Population: Adults with low-back pain.
Organizations
 ACP 2020, NICE 2020, ICSI 2018, ACR 2021
ACP 2020, NICE 2020, ICSI 2018, ACR 2021
Recommendations
–Exclude other specific causes of back pain, eg, cancer, infection, trauma, inflammatory disease.
–Consider various nonpharmacologic treatments for acute or subacute low-back pain including superficial heat, massage, exercise program, acupuncture, and spinal manipulation.
–For chronic low-back pain, start a trial of nonpharmacologic treatments including exercise, multidisciplinary rehabilitation, acupuncture, mindfulness-based stress reduction, tai chi, yoga, biofeedback, cognitive behavioral therapy, or spinal manipulation.
–Consider behavioral health referral for patients with a high disability and/or who experience significant psychological distress from their low-back pain.
–If pharmacologic treatments are needed, offer NSAIDs (topical or oral) or oral acetaminophen or skeletal muscle relaxants in the lowest effective dose for shortest period of time.
–Obtain imaging in the following situations: persistent or progressive symptoms after 6 wk of optimal medical management; history of prior lumbar surgery with new or worsening symptoms; presence of red flag symptoms.

–Consider epidural steroid injections as an adjunct for acute and subacute low-back pain with a radicular component. (ICSI)
–Avoid routine imaging (x-ray, CT, MRI) in patients with nonspecific or radicular low-back pain without red flag symptoms.
–Do not offer SSRI, SNRI, tricyclic antidepressants, or anticonvulsants for management of low-back pain. (NICE)
–Do not offer spinal fusion for low-back pain. (NICE)
–Do not offer orthotics such as belts, corsets, foot orthotics for low-back pain. (NICE)
Practice Pearls
• Exercise guided by a physical therapist produces the best long-term results (NNT 7 for pain relief). NSAIDs are also effective (NNT=6). Duloxetine (NNT=10) and opioids (NNT=16) have benefits but also significant side-effect profiles. Other interventions do not show consistent long-term benefit. (Can Fam Physician. 2021;67(1):e20–e30)
• When using pharmacologic therapy, consider and counsel the patients on potential side effects.
• While the guidelines recommend them, muscle relaxants do not improve functional outcomes or pain (Ann Emerg Med. 2019;74(4):512-520). If they are used, limit duration to <1 wk.
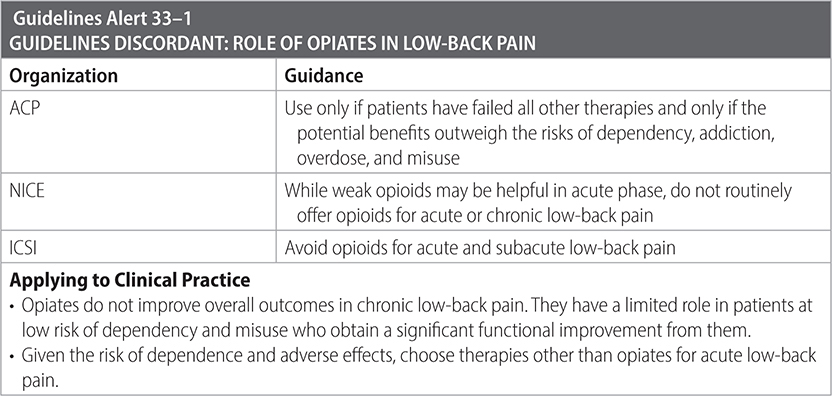
• When using opiates, restrict duration to 7 d or less.
• Topical NSAIDs with or without menthol gel were the most effective first-line therapy.
• Epidural injections provide a small amount of immediate improvement in both back and leg pain and functional ability, but the benefits were no longer measurable after 2 wk according to a Cochrane review. (Spine. 2020;45(21):e1405-e1415)
• Patients knowingly given placebo report improved pain and function. (Pain. 2019;160(12):2891-2897)
• In the absence of red flag symptoms, immediate lumbar imaging does not improve clinical outcomes compared to those who received usual care. Imaging should be reserved for patients for whom noninvasive, conservative regimens have failed and surgery and/or injections are being considered. (Lancet. 2009; 373(9662):463-472)
Sources
–Ann Intern Med. 2017;166(7):514-530.
–Ann Internal Med. 2020;173(9).
–Lancet. 2009;373:463-472.
–NICE practice guidelines: Low Back Pain; www.pathways.nice.org.uk/pathways/low-back-pain-and-sciatica/managing-low-back-pain-and-sciatica
–ICSI. Adult Acute and Subacute Low Back Pain. March 2018.
–ACR. ACR Appropriateness Criteria: Low Back Pain. 2021.