= sac covered by leptomeninges containing CSF + variable amount of neural tissue; herniated through a defect in the posterior / anterior elements of spine
Prevalence: 1÷1,000–2,000 births (in Great Britain 1÷200 births); twice as common in infants of mothers >35 years of age; Caucasians >Blacks >Orientals; most common congenital anomaly of CNS
Etiology: localized defect of closure of caudal neuropore (usually closed by 28 days); persistence of neural placode causes derangement in the development of mesenchymal + ectodermal structures
- positive family history in 10%
- neural placode = reddish neural tissue in the middle of back made up of open spinal cord
- normal skin / cutaneous abnormality: pigmented nevus, abnormal distribution of hair, skin dimple, angioma, lipoma
- MS-AFP (≥2.5 S.D. over mean) permits detection in 80% (2–5% PPV) if defect not covered by full skin thickness
Recurrence rate: 3–7% chance of NTD with previously affected sibling / in fetus of affected parent
Associated with:
- Hydrocephalus (70–90%): requiring ventriculoperitoneal shunt in 90%
- 25% of patients with hydrocephalus have spina bifida!
- Chiari II malformation (99%)
- Congenital / acquired kyphoscoliosis (90%)
- Vertebral anomalies: vertebral body fusion, hemivertebrae, cleft vertebrae, butterfly vertebrae
- Diastematomyelia (20–46%): spinal cord split above (31%), below (25%), at the same level (22%) as the myelomeningocele
- Duplication of central canal (5%) cephalic to + at level of placode
- Hemimyelocele (10%) = two hemicords in separate dural tubes separated by fibrous / bony spur: one hemicord with myelomeningocele on one side of midline, one hemicord normal / with smaller myelomeningocele at a lower level
- impaired neurological function on side of hemimyelocele
- Hydromyelia (29–77%) cranial to placode ← disturbed CSF circulation
- Chromosomal anomalies (10–17%): trisomy 18, trisomy 13, triploidy, unbalanced translocation
- In 20% no detectable associated anomalies!
- Tethering of spinal cord (70–90%)
- Arachnoid cyst (2%) ← developmental deficiency during formation of arachnoid / dura mater with a subdural location
Distribution: thoracic (2%), thoracolumbar (32%), lumbar (22%), lumbosacral (44%)
Location:
- cranial meningocele = encephalocele
- dorsal / posterior meningocele
- anterior sacral meningocele
- lateral thoracic / lumbar meningocele
OB-US:
- detection rate of 85–90%; sensitivity dependent on GA (fetal spine may be adequately visualized after 16–20 weeks GA); false-negative rate of 24%
- spinal level estimated by counting up from last sacral ossification center = S4 in 2nd trimester + S5 in 3rd trimester (79% accuracy for ± spinal level)
- may have clubfoot / rocker-bottom foot
- polyhydramnios
- Spine:
- loss of dorsal epidermal integrity
- soft-tissue mass protruding posteriorly + visualization of sac
- widening of lumbar spine with fusiform enlargement of spinal canal:
- splaying (= divergent position) of ossification centers of laminae with cup- / wedge-shaped pattern (in transverse plane = most important section for Dx)
- absence of posterior line = posterior vertebral elements (in sagittal plane)
- gross irregularity in parallelism of lines representing laminae of vertebrae (in coronal plane)
- anomalies of segmentation / hemivertebrae (33%) with short-radius kyphoscoliosis
- tethered cord + lumbar / lumbosacral myelomeningocele
- Head:
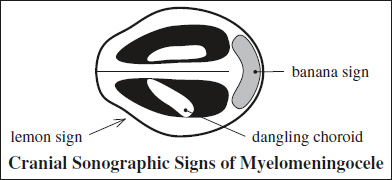
- “lemon” sign = concave / linear frontal contour abnormality located at coronal suture strongly associated with spina bifida
- “banana” sign
Prevalence: in 96% of fetuses ≤24 weeks; in 91% of fetuses >24 weeks - “nonvisualization” of cerebellum
- effaced cisterna magna (100% sensitivity)
- A normal cisterna magna is 3–10 mm deep and usually visualized in 97% at 15–25 weeks GA
- BPD <5th percentile during 2nd trimester (70% sensitive)
- HC <5th percentile (35% sensitivity)
- ventriculomegaly (40–90%) with choroid plexus incompletely filling the ventricles (54–63% sensitivity) = “dangling” choroid on dependent side
Prevalence: in 44% of myelomeningoceles <24 weeks GA; in 94% of myelomeningoceles during 3rd trimester
Plain films:
- bony defect in neural arch
- deformity + failure of fusion of lamina
- absent spinous process
- widened interpedicular distance
- widened spinal canal
Rx:
- Possibly elective cesarean section at 36–38 weeks GA (may decrease risk of contaminating / rupturing the meningomyelocele sac)
- Repair within 48 hr
Postoperative complications:
- Postoperative tethering of spinal cord by placode / scar
- Constricting dural ring
- Cord compression by lipoma / dermoid / epidermoid cyst
- Ischemia from vascular compromise
- Syringohydromyelia
Prognosis:
- Mortality 15% by age 10 years
- Intelligence: IQ <80 (27%); IQ >100 (27%); learning disability (50%)
- Urinary incontinence: 85% achieve social continence (scheduled intermittent catheterization)
- Motor function: some deficit (100%); improvement after repair (37%)
- Hindbrain dysfunction associated with Chiari II malformation (32%)
- ventriculitis: 7% in initial repair within 48 hours, more common in delayed repair >48 hours
Dorsal / Posterior Meningocele
- lumbosacral (70% below L2): may be associated with tethered cord, partial sacral agenesis
- suboccipital
= prolapse through sacral foramen / anterior bony defect
May be associated with:
- neurofibromatosis type 1, Marfan syndrome, partial sacral agenesis, imperforate anus, anal stenosis, tethered spinal cord, GU tract / colonic anomalies; Currarino triad
Prevalence: 1÷40,000
Age: 1st decade of life (in 80%); M÷F = 1÷4
- usually asymptomatic in older children
- constipation, dysmenorrhea, urinary incontinence ← mass effect
- back pain, numbness in lower limbs, headache ← neurologic compromise / meningitis / rupture
- vertebral body scalloping, hypoplasia, aplasia
- scimitar sacrum = sickle-shaped sacrum
= outpouching of leptomeninges through enlarged intervertebral foramen into extrapleural aspect of thorax
Location: right >left side, in 10% bilateral
Often associated with: neurofibromatosis (75–85%) with sharply angled scoliosis convex to meningocele
- expanded spinal canal
- erosion of posterior surface of vertebral body
- thinning of neural arch
- enlarged neural foramen
- spinal abnormalities: kyphoscoliosis, scalloping of dorsal vertebrae, enlargement of intervertebral foramen, pedicle erosion, thinning of ribs
Site: through enlarged neural foramina into subcutaneous tissue / retroperitoneum
Often associated with: Marfan / Ehlers-Danlos syndrome / neurofibromatosis
- expanded spinal canal
- erosion of posterior surface of vertebral body
- thinning of neural arch
- enlarged neural foramen
= avulsion of spinal nerve roots ← tear in meningeal root sheath
Location: (most commonly) in C-spine after brachial plexus injury
- small irregular arachnoid diverticulum with extension outside the spinal canal