Bone and Soft-Tissue Disorders
= inflammation of bone and marrow caused by bacteria (most commonly pyogenic bacteria + mycobacteria), fungi, parasites, viruses
Predisposed: immunosuppression, diabetes mellitus, sickle cell disease, intravenous drug abuse, alcoholism
Source of infection:
- direct inoculation: open fracture / direct trauma (commonly in young adults)
- prominent local signs and symptoms
- hematogenous: bacteremia (commonly in elderly / child)
- slow insidious progression of symptoms
- positive blood culture (in 50%)
- extension from adjacent soft-tissue infection
Location: tibia, wrist, femur, rib, thoracolumbar spine
Dx: requires 2 out of 4 of the following criteria
- purulent material draining from site of osteomyelitis
- positive findings at bone tissue / blood culture
- localized classic physical findings of bone tenderness
- positive radiologic findings
Age: most commonly affects children
Organism:
- newborns: S. aureus, group B streptococcus, E. coli
- children: S. aureus (blood cultures in 50% positive)
- adults: S. aureus (60%), enteric species (29%), Streptococcus (8%)
- drug addicts: Pseudomonas (86%), Klebsiella, Enterobacteriae; (57 days average delay in diagnosis)
- sickle cell disease: S. aureus, Salmonella
- diabetics: often multiple organisms like S. aureus, Streptococcus, E. coli, Klebsiella, Clostridia, Pseudomonas (in soil + sole of shoes)
- HIV-infected patients: TB, atypical mycobacteria
Cause:
- genitourinary tract infection (72%)
- lung infection (14%)
- dermal infection (14%): direct contamination from a soft-tissue lesion in diabetic patient
Pathophysiology:
bacterial growth in bone → entrapped bone becomes necrotic within 48 hours → spread to shaft ± periosteum (large subperiosteal abscess in children) → lifted periosteum impedes blood supply → sequestrum (= dead bone) → rupture of periosteum → draining sinus + soft-tissue abscess; host response causes reactive sleeve of new bone deposition (= involucrum)
[involucrum, Latin = covering / sheath]
[sequestrum, Latin = deposit], [cloaca, Latin = sewer, canal]
Location:
- Lower extremity (75%) over pressure points in diabetic foot
- Vertebra (53%) = infectious spondylitis: lumbar (75%) >thoracic >cervical
- Radial styloid (24%)
- Sacroiliac joint (18%)
- leukocytosis + fever (66%)
Conventional radiographs (insensitive):
- radiographs normal in 95% at presentation (notoriously poor in early phase of infection for as long as 10–21 days)
DDx: infarction (similar radiographic findings) - some abnormality in 90% 28 days after onset of infection:
- localized soft-tissue swelling adjacent to metaphysis with obliteration of usual fat planes (after 3–10 days)
- permeative metaphyseal osteolysis (lags 7–14 days behind pathologic changes)
- endosteal erosion
- intracortical fissuring
- involucrum = cloak of laminated / spiculated periosteal reaction (develops after 20 days)
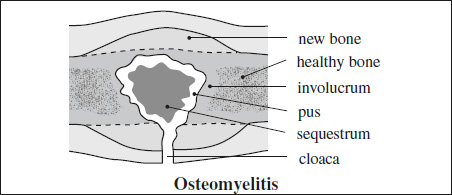
- button sequestrum = detached necrotic cortical bone (develops after 30 days)
- cloaca formation = space in which dead bone resides
US:
- soft-tissue changes, fluid collection, periosteal reaction
CT:
- overlying soft-tissue swelling
- periosteal reaction
- hypoattenuating marrow = density difference of >20 HU compared to healthy side indicates marrow infection
- trabecular coarsening
- focal cortical erosion
- extramedullary fat-fluid level ← cortical breach
MR (82% sensitive, 80% specific in diabetics):
- demonstrates extent of infection
- normal marrow / low SI on T2WI excludes osteomyelitis!
- bone marrow hypointense on T1WI in geographic confluent pattern ← infiltration by inflammatory cells + purulent material
- hyperintense relative to normal fatty marrow on T2WI / STIR (= water-rich inflammatory tissue + edema fluid)
- Periarticular bone marrow edema can be seen adjacent to joints involved by noninfectious inflammatory arthropathy / osteoarthritis and does not reliably indicate osteomyelitis!
DDx: noninfectious inflammatory arthropathy (Charcot joint), osteoarthritis, cellulitis, normal hematopoietic marrow in children
- Periarticular bone marrow edema can be seen adjacent to joints involved by noninfectious inflammatory arthropathy / osteoarthritis and does not reliably indicate osteomyelitis!
- variable enhancement after IV administration of Gd-chelate
- focal / linear cortical involvement hyperintense on T2WI
- subperiosteal infection = hyperintense halo surrounding cortex on T2WI
- sinus tract (= communication of medullary fluid collection with soft-tissue fluid collection through cortical disruption) = hyperintense line on T2WI extending from bone to skin surface + enhancement of its borders
- sequestrum = central hypointense area on T2WI
Abscess characteristics at MRI:
- hyperintense enhancing rim (= hyperemic zone) around a central focus of low intensity (= necrotic / devitalized tissue) on contrast-enhanced T1WI
- hyperintense fluid collection surrounded by hypointense pseudocapsule on T2WI + contrast enhancement of granulation tissue
- adjacent hyperintense soft tissues on T2WI
- fat-suppressed contrast-enhanced imaging (88% sensitive + 93% specific compared with 79% + 53% for nonenhanced MR imaging)
DDx: bone tumor (“no penumbra” sign = higher-SI layer of granulation tissue lining abscess cavity on T1WI)
NUC (~ 90% accurate):
Advantage: imaging of whole skeleton!
- 67Ga scan: 100% sensitivity; increased uptake 1 day earlier than for 99mTc-MDP
◊ Gallium also helpful for chronic osteomyelitis! - Static 99mTc-diphosphonate: 83% sensitive with 5–60% false-negative rate in neonates + children because of
- masking effect of epiphyseal plates
- early diminished blood flow with infection
- spectrum of uptake pattern from hot to cold
- Triple-phase skeletal scintigraphy:
92% sensitive + 87% specific
◊Positive within 1–2 days after onset of symptoms!
Phase 1: Radionuclide angiography = increased perfusion phase of regional blood flow
Phase 2: “blood pool” images ← hyperemia = tissue phase
Phase 3: “bone uptake” ←- increased osteoblastic activity = delayed phase
- increased activity in all 3 phases (HALLMARK)
- photopenia (rare) = “cold” osteomyelitis (due to vascular thrombosis + bone infarct) → may become “hot” at subsequent imaging (esp. TB)
- No uptake during delayed phase = NO osteomyelitis!
- Obtain SPECT whenever possible!
Limitations: diagnostic difficulties in children (motion), in posttraumatic / postoperative state, diabetic neuropathy (poor blood supply), neoplasia, septic arthritis, Paget disease, healed osteomyelitis, noninfectious inflammatory process - WBC-scan:
- 111In-labeled leukocytes: best agent for acute infections
- 99mTc-hexamethylpropyleneamine oxime labeled leukocytes: preferred over 111In-leukocyte imaging especially in extremities
- WBC scans have largely replaced gallium imaging for acute osteomyelitis ← faster imaging + greater resolution ← improved photon flux and improved dosimetry (higher dose allowed relative to 111In)
- Bone marrow imaging (99mTc-sulfur colloid) in combination with WBC-scan
- “cold” area in early osteomyelitis subsequently becoming “hot” if localized to long bones / pelvis (not seen in vertebral bodies)
- local increase in radiopharmaceutical uptake (positive within 24–72 hours)
Scintigraphy is more useful than MR imaging in a child when the suspected site of osteomyelitis is not clinically evident (+ bacteremia / limping / refusing to bear weight)
Cx:
- Abscess of soft-tissue / bone
- Fistula formation
- Pathologic fracture
- Septic arthritis (← extension into joint)
- Growth disturbance due to epiphyseal involvement
- Neoplasm
- Amyloidosis
- Severe deformity with delayed treatment
Acute Pyogenic Neonatal Osteomyelitis

Age: onset <30 days of age
Prevalence: 1–3÷1000 admissions to nursery
Risk factors: prematurity, low birth weight, complicated delivery, antecedent illness, umbilical artery catheterization, invasive procedure
Anatomy: metaphyseal vessels penetrate growth plate (= physis) crossing into epiphysis
Site:metaphysis + epiphysis of long bones
- little / no systemic disturbance
- multicentric involvement more common
- often joint involvement (transphyseal / subperiosteal route)
- bone scan falsely negative / equivocal in 70%
Acute Pyogenic Osteomyelitis in Infancy
Age:<18 months of age
Anatomy: metaphyseal vessels penetrate growth plate (= physis) crossing into epiphysis
Pathomechanism: spread from metaphysis to epiphysis
- striking soft-tissue component
- subperiosteal abscess with extensive periosteal new bone
Cx: frequent infection of epiphysis + joint ← transphyseal blood flow
◊osteomyelitis of proximal femur is usually associated with septic arthritis in children <1 year of age.
Prognosis: rapid healing
Acute Pyogenic Osteomyelitis in Childhood
Cause: hematogenous spread ← bacteremia
Organism: Staphylococcus aureus, β-hemolytic Streptococcus, Streptococcus pneumoniae, Escherichia coli, Pseudomonas aeruginosa; increasing incidence of methicillin-resistant S. aureus (MRSA) and Kingella kingae
Age: 2–16 years of age
Anatomy: transphyseal vessels closed; metaphyseal vessels adjacent to growth plate loop back toward metaphysis
Site: primary focus of infection located in metaphysis via nutrient artery; abscess formation in medulla with spread to cortex
Pathophysiology: metaphyseal capillaries lack phagocytic lining cells → uninhibited growth of microorganisms
Location: femur, tibia
- sequestration frequent
- periosteal elevation → disruption of periosteal blood supply
- small single / multiple osteolytic areas in metaphysis
- extensive periosteal reaction parallel to shaft (after 3–6 weeks); may be “lamellar nodular” (DDx: osteoblastoma, eosinophilic granuloma)
- shortening of bone ← destruction of epiphyseal cartilage
- growth stimulation ← hyperemia + premature maturation of adjacent epiphysis
- midshaft osteomyelitis less frequent site
- serpiginous tract with small sclerotic rim (PATHOGNOMONIC)
CAVE:
- Increased uptake in contralateral limb in patient with a limp
- Diffuse hyperemia in normal bones of an extremity involved with focal osteomyelitis should not be mistaken for multifocal osteomyelitis / septic arthritis.
Acute Pyogenic Osteomyelitis in Adulthood
Associated with: soft-tissue abscess, pathological fracture
Risk factors: IV drug use, previous trauma, immunosuppressed state, diabetes
Site: epiphysis + subchondral region (after growth plate closure)
- delicate periosteal new bone
- joint involvement common
- 67Ga citrate more useful than 111In-labeled leukocytes ← lymphocytes are predominant cell type
- CT considered superior to MR for chronic osteomyelitis
- cortical destruction and gas
- thick irregular sclerotic bone with radiolucencies, elevated periosteum, chronic draining sinus
Sclerosing Osteomyelitis of Garré
= STERILE OSTEOMYELITIS
= low-grade nonnecrotic nonpurulent infection
Location: mandible (most commonly)
- focal bulge of thickened cortex ← sclerosing periosteal reaction)
DDx: osteoid osteoma, stress fracture
Chronic Recurrent Multifocal Osteomyelitis
= benign self-limited disease of genetic etiology
◊May be identical to chronic sclerosing osteomyelitis of Garré; childhood equivalent to SAPHO syndrome
Age: children + adolescents; M÷F = 1÷2
Histo: nonspecific subacute / chronic osteomyelitis
- pain, tenderness soft-tissue swelling
- limited range of motion
- elevated ESR + C-reactive protein; normal WBC
Associated with: psoriasis, palmoplantar pustulosis, inflammatory bowel disease
Location: tibia >femur >clavicle >fibula
◊Whole-body imaging (99mTc bone scintigraphy, MRI) usually shows additional unsuspected locations
Site: metaphyses of long bones (75%); often symmetric
- No abscess formation, fistula, sequestra
Early:
- small areas of bone lysis, often confluent
- progressive sclerosis surrounding osteolytic foci
MRI:
- bone marrow edema, periostitis, soft-tissue inflammation, transphyseal disease
- joint effusion (30%), synovial thickening, cartilage destruction, destruction of subchondral bone
Late:
- sclerosis + hyperostosis
Prognosis: delayed spontaneous resolution
DDx: subacute + chronic infectious osteomyelitis; histiocytosis; hypophosphatasia; malignancy (leukemia, lymphoma, Ewing sarcoma)
Brodie Abscess
= small intraosseous abscess involving cortex surrounded by reactive bone (in smoldering indolent infection of subacute pyogenic osteomyelitis / inadequate treatment of acute osteomyelitis)
Organism: S. aureus (most common); cultures often negative
Histo: granulation tissue + eburnation
Age: more common in children; M >F
Location: predilection for ends of tubular bones (proximal / distal tibial metaphysis most common); carpal + tarsal bones
Site: metaphysis, rarely traversing the open growth plate; epiphysis (in children + infants)
- lytic lesion often in an oval configuration that is oriented along the long axis of the bone
- surrounded by thick dense rim of reactive sclerosis that fades imperceptibly into surrounding bone
- lucent tortuous channel extending toward growth plate prior to physeal closure (PATHOGNOMONIC)
- periosteal new-bone formation
- ± adjacent soft-tissue swelling
- may persist for many months
MR:
- “double line” effect = high SI of granulation tissue surrounded by low SI of bone sclerosis on T2WI
- well-defined lesion of low- to intermediate SI outlined by low-signal rim on T1WI
- generally surrounded by marrow edema
- no / rim enhancement after IV Gd-chelate
DDx: Osteoid osteoma
Etiology: complication of chronic osteomyelitis (0.2–1.7%)
Histo: squamous cell carcinoma (90%); occasionally: basal cell carcinoma, adenocarcinoma, fibro-sarcoma, angiosarcoma, reticulum cell sarcoma, spindle cell sarcoma, rhabdomyosarcoma, parosteal osteosarcoma, plasmacytoma
Age: 30–80 (mean 55) years; M >>F
Latent period: 20–30 (range of 1.5–72) years
- history of childhood osteomyelitis
- exacerbation of symptoms with increasing pain, enlarging mass
- change in character / amount of sinus drainage
Location: at site of chronically / intermittently draining sinus; tibia (50%), femur (21%)
- lytic lesion superimposed on changes of chronic osteomyelitis
- soft-tissue mass
- pathologic fracture
Prognosis:
- Early metastases in 14–20–40% (within 18 months)
- No recurrence in 80%
