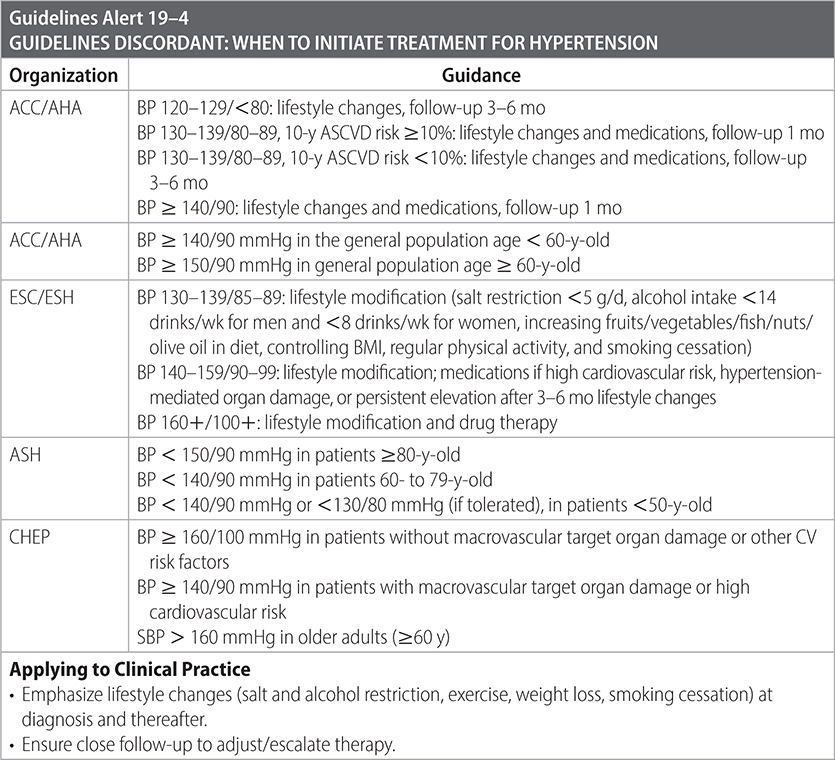
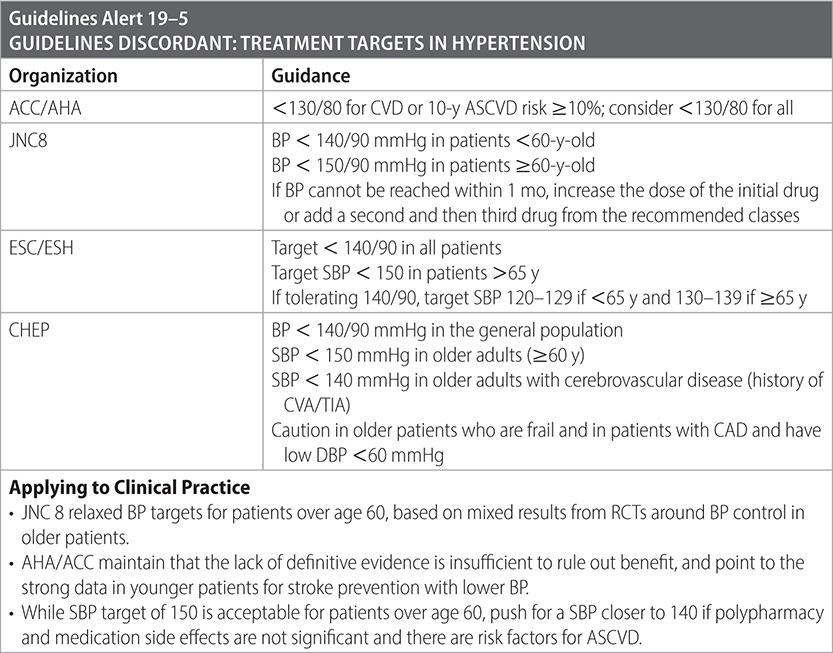
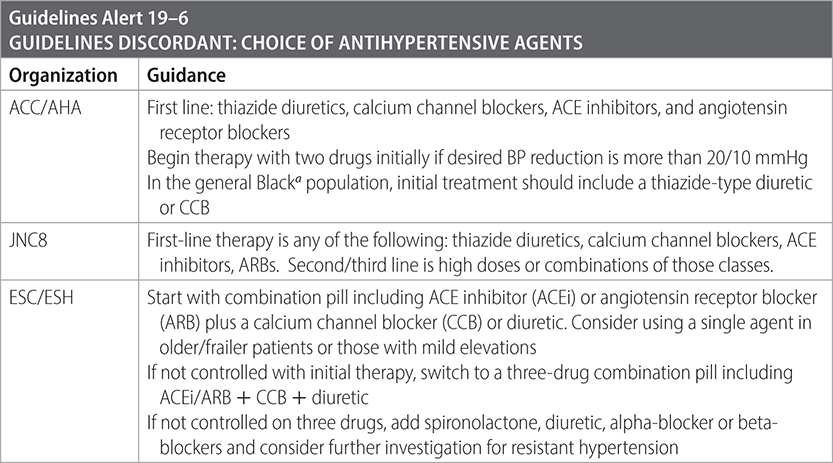
Population: Adults with HTN.
Organizations
 ACC/AHA 2017, JNC8 2014, ESC/ESH 2018, ASH 2014, CHEP 2015
ACC/AHA 2017, JNC8 2014, ESC/ESH 2018, ASH 2014, CHEP 2015
Recommendations
–Initiate lifestyle modification including structured exercise and dietary adjustments including lower sodium diet and efforts at weight loss if overweight or obese. Further measures include weight reduction, DASH/Mediterranean diet, dietary sodium restriction, exercise, moderate ETOH, cessation of smoking, and K+ supplementation in diet.
–Consider overall cardiovascular risk in patients with hypertension and evaluate need for primary prevention measures for ASCVD including smoking cessation, aspirin, and statin.



Sources
–ACC/AHA; Whelton PK et al. JACC. 2018;71(19):e127-e248.
–JNC8. JAMA. 2014;311(5):507-520.
–ESC/EHA: Eur Heart J. 2018;39:3021-3104.
–ASH. J Clin Hypertens. 2014. doi: 10.1111/jch.12237.
–CHEP. Can J Cardiol. 2015;31(5):549-568.
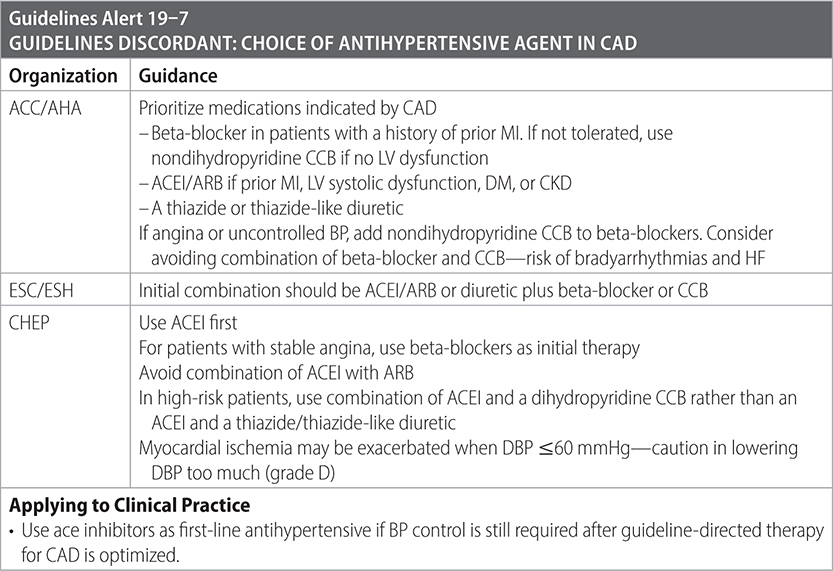
Population: Adults with HTN and CAD.
Organizations
 ACC/AHA 2017, ESC/ESH 2018, CHEP 2014
ACC/AHA 2017, ESC/ESH 2018, CHEP 2014
Recommendations
–Prioritize medications indicated by CAD.
–Treatment target (ACC/AHA):
• <130/80 if CAD, prior MI/stroke/TIA/PAD/AAA.
• <140/90 if chronic stable angina.

Sources
–ACC/AHA; Whelton PK et al. JACC. 2018;71(19):e127-e248.
–ESC/EHA. Eur Heart J. 2018;39:3021-3104.
–CHEP. Can J Cardiol. 2015;31(5):549-568.
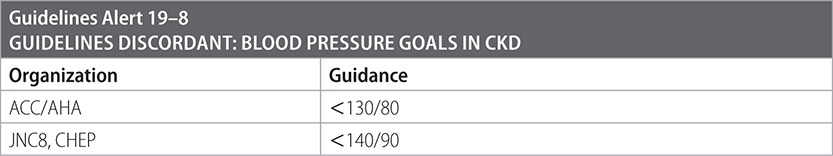
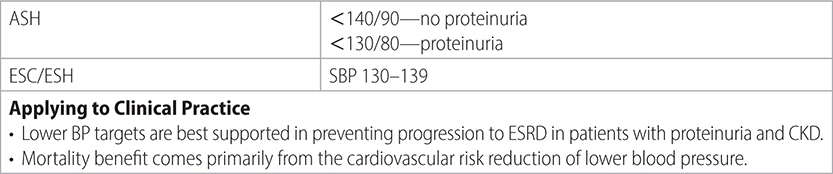
Population: Adults with HTN and CKD.
Organizations
 ACC/AHA 2017, ESC/ESH 2018, CHEP 2014, ASH 2014, JNC8 2014
ACC/AHA 2017, ESC/ESH 2018, CHEP 2014, ASH 2014, JNC8 2014
Recommendations
–Use ACE inhibitor (ACEI) or angiotensin receptor blocker (ARB), particularly if proteinuria.
• Consider starting with ACEI/ARB plus CCB or diuretic as initial therapy. (ESC)
• In patients over 75 y, use CCB and thiazide-type diuretic instead of ACE/ARB. (JNC8)

Sources
–ACC/AHA; Whelton PK et al. JACC. 2018;71(19):e127-e248.
–JNC8. JAMA. 2014;311(5):507-520. doi:10.1001/jama.2013.284427.
–ESC/EHA. Eur Heart J. 2018;39:3021-3104.
–ASH. J Clin Hypertens. 2014. doi: 10.1111/jch.12237.
Population: Adults with HTN and HF.
Recommendations
 ACC/AHA/ASH 2017, CHEP 2014
ACC/AHA/ASH 2017, CHEP 2014
–BP target is <130/80 mmHg, but consideration can be given to lowering the BP even further, to <130/80 mmHg. In patients with an elevated DBP who have CAD and HF with evidence of myocardial ischemia, lower the BP slowly. In older hypertensive individuals with wide pulse pressures, lowering SBP may cause very low DBP values (<60 mmHg).
–If stable ischemic heart disease, prioritize medications indicated by CAD/CHF as first drugs: ACEI/ARB, beta-blocker (carvedilol, metoprolol succinate, bisoprolol, or nebivolol), and aldosterone receptor antagonist.
–Use thiazide/thiazide-type diuretic for BP control and to reverse volume overload and associated symptoms. In patients with severe HF (NYHA III or IV), or those with severe renal impairment (eGFR < 30 mL/min/1.73 m2), use loop diuretics for volume control (less effective than thiazide/thiazide-type diuretics in lowering BP). Use diuretics together with an ACE/ARB and a beta-blocker.
–Use aldosterone receptor antagonists spironolactone and eplerenone if there is HF (NYHA III or IV) with reduced EF <40%. One or the other may be substituted for a thiazide diuretic in patients requiring a K-sparing agent. If used with an ACEI/ARB in the presence of renal insufficiency, monitor serum K level frequently. Do not use if creatinine level ≥2.5 mg/dL in men or ≥2.0 mg/dL in women, or if serum K level ≥5 mEq/L.
–Add hydralazine plus isosorbide dinitrate to the regimen of diuretic, ACE inhibitor, or ARB, and beta-blocker in Black patients with NYHA class III or IV HF with reduced ejection fraction.
–Do not use nondihydropyridine CCBs in the treatment of HTN in adults with HFrEF.
–Preserved ejection fraction: consider beta-adrenergic blocking agents, ACEI/ARBs, or CCB as antihypertensives in patients with HF to minimize symptoms of HF.
–Avoid the following drugs in patients with hypertension and HF with reduced ejection fraction:
• Nondihydropyridine CCBs (such as verapamil and diltiazem).
• Clonidine.
• Moxonidine.
• Hydralazine, without a nitrate.
• Alpha-adrenergic blockers such as doxazosin (unless all other drugs for the management of hypertension and HF are inadequate to achieve BP control at maximum tolerated doses).
• Nonsteroidal anti-inflammatory drugs, given their effects on BP, volume status, and renal function.
Source
–ACC/AHA; Whelton PK et al. JACC. 2018;71(19):e127-e248.
Population: Adults with HTN and diabetes.
Recommendations

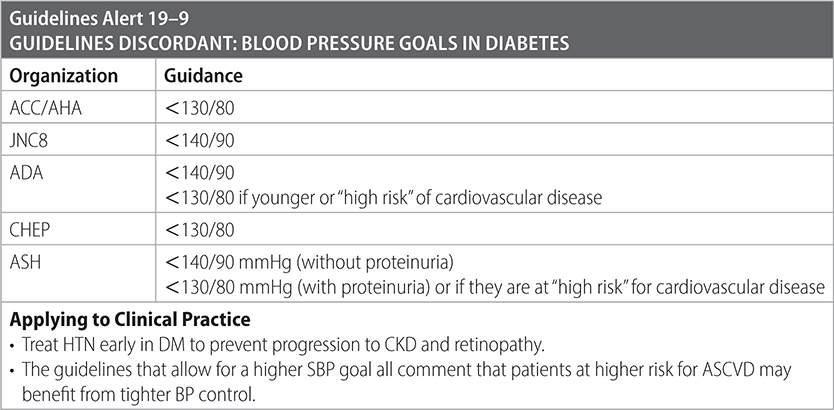

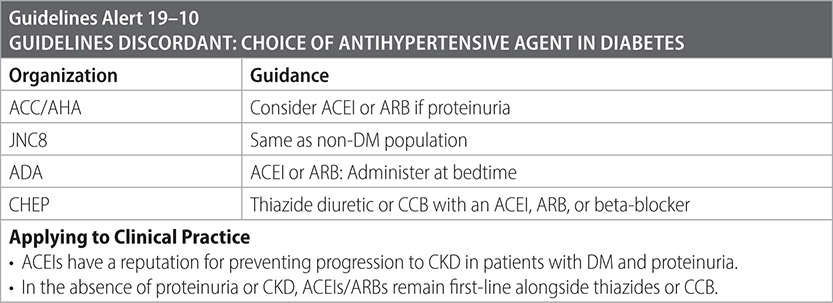
Sources
–Standards of medical care in diabetes. Diabetes Care. 2017;40(suppl 1):S1–S142. (www.care.diabetesjournals.org).
–ACC/AHA; Whelton PK et al. JACC. 2018;71(19):e127-e248.
–JNC8. JAMA. 2014;311(5):507-520.
–CHEP. Can J Cardiol. 2015;31(5):549-568.
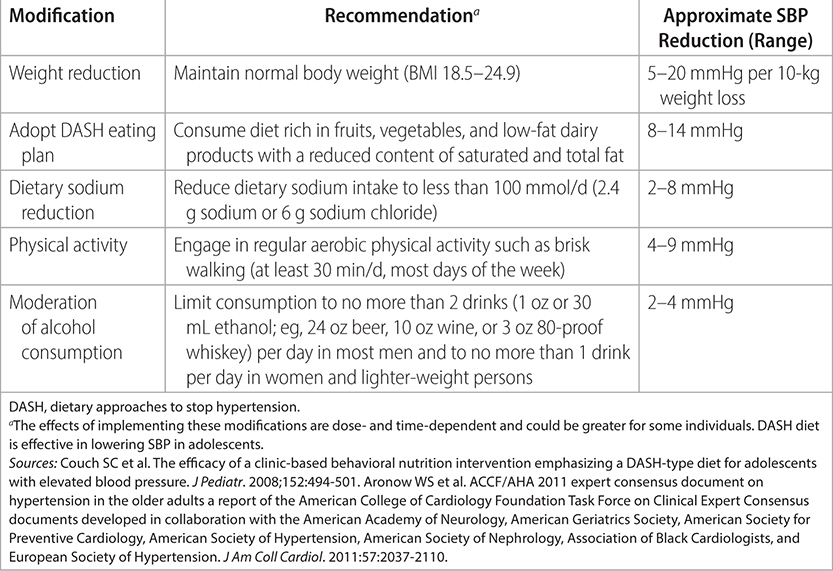
Population: Adults with HTN attempting lifestyle changes.
Recommendation
–See Table 19–10 for the impacts of behavior changes on blood pressure, and Table 19–11 for impacts of specific lifestyle modifications.
TABLE 19–10 IMPACT OF HEALTH BEHAVIOR MANAGEMENT ON BLOOD PRESSURE
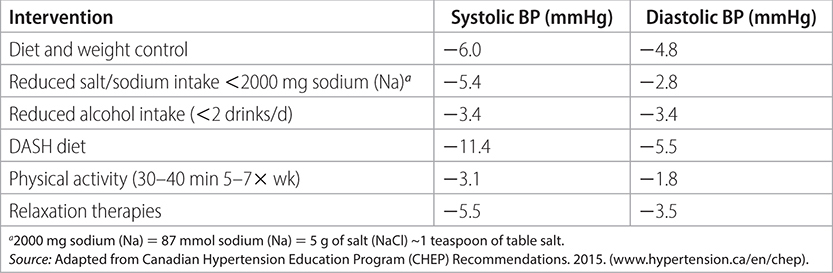
TABLE 19–11 LIFESTYLE MODIFICATIONS FOR TREATMENT OF HYPERTENSION
Population: Adults with refractory hypertension.
Recommendations
–Definition: Failure to reach BP goal (<140/90 mmHg, or 130/80 mmHg in patients with diabetes, heart disease, or chronic kidney disease) using three different antihypertensive drug classes.
–Common causes:
• Nonadherence to drugs/diet.
• Suboptimal therapy/BP measurement (fluid retention, inadequate dosage).
• Diet/drug interactions (caffeine, cocaine, alcohol, nicotine, NSAIDs, steroids, BCP, erythropoietin, natural licorice, herbs).
• Common secondary causes:
 Obstructive sleep apnea.
Obstructive sleep apnea.
 Diabetes.
Diabetes.
 Chronic kidney disease.
Chronic kidney disease.
 Renal artery stenosis.
Renal artery stenosis.
 Obesity.
Obesity.
 Endocrine disorders (primary hyperaldosteronism, hyperthyroidism, hyperparathyroidism, Cushing syndrome), pheochromocytoma.
Endocrine disorders (primary hyperaldosteronism, hyperthyroidism, hyperparathyroidism, Cushing syndrome), pheochromocytoma.
Therapies
–Exclude nonadherence and incorrect BP measurement.
–Review drug and diet history.
–Screen for secondary causes: History of sleep disorders/daytime sleepiness/tachycardias/BPs in both arms; routine labs: sodium, potassium, creatinine, CBC, ECG, urinalysis, blood glucose, cholesterol; additional evaluation: aldosterone: renin ratio, renal ultrasound with Doppler flow study, serum or urine catecholamine levels, morning cortisol level.
–Lifestyle therapy: Weight loss (10-kg weight loss results in a 5–20 mmHg decrease in SBP); diet consult for low sodium (2.3 g daily), high fiber, and high potassium (DASH diet results in an 8–14 mmHg decrease in SBP); exercise aerobic training results in a 4–9 mmHg decrease in SBP; and restriction of excess alcohol (1 oz in men and 0.5 oz in women) results in a 2–4 mmHg decrease in SBP.
–Pharmacologic therapy: Consider volume overload.
–Switch from HCTZ to chlorthalidone (especially if GFR < 40 mL/min/1.73 m2).
–Switch to loop diuretic if GFR < 30 mL/min/1.73 m2 (eg, furosemide 40 mg BID).
–Use CCB (amlodipine or nifedipine) + ACE inhibitor or ARB: Consider catecholamine excess.
–Switch to vasodilating beta-blocker (carvedilol, labetalol, nebivolol): Consider aldosterone excess (even with normal serum K+ level).
–Spironolactone or eplerenone.
–Finally, consider hydralazine or minoxidil.
–If already on beta-blocker, clonidine adds little BP benefit.
–Nonpharmacologic therapy: Still under investigation.
–Carotid baroreceptor stimulation (Hypertension. 2010;55:1-8): May lower BP 33/22 mmHg.
–Renal artery nerve denervation (SYMPLICITY HTN-3) did not show a significant reduction of SBP in patients with resistant hypertension, 6 mo after the procedure.
Sources
–Bhatt DL et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393-1401. Calhoun DA et al.; American Heart Association Professional Education Committee.
–Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510-e526.
–JNC VII. Arch Intern Med. 2003;289:2560-2572.
–European 2007 Guidelines. 2007;28:1462-1536.
–American College of Cardiology/American Heart Association/European Society of Cardiology.
–VA DoD CPG for the Diagnosis and Management of HTN in the Primary Care Setting. https://www.healthquality.va.gov/guidelines/CD/htn/.
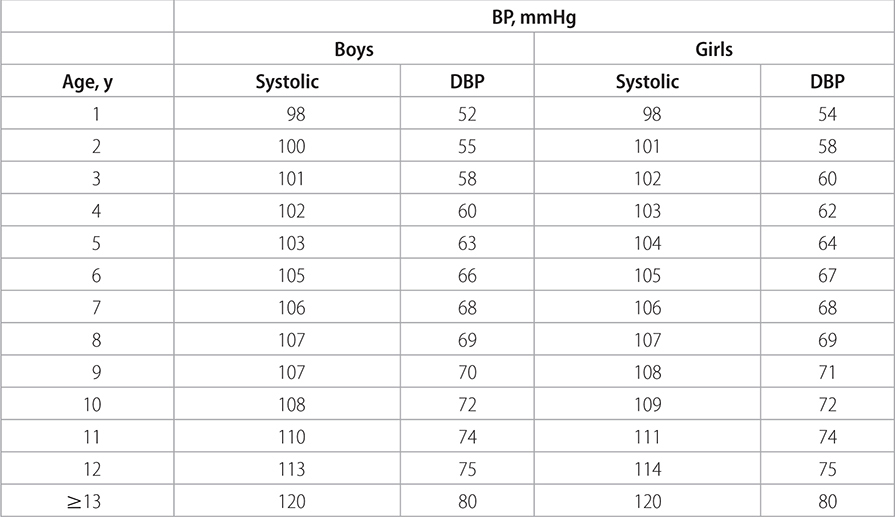
Population: Children and adolescents with hypertension.
Recommendations
–The current definition of HTN in children and adolescents is based on the normative distribution per above; “normal BP” was initially defined as SBP and DBP values <90th percentile (on the basis of age, sex, and height percentiles). See Table 19–12 for age-stratified cutoffs.
–For adolescents, “prehypertension” is BP >120/80 mmHg to <95th percentile or >90th and <95th percentile.
–Indications for antihypertensive therapy in children and adolescents:
• Symptomatic hypertension.
• Secondary hypertension.
• Hypertensive target organ damage.
• Diabetes (types 1 and 2).
• Persistent hypertension despite nonpharmacologic measures (weight management counseling if overweight; physical activity; diet management).
Sources
–Pediatrics. 2011;128(5):S213-S258.
–Kavey RE et al.; American Heart Association Expert Panel on Population and Prevention Science; American Heart Association Council on Cardiovascular Disease in the Young; American Heart Association Council on Epidemiology and Prevention, et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation. 2006;114:2710-2738.
TABLE 19–12 SCREENING BP VALUES REQUIRING FURTHER EVALUATION