Steps of Pharmacological and Surgical Treatment of ED
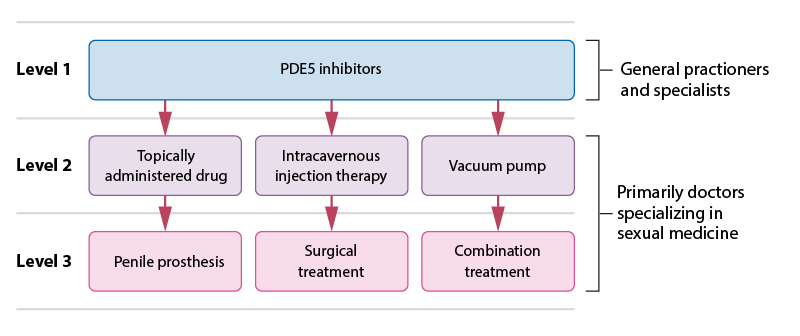
Steps of pharmacological and surgical treatment of ED.
Picture: Piha J. [Steps of pharmacotherapy]. In: Brusila P, Kero K, Piha J et al (eds.). [Sexual Medicine]. Helsinki: Duodecim Publishing Company 2020. Modified from: Hatzimouratidis K, Giuliano F, Moncada I et al. EAU Guidelines on Erectile Dysfunction, Premature Ejaculation, Penile Curvature and Priapism. European Association of Urology 2018.
http://d56bochluxqnz.cloudfront.net/media/EAU-Guidelines-on-Male-Sexual-Dysfunction-2018-large-text.pdfPrimary/Secondary Keywords
- ED
- erectile dysfunction
- medical treatment
- surgical treatment
- PDE5 inhibitor
- alprostadil
- penile prosthesis
- injection therapy
- vacuum pump