Atypical Pneumonia in a Patient with HIV
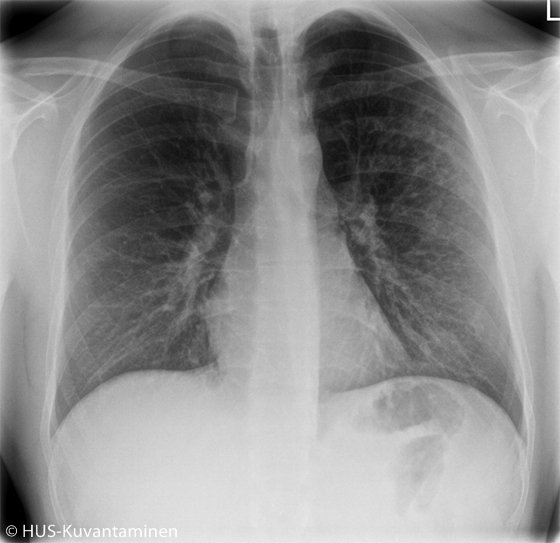
Atypical pneumonia in a patient with HIV (radiograph without markers).
A young man had been coughing and experiencing low-grade fever for 2 weeks. The patient had HIV, which had been managed appropriately. Obstruction was heard in pulmonary auscultation.
Picture: HUS Imaging
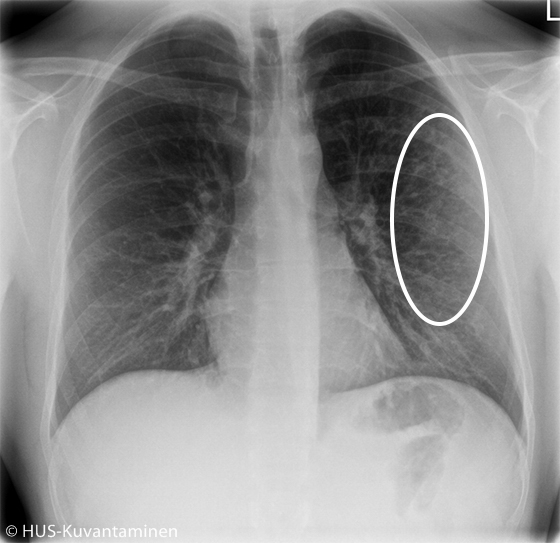
Atypical pneumonia in a patient with HIV (radiograph with markers).
The chest X-ray showed atypical pneumonia. There is diffuse shadowing and increased markings in the distal lung parenchyma (circle).
Picture: HUS Imaging
Primary/Secondary Keywords
- thorax
- chest
- x-ray
- atypical pneumonia
- pneumonia
- HIV