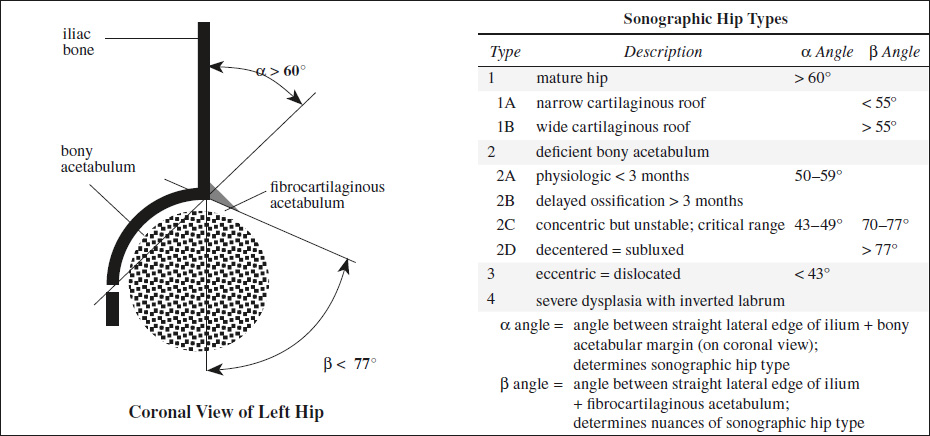
- posterior + superior dislocation of head against ilium
- “equator” sign = <50% of femoral head lies medial to line drawn along iliac bone (on coronal view): >58% coverage is normal; 58–33% coverage is indeterminate; <33% coverage is abnormal
- Femoral head
- disparity in size of directly visualized unossified femoral head
- disparity in presence + size of ossific nucleus
- Acetabulum
- delayed ossification of acetabular corner
- wavy contour of bony acetabulum with only slight curvature
- abnormally acute alpha angle (= angle between straight lateral edge of ilium + bony acetabular margin)
- α>60° in an infant is normal
- α55–60° can be normal <4 weeks of age
- α<55° occurs in an immature acetabulum
- 4°–6° interobserver variation!
Prognosis: alpha-angle <50° at birth / 50°–59° after 3 months indicates significant risk for dislocation without treatment; follow-up at 4-week intervals are recommended
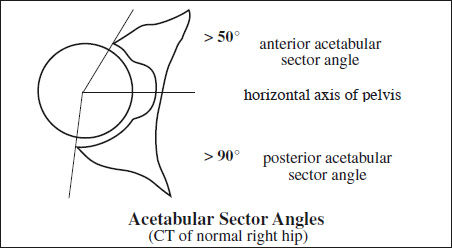
CT (during cast treatment / attempted closed reduction):
- sector angle = angle between line drawn from center of femoral head to acetabular rim + horizontal axis of pelvis (= reflects acetabular support)
- anterior acetabular sector angle <50°
- posterior acetabular sector angle <90°
Cx:
- Degenerative joint disease
- Avascular necrosis of femoral head
Obstacles to reduction:
- Intraarticular obstacle to reduction
- pulvinar = fibrofatty tissue at apex of acetabulum
- hypertrophy of ligamentum teres
- labral hypertrophy / inversion
- Extraarticular obstacle to reduction (iliopsoas tendon impingement on anterior joint capsule with infolding of joint capsule)
Prognosis: 78% of hips become spontaneously normal by 4th week + 90% by 9th week; >90% of abnormalities identified by ultrasound resolve spontaneously
Rx:
- Flexion-abduction-external rotation brace (Pavlik harness) / splint / spica cast
- Femoral varus osteotomy
- Pelvic (Salter) / acetabular rotation
- Increase in acetabular depth (Pemberton)
- Medialization of femoral head (Chiari)