Metabolic Syndrome Caused by Cancer Treatment
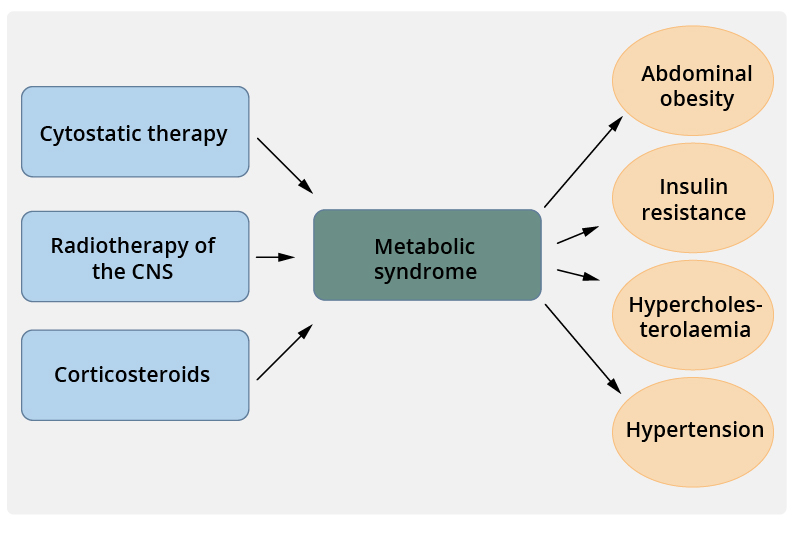
Metabolic syndrome caused by cancer treatment.
Picture: Duodecim Medical Publications Ltd., text: Riikka Nevala
Primary/Secondary Keywords
- cancer
- metabolic syndrome
- lääkehoito
- cancer treatment
- cytotoxic treatment
- radiotherapy
- corticosteroids
- insulin resistance
- hypercholesterolaemia
- hypertension
- abdominal obesity